Abstract
Backgrounds/Aims
Elderly patients aged >80 yr have high morbidity and mortality rates after biliary surgery, especially in emergency operations. We conducted this study to determine the effect of preoperative management on the outcome of elderly patients undergoing cholecystectomy.
Methods
The medical records of 452 elderly (≥80 yr old) patients who underwent cholecystectomy from January 1997 to December 2015 were reviewed retrospectively. We divided the patients into 2 groups: intervention (preoperative biliary drainage) and non-intervention groups. We evaluated the effects of preoperative management on the American Society of Anesthesiology (ASA) score and perioperative outcomes.
Results
Among the preoperative biliary drainage intervention group (n=286), 48 patients (51.7%) were diagnosed as having gallbladder stone combined with common bile duct stone. On admission, the proportion of patients with ASA score ≥3 and WBC counts were significantly higher in the intervention group than in the non-intervention group (p<0.05). The preoperative hospital stay was longer in the intervention group; however, operation-related factors such as operation type, time, conversion rate, complications, and mortality showed no difference between groups.
The prevalence of cholelithiasis increases with age, and among patients aged ≥80 yr, prevalence rates as high as 38% to 53% have been reported.1,2 Biliary tract disease is the single most common cause of acute abdominal complaints and accounts for approximately one-third of all abdominal operations in the elderly.3 An increased incidence of common bile duct (CBD) stones is also associated with advanced age.4 Elderly patients frequently have significant comorbid diseases and limited functional reserve, which may increase the perioperative mortality rate from 1.5% in patients with no concomitant diseases to 6.1% in patients with >3 additional conditions.5 Emergency cholecystectomy without proper preoperative management of comorbidities and acute inflammation also significantly increases the mortality rate from 2% to 10%.6,7 At our institution, most elderly patients with gallstones undergo elective cholecystectomy after a thorough preoperative evaluation and management of comorbid disease and CBD stones, as a means of reducing perioperative complication and mortality. We apply the American Society of Anesthesiologists (ASA) score for evaluating the preoperative health of elderly surgical candidates before the operation. It is known that the ASA score has a strong association with postoperative morbidity and mortality.8 We conducted this study to know how much preoperative management affects the outcome of elderly patients undergoing cholecystectomy.
A total of 452 patients age >80 yr who underwent cholecystectomy for biliary tract disease from January 1997 to December 2015 were included in the study. Patients who underwent incidental cholecystectomy were excluded.
