INTRODUCTION
In Korea, a 20-bed pediatric intensive care unit (PICU) was first established in 1985 at the Seoul National University Children's Hospital. In 2000, the first pediatric critical care (PCC) specialist degree was conferred. In 2011, Assembly of Korean Pediatric Critical Care Medicine was initiated. In 2016, The Korean Society of Pediatric Critical Care Medicine (KSPCCM) was established.
Most of the pediatricians are aware of the need for PICU and pediatric intensivists in PCC in Korea. However, there is a lack of objective data on this subject. Therefore, it is necessary to investigate whether there is an actual shortage of PICUs and PCC.
The aim of this study was to identify the current status of PCC in Korea and to obtain objective data on the subject. PICU bed numbers, infrastructure, medical staff numbers, and the children admitted to PICUs in Korea were evaluated. Based on the results of this research, it is necessary to recognize the lack of PCC in the short-term and to develop a long-term plan at the national level.
METHODS
The KSPCCM directed a questionnaire survey from March to August 2015. Two types of questionnaires were used in this survey. Thirty-two out of the 43 Upper Grade General Hospitals responded to the first questionnaire survey. The questionnaire contained questions to assess the medical staff and facilities in PCC. Data on the number of hospital beds, the number of pediatric beds, the percentage of pediatric beds, the presence of PICU, the type of PICU, and the number of beds in PICU was collected through this questionnaire. Eighteen out of the 43 Upper Grade General Hospitals responded to the second questionnaire survey. The questionnaire contained questions on the infrastructure and patient data of a PICU. The infrastructure included mechanical ventilator and noninvasive ventilator. Patient data included age, sex, reason for admission, the Pediatric Risk of Mortality (PRISM) score 24, patients who were hospitalized within the last one month and who expired within 24 hours from the start of the survey, the place where they had been transferred from, the department responsible for the patients, length of stay, mental status changes, whether patients were placed on mechanical ventilation, central venous catheters, infusion of continuous intravenous vasoactive medications or sedative agents, nutritional support, and whether patients had terminal illness or organ failure. Patient data were collected retrospectively from a chart review. Patients' organ failure was judged by PCC intensivists subjectively.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board (IRB) Seoul St. Mary's Hospital, the Catholic University of Korea, Seoul, Korea (approval No. KC18QEDI0372). Informed consent was waived by the IRB because the study was retrospective.
RESULTS
PICU characteristics
Beds
The mean number of hospital beds in 32 Upper Grade General Hospitals which responded to the first questionnaire survey was 1,069 ± 456 (range, 550–2,700), and the mean number of pediatric beds was 117 ± 89 (range, 22–403). The proportion of pediatric beds in total beds was 10.5% (3.1%–30.4%).
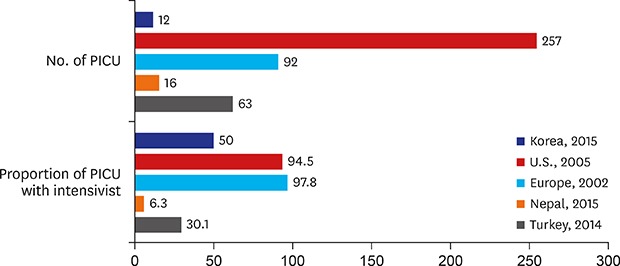
Twelve of the 32 Upper Grade General Hospitals had a total of 13 PICUs. One hospital had both a separate general PICU and a cardiac PICU. Among the 13 PICUs, 12 were used solely by children and infants and one was used by children and adults. The mean number and total number of PICU beds were 9.4 ± 9.3 (range, 2–30) and 113, respectively.
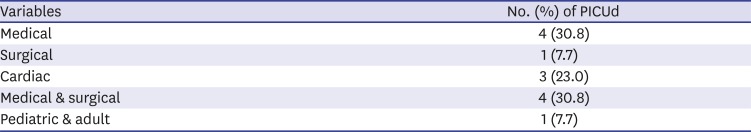
These PICUs were categorized into five categories according to the characteristics of the patients. There were 4 medical PICUs, 1 surgical PICU, 3 cardiac PICUs, 4 medical/surgical PICUs, and 1 PICU that shared an area with adults (
Table 1).