Information obtained from database and hospital records were used to gather the patients' demographic details. Preoperative, operative, and postoperative data were collected through a review of case notes. These data included level of urgency on admission, location of biliary stones based on clinical and radiologic assessments, preoperative comorbidities and managements, changes in ASA score and leukocyte counts between the time of admission and before the operation, type of operation according to urgency and operation method, need for conversion to an open procedure, and postoperative complications.
Preoperative assessments for biliary stones included abdominal ultrasonography (US), CT, and/or magnetic resonance cholangiography (MRC) for hypersensitive patients. Preoperative endoscopic retrograde cholangiopancreatography (ERCP) and consequent endoscopic nasobiliary drainage (ENBD) were performed in patients suspected to have CBD stones or other bile duct etiologies based on imaging evaluations and liver function tests. Patients with acute cholecystitis but not responding to antibiotics underwent percutaneous cholecystostomy (PTGBD) to reduce inflammation and improve surgical performance. Percutaneous transhepatic biliary drainage (PTBD) was performed in patients who were unable to go through ERCP due to previous operation history such as gastrectomy and unstable vital sign. Cardiopulmonary workups including echocardiography, thallium scan, and pulmonary function test (PFT) were performed before the operation, with echocardiography and PFT being mandatory for all patients. Routine intraoperative cholangiography was not applied. Clinical assessment was performed by the attending surgeon and, when necessary, the attending anesthetist. Specific outcomes were assessed in terms of any change in the patients' urgency and ASA score between admission and operation day, as well as differences in outcomes according to preoperative biliary drainage.
Statistical analysis was performed using SPSS for Windows release 11.0.0 (SPSS, Chicago, IL, USA). Differences between groups were determined using χ2 and Fisher's exact test for categorical variables. Continuous variables were expressed as mean±SD, and comparisons between means were done using Student's t-test. A p-value of <0.05 was considered significant.
This study was approved by the institutional review board in Asan Medical Center (2018-0032).
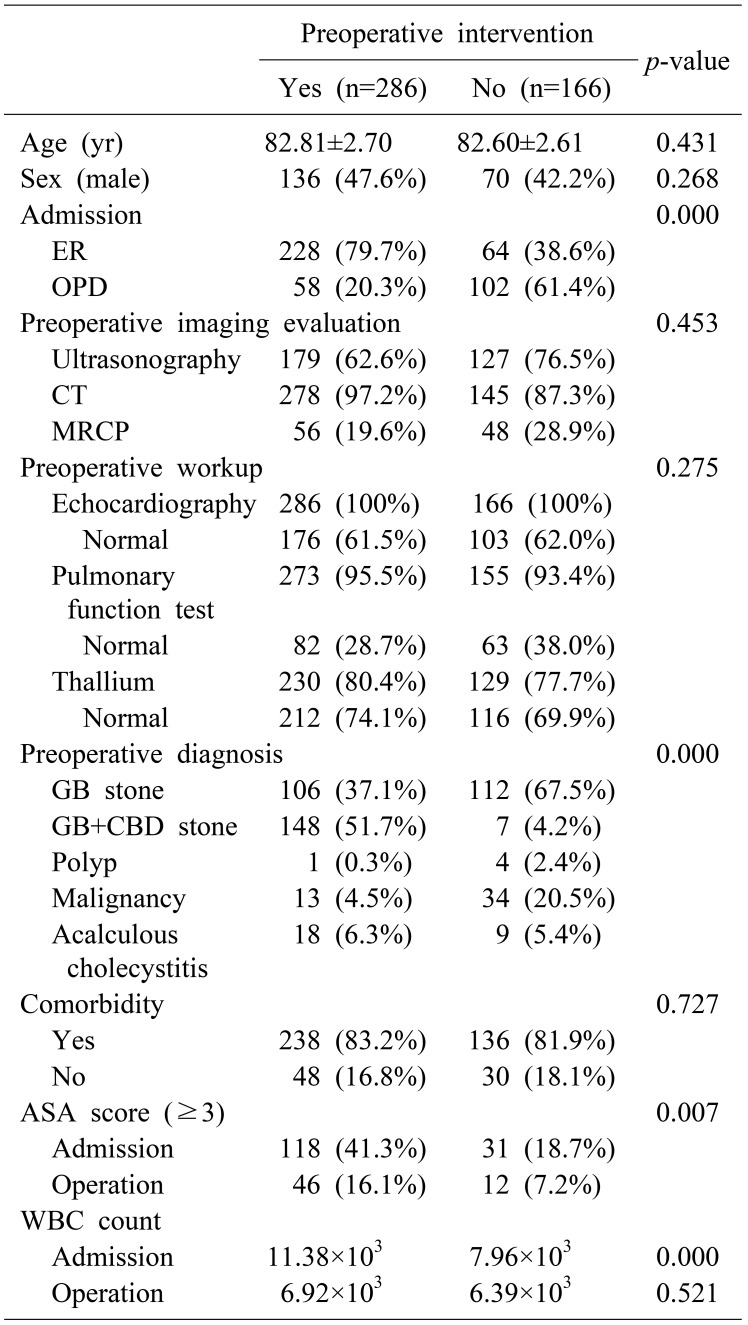
The demographic characteristics of the patients are shown in Table 1. The mean patient age was 82.81±2.70 yr and 82.60±2.61 yr in the intervention (preoperative biliary drainage) and non-intervention groups, respectively (p=0.431). The proportion of male patients was 47.6% (n=136) and 42.2% (n=70) each in the 2 groups (p=0.268). There were 228 (79.7%) and 64 (38.6%) patients who were admitted to the hospital via the emergency department in the intervention and non-intervention groups, respectively (p=0.000). The diagnostic process of preoperative imaging evaluation and cardiopulmonary workup showed no significant difference between the 2 groups (p=0.453 and p=0.275).