Table 1
Types of PICUs (n = 13)
|
Variables |
No. (%) of PICUd |
|
Medical |
4 (30.8) |
|
Surgical |
1 (7.7) |
|
Cardiac |
3 (23.0) |
|
Medical & surgical |
4 (30.8) |
|
Pediatric & adult |
1 (7.7) |
Specialists
Among the 32 Upper Grade General Hospitals, there were 28 medical doctors responsible for PCC in 16 Upper Grade General Hospitals. Among these 28 doctors, 18 were pediatricians, 8 were thoracic surgeons, one was a pediatric surgeon, and the other was an adult respiratory medicine specialist. Of these 28 doctors, only five doctors were assigned solely to the PICU, while the remaining 23 doctors were in charge of the PICU, as well as additional outpatient care, general wards, and surgery.
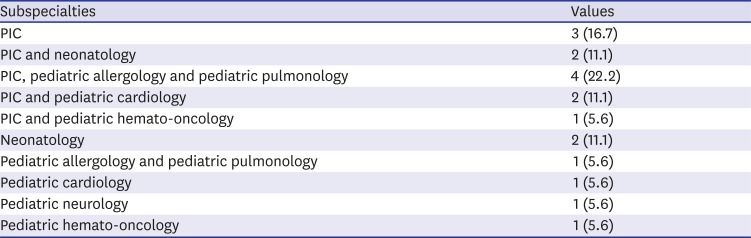
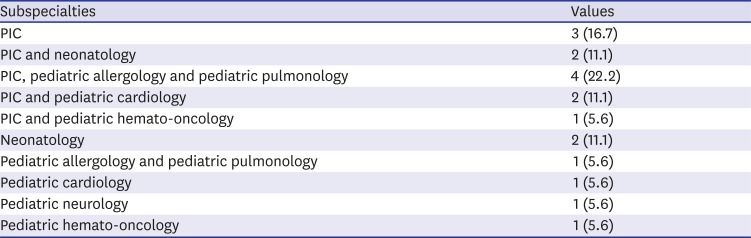
Among these 18 pediatric specialists, there 3 pediatric critical care medicine (PCCM) specialists, 2 PCCM and neonatology specialists, 4 PCCM and pediatric allergy and respiration specialists, 2 PCCM and pediatric cardiology specialists, 1 PCCM and pediatric hemato-oncology specialists, 2 neonatology specialists, 1 pediatric allergy and respiration specialist, 1 pediatric cardiology specialist, 1 pediatric neurology specialist, and 1 pediatric hemato-oncology specialist (
Table 2).
Table 2
Subspecialties of PCC physicians (n = 18)
|
Subspecialties |
Values |
|
PIC |
3 (16.7) |
|
PIC and neonatology |
2 (11.1) |
|
PIC, pediatric allergology and pediatric pulmonology |
4 (22.2) |
|
PIC and pediatric cardiology |
2 (11.1) |
|
PIC and pediatric hemato-oncology |
1 (5.6) |
|
Neonatology |
2 (11.1) |
|
Pediatric allergology and pediatric pulmonology |
1 (5.6) |
|
Pediatric cardiology |
1 (5.6) |
|
Pediatric neurology |
1 (5.6) |
|
Pediatric hemato-oncology |
1 (5.6) |
Nurses
A total of 239 nurses were exclusively assigned to provide PCC in the 18 Upper Grade General Hospitals that responded to the second questionnaire survey, with an average number of 13.3 ± 18.4 (range, 0–52). The ratio of total PCC nurses to PICU beds was 2.1:1. And the ratio of total PCC nurses to pediatric patients was 2.5:1 on the day the survey was conducted.
Infrastructure of PICUs
There were a total of 200 mechanical ventilators and 58 noninvasive ventilators in the 18 Upper Grade General Hospitals that responded to the second questionnaire survey. The mean number of mechanical ventilators and noninvasive ventilators was 11.1 ± 8.6 (range, 0–27) and 3.2 ± 3.1 (range, 0–10), respectively.
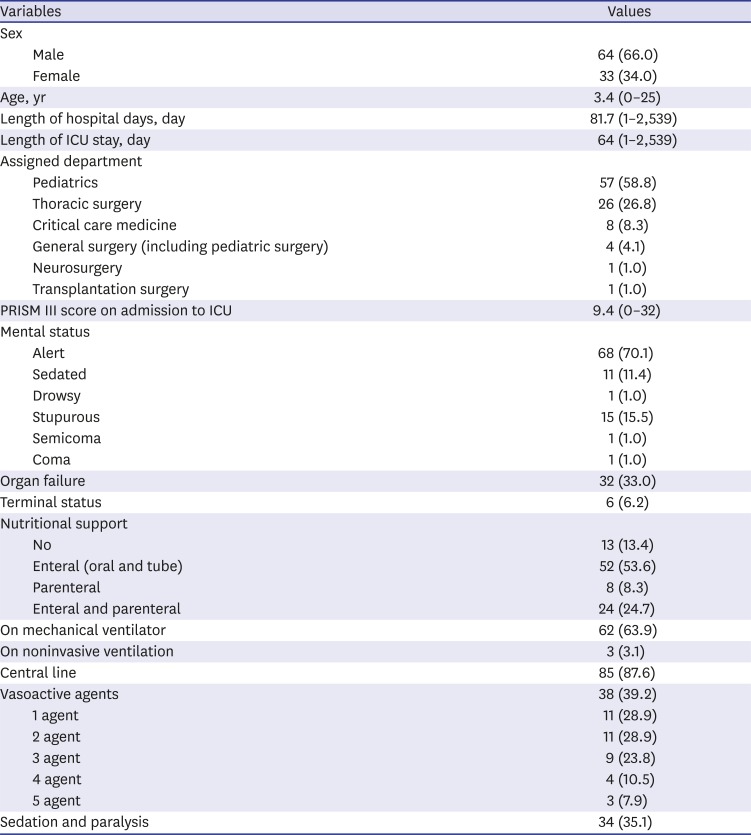
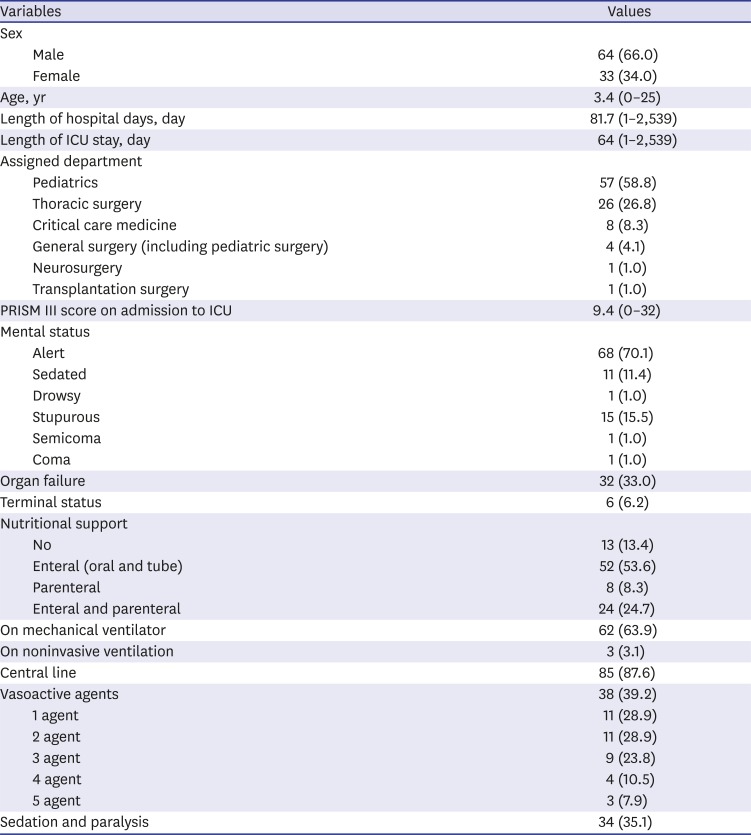
Patient characteristics
In the 18 Upper Grade General Hospitals that responded to the second questionnaire survey, 370 patients were newly admitted to the PICUs within one month from the start of the survey and the mean number of patients was 20.6 ± 31.1 (range, 0–109). On the day of the questionnaire survey, there were 97 patients in the PICUs with an average number of 5.7 ± 7.2 (range, 0–22). None of the patients died within 24 hours of the questionnaire survey. The mean age of the patients was 3.4 ± 5.6 years. Sixty-six percent of patients were boys and 34% of patients were girls. The mean length of hospital stay was 82 ± 271 days, and the mean length of PICU stay was 64 ± 266 days.