Preoperative diagnosis showed statistical differences between the 2 groups (Table 1). A total of 148 (51.7%) patients in the intervention group had gallbladder and CBD stones combined, and 7 (4.2%) patients in the non-intervention group had gallbladder stone with CBD stone (p=0.000). There were 118 (41.3%) patients in the intervention group and 31 (18.7%) patients the in non-intervention group (p=0.007) who had ASA score >3. WBC counts were significantly higher in the intervention group (11.38×103) than in the non-intervention group (7.96×103) on admission (p=0.000). However, there was no statistical difference in WBC count between the 2 groups at the time of the operation.
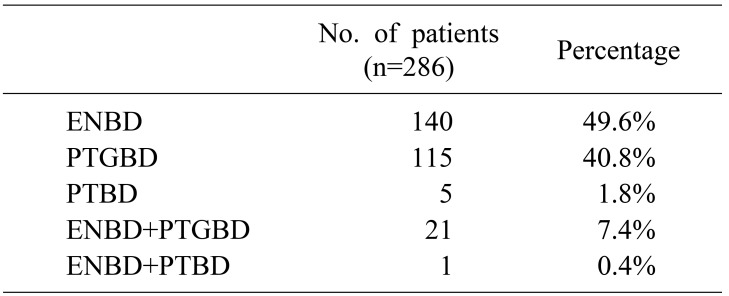
Within the intervention group, endoscopic nasobiliary drainage tube insertion was performed in 162 patients (57.4%) and percutaneous transhepatic gallbladder drainage tube insertion in 115 (48.2%) patients preoperatively (Table 2).
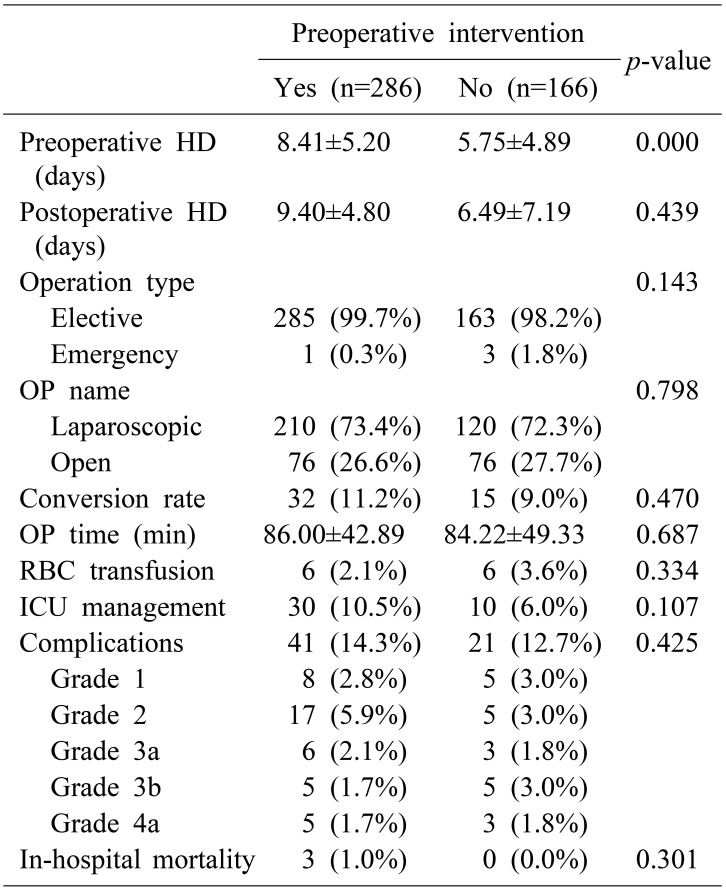
The postoperative outcomes are shown in Table 3. The preoperative hospital stay duration was longer in the intervention group than in the non-intervention group (8.41±5.20 vs. 5.75±4.89 days, p=0.000); however, the postoperative hospital stay duration was not statistically different between the 2 groups (9.40±4.80 vs. 6.49±7.19 days, p=0.439). A total of 285 (99.7%) patients in the intervention group and 163 (98.2%) patients in the non-intervention group underwent elective surgery (p=0.140). Only 1 (0.3%) patient in the intervention group and 3 (1.8%) patients in the non-intervention group underwent emergency surgery. Laparoscopic cholecystectomy was performed in 210 (73.4%) patients in the intervention group and 120 (72.3%) patients in the non-intervention group (p=0.798). The conversion rate was 11.2% (n=32) in the intervention group and 9.0% (n=15) in the non-intervention group, with no statistical significance (p=0.470). Postoperative intensive care unit (ICU) management was needed in 30 (10.5%) patients in the intervention group and 10 (6.0%) patients in the non-intervention group (p=0.107). There was no statistical difference in RBC transfusion and operation time between the 2 groups. We classified the surgical complications according to the Clavien-Dindo classification.9 The number of patients who required interventional treatment was 11 (3.8%) in the intervention group and 8 (4.8%) in the non-intervention group (p=0.425). There were 3 cases of in-hospital mortality involving patients in the intervention group.
The population of Korea has increased significantly over the past few generations, mostly as a result of decreased mortality due to medical and public health interventions accompanied by increased income. According Mathers et al.10 by 2011, the life expectancy of persons aged 80 yr in a high-income country was 8.7 yr for men and 11.0 yr for women, compared with 6.2 yr for men and 7.7 yr for women in 1980.