In the case of intra-hospital transfers, 74% of the patients were transferred from other wards, 13% of the patients were transferred from the Emergency room, and 6% of the patients were transferred from the neonatal intensive care unit. The proportions of departments responsible for the infants were 59% for the pediatrics department, 26% for the thoracic surgery department, 8% for the critical care medicine department, 4% for the general surgery (including pediatric general surgery) department, 1% for the neurosurgery department and 1% for the transplantation surgery department.
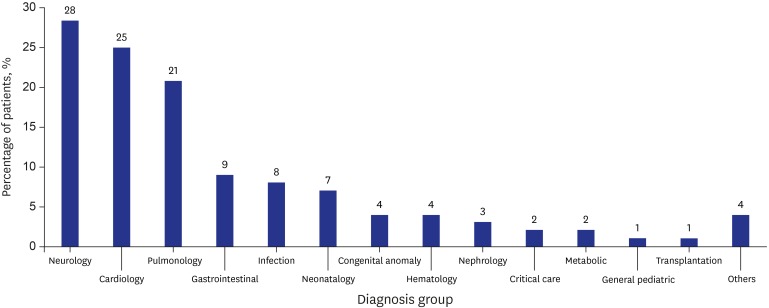
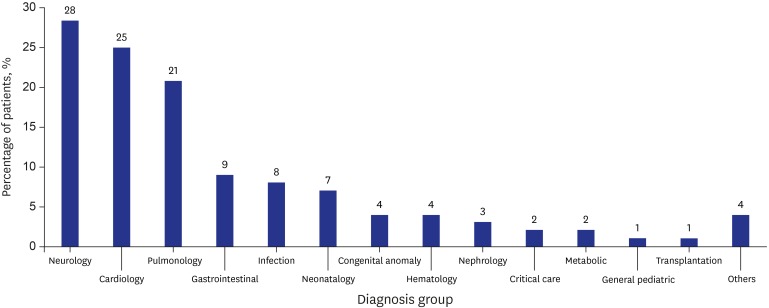
The proportions of reasons for admission of patients were as follows: 28% for neurologic diseases, 25% for cardiologic diseases, 21% for respiratory diseases, 9% for gastrointestinal illness, 8% for infections, 7% for neonatal diseases, 4% for congenital anomaly, 4% for hematologic diseases, 3% for nephrologic diseases, 2% for critical care, 2% for metabolic diseases, 1% for general pediatric diseases, 1% for transplantation, and 4% for other illnesses (
Fig. 1).
Fig. 1
Reason for admission to pediatric intensive care unit.
The mean PRISM score 24 was 9.4 ± 7.8 at the time of admission to the PICU. Sixty-four percent of the patients were using mechanical ventilators and 3% of the patients were using noninvasive ventilators. Eighty-eight percent of the patients had a central line. The mental status of patients was as follows: 70% of patients were alert, 1% of patients were drowsy, 16% of patients were stuporous, 1% of patients were in semicoma, 1% of patients were in coma, and 11% of patients were sedated.
Thirty-five percent of the patients were using sedative agents. Glasgow Coma Scale and COMFORT scale were used for sedation assessment of patients. When one agent was used, midazolam, fentanyl, or chloral hydrate was used. When two agents were used, fentanyl and midazolam or vecuronium, or midazolam and phenobarbital were used. When three agents were used, midazolam, fentanyl and vecuronium or ketamine were used. When four agents were used, midazolam, ketamine, vecuronium, and remifentanil were used. When five agents were used, dexmedetomidine, midazolam, ketamine, fentanyl, and vecuronium were used.
Thirty-nine percent of the patients were receiving infusion of continuous intravenous vasoactive medications. Of these patients, 29% were taking one of the following: dobutamine, dopamine, milrinone, or norepinephrine. Another 29% of patients were taking any of the following two medications: dobutamine, dopamine, epinephrine, norepinephrine and milrinone. Twenty-four percent of patients were taking three medications such as dobutamine, dopamine, epinephrine, norepinephrine, milrinone, vasopressin, nitroglycerin and nitroprusside. Eleven percent of patients were taking four medications and 8% of patients were taking 5 medications (
Table 3).
Table 3
Characteristics of pediatric patients in PICUs (n = 97)
|
Variables |
Values |
|
Sex |
|
|
Male |
64 (66.0) |
|
Female |
33 (34.0) |
|
Age, yr |
3.4 (0–25) |
|
Length of hospital days, day |
81.7 (1–2,539) |
|
Length of ICU stay, day |
64 (1–2,539) |
|
Assigned department |
|
|
Pediatrics |
57 (58.8) |
|
Thoracic surgery |
26 (26.8) |
|
Critical care medicine |
8 (8.3) |
|
General surgery (including pediatric surgery) |
4 (4.1) |
|
Neurosurgery |
1 (1.0) |
|
Transplantation surgery |
1 (1.0) |
|
PRISM III score on admission to ICU |
9.4 (0–32) |
|
Mental status |
|
|
Alert |
68 (70.1) |
|
Sedated |
11 (11.4) |
|
Drowsy |
1 (1.0) |
|
Stupurous |
15 (15.5) |
|
Semicoma |
1 (1.0) |
|
Coma |
1 (1.0) |
|
Organ failure |
32 (33.0) |
|
Terminal status |
6 (6.2) |
|
Nutritional support |
|
|
No |
13 (13.4) |
|
Enteral (oral and tube) |
52 (53.6) |
|
Parenteral |
8 (8.3) |
|
Enteral and parenteral |
24 (24.7) |
|
On mechanical ventilator |
62 (63.9) |
|
On noninvasive ventilation |
3 (3.1) |
|
Central line |
85 (87.6) |
|
Vasoactive agents |
38 (39.2) |
|
1 agent |
11 (28.9) |
|
2 agent |
11 (28.9) |
|
3 agent |
9 (23.8) |
|
4 agent |
4 (10.5) |
|
5 agent |
3 (7.9) |
|
Sedation and paralysis |
34 (35.1) |
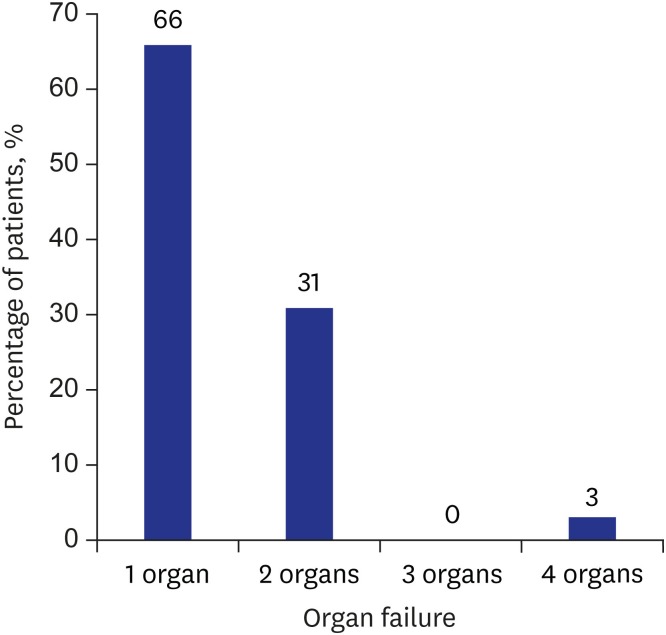
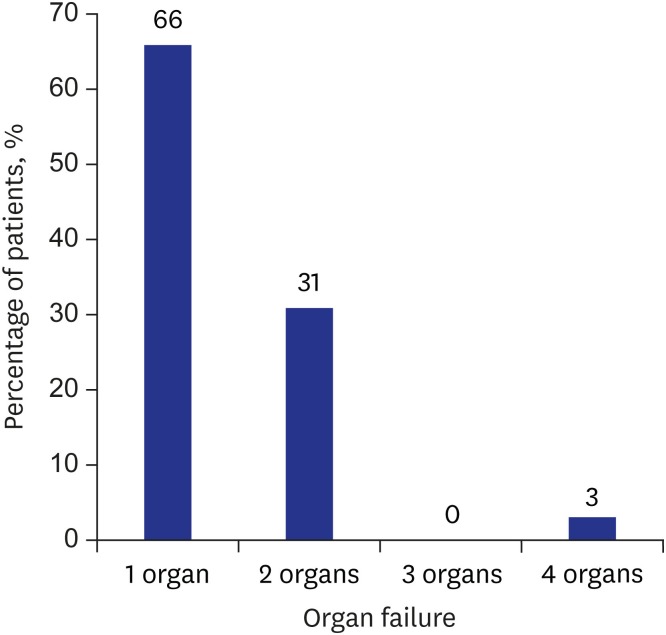
Thirty-nine percent of the patients had organ failure. Of these, 66% had 1 organ failure involving the brain, heart, kidney, liver, or lung. Thirty-one percent of patients had 2 organ failures involving the heart, kidney, liver, or lung. Three percent of patients had 4 organ failures involving the kidney, liver, lung, and pancreas (
Fig. 2).