As the number of geriatric patients increases, it becomes increasingly important for every surgeon to have a clear understanding of factors that influence the life expectancy of elderly patients.11 Particularly, a hepatobiliary surgeon should know well about such factors because biliary tract disease is the single most common cause of acute abdominal complaints and accounts for approximately one-third of all abdominal operations in the elderly population.12 Elderly patients could be challenging to treat because they present with vague symptoms that are difficult to distinguish from other abdominal etiologies, often require open abdominal surgery, and nearly two-thirds of them are admitted to the hospital in an emergency setting. In these circumstances, the existence of comorbid diseases and the decision to perform emergency operation are closely related to the mortality rate.13 Meanwhile, CBD stones are often accompanied by gallstone diseases and an additional choledocholithotomy procedure during the operation significantly increases the incidence of complications. However, nowadays, endoscopic removal of CBD stones can be performed in >90% of relevant cases.14
There are 2 important factors affecting the mortality of elderly patients undergoing cholecystectomy. One is comorbid disease and the other is limited functional reserve.15 Therefore, we attempted to correct these factors preoperatively to reduce mortality and complications after cholecystectomy.
At our institute, when managing geriatric patients with gallbladder disease, we first attempt to assess for the presence of CBD stones through imaging evaluations (US, CT scan, ERCP, and MRC), and we also assess the patient's baseline cardiopulmonary function. If the patient has a CBD stone or severe inflammation, we attempt to perform endoscopic treatment and/or percutaneous drainage first. After resolving such problems, we perform an elective operation rather than an emergency operation.
It is well known that the ASA score, which helps in evaluating the preoperative risk, is an effective method to predict the postoperative morbidity and mortality of geriatric patients.8,16,17,18 We used the ASA score to compare a patient's medical status before and after the interventional treatment. The proportion of patients with ASA score ≥3 in the intervention (preoperative biliary drainage) group was 41.3%. After the preoperative interventional treatment, the proportion of those patients declined to 16.1% at the time of the operation. Although patients in the intervention group tended to have higher ASA scores on admission, postoperative outcomes such as complication and mortality rates were not statistically different between the 2 groups. It was notable that the ASA score of the non-intervention group decreased before the operation compared with that on admission. This is because even without preoperative biliary drainage, conservative treatment such as administration of antibiotics and analgesics helped relieve the patients' symptoms and aided their recovery from physical derangement.