Fig. 2
Organ failure of PICU patients.
PICU = pediatric intensive care unit.
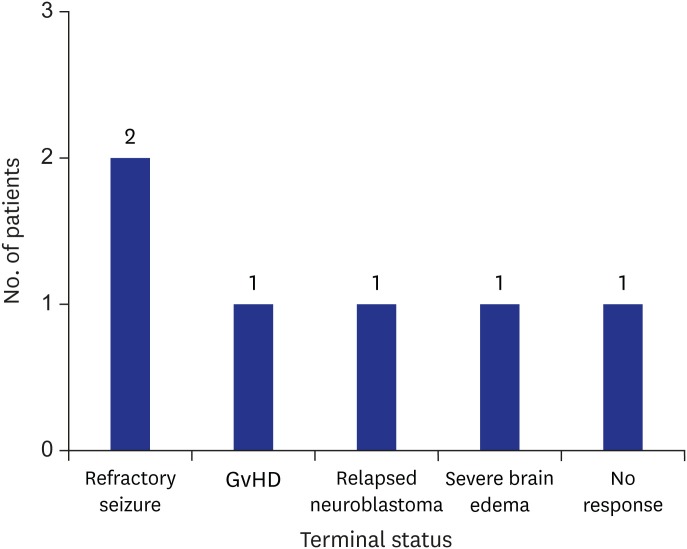
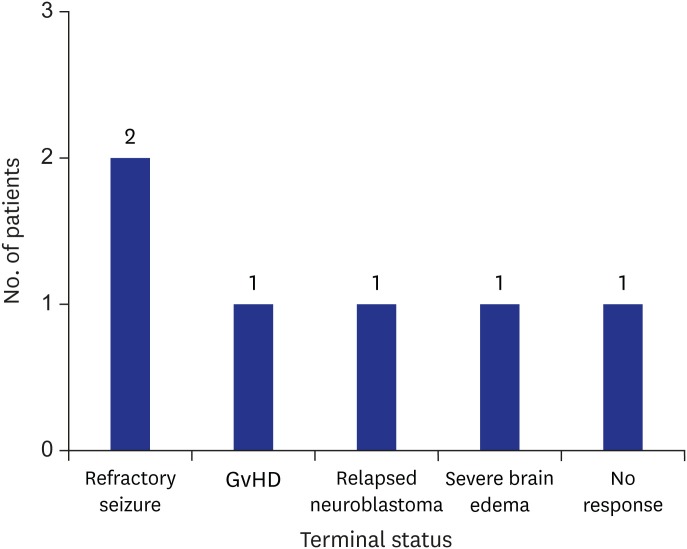
Six patients had a terminal status. Two of these six patients had refractory seizures, one patient had graft versus host disease, one patient had relapsed neuroblastoma, one patient had severe brain edema, and one patient did not show any response (
Fig. 3).
Fig. 3
Terminal status of PICU patients.
PICU = pediatric intensive care unit, GvHD = graft versus host disease.
DISCUSSION
This was the first study to conduct a survey on the status of PICUs in Korea. PCCM was first established in the 1960s.
1 John Downes established the first recorded pediatric ICU at Children's Hospital of Philadelphia in 1967.
1 Since then, PCCM has been continuously expanding and developing worldwide. In the United States, similar studies on PCCM have been conducted since the 1990s and in Europe since the 2000s.
2,3 However, due to the lack of awareness of the need for PCCM in Korea, there is no systematic investigation on the current status of PICUs. Therefore, the KSPCCM conducted a survey on the current status of PICUs in Korea.
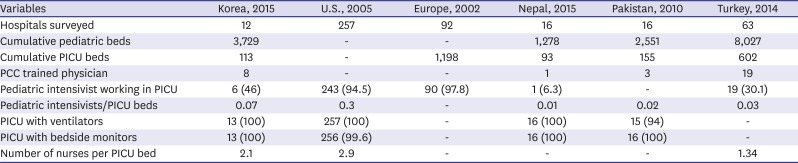
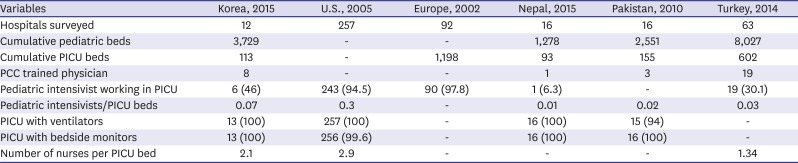
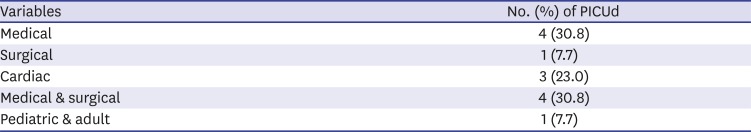
The number of PICUs in Korea was 13, which is not enough compared to 337 PICUs in the US in 2005 and 63 PICUs in Turkey in 2014.
2,4 The total number of beds in the PICU in Korea was 113. In 2015, the number of children and adolescents under 18 years of age in Korea was 8,753,064. The ratio of the number of PICU beds to the number of children and adolescents was 1:77,460 in Korea. It was estimated that number of children per PICU bed ranged from 1:18,000 to 1:50,000 in other countries.
4-8 There was 1 PICU bed per 18,542 pediatric populations in the United States. Based on this number, Korea has 1 quarter of PICU beds compared with the US standards. This shows that there is a considerable shortage of PICU beds compared to that in other countries. The average size of the PICU in Korea was 9.4 beds/unit (range, 2–30), which was similar to the size of the PICU of 12 beds/unit in the US, 8–10 beds/unit in Europe, and 9.6 beds/unit in Turkey.
2-4
Of the 28 doctors responsible for PCC, only 12 doctors were PCC specialists. Twelve PCC specialists worked in the PICUs of six Upper Grade General Hospitals. Only 46% of Korea's PICUs were staffed with a PCC specialist. This percentage was 94% in the United States, 98% in Europe, and 100% in Australia.
3,8 There are reports suggesting that mortality and complications are reduced, outcomes are improved, and resources are used more efficiently by reducing the number of inappropriate admissions in the PICUs with guidance from a PCC specialist.
9,10 This suggests that there is not only a significant lack of PCC specialists, but PICUs are also being operated inefficiently in Korea.
The ratio of PCC specialists to PICU beds was 1:9.4. This ratio was 1:2–1:4.5 in the United States, 1:1.2–1:1.6 in Europe, and 1:3–1:5 in Australia.
11,12 This suggests that PCC specialists face a considerable burden in Korea. This burden can also potentially adversely affect the patients in PICUs, which can lead to increased mortality and complications.
The ratio of nurses to PICU bed was 2.1:1 in Korea. Korean nurses are not nurses per shift, but nurses assigned to PICU. Unfortunately, the survey did not specifically measure the ratio of nurses per shift to patients or PICU beds. In the US, the ratio of nurses to PICU beds was 1:2.9 and in 81% of the investigated PICUs, this ratio was 1:2.
2 Nurses in the US are nurses per shift.
All 13 Upper Grade General Hospitals with PICUs had pediatric mechanical ventilators. This percentage was 100 percent in both the US and Nepal (
Table 4).