The operation type, conversion rate, and ICU stay did not show statistical differences between the intervention and non-intervention groups. The most common reason for conversion to open cholecystectomy (n=32, 11.2%) was severe adhesion (n=29) after upper abdominal surgery in the intervention group. The rate and main cause of conversion operation were similar between the 2 groups (p=0.470). Postoperative ICU management was needed in 30 (10.5%) and 10 (6.0%) patients in the intervention and non-intervention groups, respectively. A total of 3 patients (1.1%) in the intervention group died within 3 mo after the operation. The causes of death were acute kidney injury, aspiration pneumonia, and sepsis combined with mesenteric infarct, respectively. According to Nielsen et al.,19 patients aged ≥80 yr who underwent cholecystectomy, mortality rate after surgery was 6.3%. It is notable that our study showed significantly lower rate of mortality compared to other studies. In addition, since intervention group and non-intervention group's mortality rate showed no statistical difference (p=0.301), cholecystectomy can be considered as a safe treatment option for intervention group patients without additional risk for mortality.
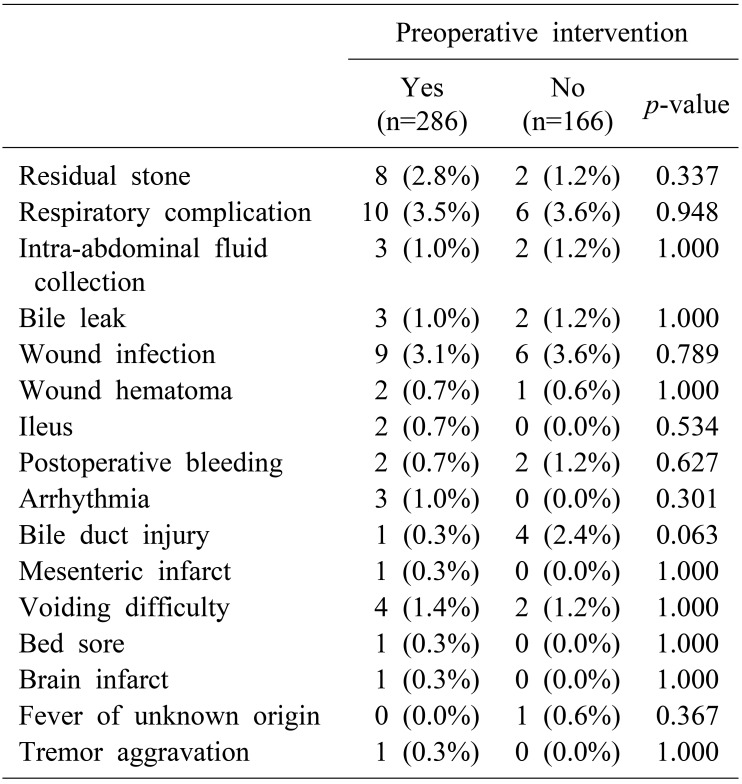
The most common postoperative complications were respiratory complications, wound infection, and residual stone, in that order (Table 4). We compared the complications between the intervention and non-intervention groups, and each of the complications showed no statistical difference between the 2 groups. It is noteworthy that the complication rate in patients in the intervention group who underwent surgery was similar to that of the non-intervention group, which is opposite to the common notion that patients who need intervention will have more complications owing to their higher disease severity. This guarantees that the surgery is safe without conferring a higher risk of complications after the intervention.
However, this study has a few limitations. First, this study has a retrospective design. Second, as the results of this study only convey the outcomes of patients who underwent surgery, patients with gallbladder disease who only received conservative treatment without surgery were not included, which confers the possibility of a selection bias.
In conclusion, proper preoperative evaluations and preoperative biliary drainage allow reductions in the ASA score, making surgery a safe treatment option for elderly patients needing a cholecystectomy.
References
1. Festi D, Dormi A, Capodicasa S, Staniscia T, Attili AF, Loria P, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008; 14:5282–5289. PMID: 18785280.