2,13
Table 4
Comparison with other national surveys on PICUs
|
Variables |
Korea, 2015 |
U.S., 2005 |
Europe, 2002 |
Nepal, 2015 |
Pakistan, 2010 |
Turkey, 2014 |
|
Hospitals surveyed |
12 |
257 |
92 |
16 |
16 |
63 |
|
Cumulative pediatric beds |
3,729 |
- |
- |
1,278 |
2,551 |
8,027 |
|
Cumulative PICU beds |
113 |
- |
1,198 |
93 |
155 |
602 |
|
PCC trained physician |
8 |
- |
- |
1 |
3 |
19 |
|
Pediatric intensivist working in PICU |
6 (46) |
243 (94.5) |
90 (97.8) |
1 (6.3) |
- |
19 (30.1) |
|
Pediatric intensivists/PICU beds |
0.07 |
0.3 |
- |
0.01 |
0.02 |
0.03 |
|
PICU with ventilators |
13 (100) |
257 (100) |
- |
16 (100) |
15 (94) |
- |
|
PICU with bedside monitors |
13 (100) |
256 (99.6) |
- |
16 (100) |
16 (100) |
- |
|
Number of nurses per PICU bed |
2.1 |
2.9 |
- |
- |
- |
1.34 |
There were 97 patients in PICUs on the day of the questionnaire survey. The proportion of boys was 66%, which was considerably higher than that of girls.
The proportions of reasons for admission of patients were as follows: 28% for neurologic diseases, 25% for cardiologic diseases, 21% for pulmonology diseases, 9% for gastrointestinal illness, 8% for infections, 7% for neonatal diseases, 4% for congenital anomaly, 4% for hematologic diseases, 3% for nephrologic diseases, 2% for critical care, 2% for metabolic diseases, 1% for general pediatric diseases, 1% for transplantation, and 4% for other illnesses. These proportions were similar to those in European countries and Turkey, where respiratory, neurological, and cardiac disease account for the majority of reasons for admission (
Fig. 1).
4,14
The mean PICU length of stay in Korea was 64 ± 266 days, which is exceptionally long. One of the patients was in vegetative state for 2,539 days, which increased the mean PICU length of stay. However, excluding this patient, the mean PICU length of stay was 38 ± 79 days. This finding is due to a special situation in Korea where there are many children in a vegetative state. However, there are few hospitals that can take care of these children. In addition, there are many difficulties associated with receiving treatment in a general ward, which causes these children to receive conservative care for a few months in a PICU. Due to this situation in Korea, the mean PICU length of stay has become considerably long.
This study has some limitations. First, this study was a questionnaire-based study, and therefore, it was difficult to conduct an entire survey. In the two surveys, 74% and 42% of the respondents answered the survey, respectively. There may be a selection bias. However, the strong point of this questionnaire survey is that it included all the Upper Grade General Hospitals nationwide.
Another limitation is that this study did not distinguish between PICUs with PCC specialists and those without PCC specialists. This made it difficult to compare PICUs with PCC specialists with those without PCC specialists. However, the aim of this study was to evaluate the current status of PICUs and PCC specialists in Korea.
This study did not utilize the criteria of the International Pediatric Sepsis Consensus Conference (IPSCC) in evaluating organ failure. To increase the response rate for the survey, we simplified the questionnaire and PCC intensivists judged the criteria for organ failure subjectively. This is one of the limitations in our study. Of course, objective criteria are very important to surveys, such as case reports or series, in which each patient's data are significant. However, this study presents the whole stream in Korea. In this case, the criteria are relatively less important than other aspects, so we decided to leave this to the discretion of the PCC intensivists.
In the case of intra-hospital transfers, 74% of the patients were transferred from other wards. These patients comprise post-operative care patients and non-surgical patients. It is difficult to determine the number of post-operative patients because we did not specifically investigate this aspect. This is also a limitation of our study. Further studies are needed to address these limitations.
As we mentioned above, the number of PICUs and total PICU beds in Korea are insufficient to accommodate all patients. Moreover, the number of PCC intensivists is also inadequate. This insufficiency prevents the efficient use of resources and inhibits PCC growth. For the advancement of PCC, it is required to expand the number of PICUs and the number of beds to the same high standard of more advanced countries. Moreover, support as an institutional dimension is necessary.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download