2. Tambyraja AL, Kumar S, Nixon SJ. Outcome of laparoscopic cholecystectomy in patients 80 years and older. World J Surg. 2004; 28:745–748. PMID: 15457351.

3. Kauvar DS, Brown BD, Braswell AW, Harnisch M. Laparoscopic cholecystectomy in the elderly: increased operative complications and conversions to laparotomy. J Laparoendosc Adv Surg Tech A. 2005; 15:379–382. PMID: 16108740.

4. Borzellino G, de Manzoni G, Ricci F, Castaldini G, Guglielmi A, Cordiano C. Emergency cholecystostomy and subsequent cholecystectomy for acute gallstone cholecystitis in the elderly. Br J Surg. 1999; 86:1521–1525. PMID: 10594498.

5. Yetkin G, Uludag M, Oba S, Citgez B, Paksoy I. Laparoscopic cholecystectomy in elderly patients. JSLS. 2009; 13:587–591. PMID: 20202402.

6. Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ. Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc. 2001; 15:700–705. PMID: 11591971.

7. Csikesz N, Ricciardi R, Tseng JF, Shah SA. Current status of surgical management of acute cholecystitis in the United States. World J Surg. 2008; 32:2230–2236. PMID: 18668287.

8. Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015; 18:184–190. PMID: 25937154.

9. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
10. Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet. 2015; 385:540–548. PMID: 25468166.

11. Riall TS, Zhang D, Townsend CM Jr, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010; 210:668–677. 677–679. PMID: 20421027.

12. Fuks D, Duhaut P, Mauvais F, Pocard M, Haccart V, Paquet JC, et al. A retrospective comparison of older and younger adults undergoing early laparoscopic cholecystectomy for mild to moderate calculous cholecystitis. J Am Geriatr Soc. 2015; 63:1010–1016. PMID: 25946647.

13. Strasberg SM. Clinical practice. Acute calculous cholecystitis. N Engl J Med. 2008; 358:2804–2811. PMID: 18579815.
14. Lee HM, Min SK, Lee HK. Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann Surg Treat Res. 2014; 86:1–6. PMID: 24761400.

15. Tzeng CW, Cooper AB, Vauthey JN, Curley SA, Aloia TA. Predictors of morbidity and mortality after hepatectomy in elderly patients: analysis of 7621 NSQIP patients. HPB (Oxford). 2014; 16:459–468. PMID: 24033514.

16. Shahir MA, Lemmens VE, van de Poll-Franse LV, Voogd AC, Martijn H, Janssen-Heijnen ML. Elderly patients with rectal cancer have a higher risk of treatment-related complications and a poorer prognosis than younger patients: a population-based study. Eur J Cancer. 2006; 42:3015–3021. PMID: 16797967.

17. Ranta S, Hynynen M, Tammisto T. A survey of the ASA physical status classification: significant variation in allocation among Finnish anaesthesiologists. Acta Anaesthesiol Scand. 1997; 41:629–632. PMID: 9181166.

18. Haynes SR, Lawler PG. An assessment of the consistency of ASA physical status classification allocation. Anaesthesia. 1995; 50:195–199. PMID: 7717481.

19. Nielsen LB, Harboe KM, Bardram L. Cholecystectomy for the elderly: no hesitation for otherwise healthy patients. Surg Endosc. 2014; 28:171–177. PMID: 23996332.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download