1. Tepel M, Aspelin P, Lameire N. Contrast-induced nephropathy: a clinical and evidence-based approach. Circulation. 2006; 113:1799–1806. PMID:
16606801.
2. Sadat U, Usman A, Gillard JH, Boyle JR. Does ascorbic acid protect against contrast-induced acute kidney injury in patients undergoing coronary angiography: a systematic review with meta-analysis of randomized, controlled trials. J Am Coll Cardiol. 2013; 62:2167–2175. PMID:
23994417.
3. Morcos SK, Thomsen HS, Webb JA. Contrast-media-induced nephrotoxicity: a consensus report. Contrast media safety committee, European society of urogenital radiology (ESUR). Eur Radiol. 1999; 9:1602–1613. PMID:
10525875.
4. Manske CL, Sprafka JM, Strony JT, Wang Y. Contrast nephropathy in azotemic diabetic patients undergoing coronary angiography. Am J Med. 1990; 89:615–620. PMID:
2239981.
5. Parfrey PS, Griffiths SM, Barrett BJ, Paul MD, Genge M, Withers J, Farid N, McManamon PJ. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med. 1989; 320:143–149. PMID:
2643041.
6. Gruberg L, Mintz GS, Mehran R, Gangas G, Lansky AJ, Kent KM, Pichard AD, Satler LF, Leon MB. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol. 2000; 36:1542–1548. PMID:
11079656.
7. Dangas G, Iakovou I, Nikolsky E, Aymong ED, Mintz GS, Kipshidze NN, Lansky AJ, Moussa I, Stone GW, Moses JW, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005; 95:13–19. PMID:
15619387.
8. Levy EM, Viscoli CM, Horwitz RI. The effect of acute renal failure on mortality. A cohort analysis. JAMA. 1996; 275:1489–1494. PMID:
8622223.
9. Pattharanitima P, Tasanarong A. Pharmacological strategies to prevent contrast-induced acute kidney injury. Biomed Res Int. 2014; 2014:236930. PMID:
24719848.
10. Persson PB, Hansell P, Liss P. Pathophysiology of contrast medium-induced nephropathy. Kidney Int. 2005; 68:14–22. PMID:
15954892.
11. Tumlin J, Stacul F, Adam A, Becker CR, Davidson C, Lameire N, McCullough PA; CIN Consensus Working Panel. Pathophysiology of contrast-induced nephropathy. Am J Cardiol. 2006; 98:14K–20K. PMID:
16784912.
12. Bakris GL, Lass NA, Glock D. Renal hemodynamics in radiocontrast medium-induced renal dysfunction: a role for dopamine-1 receptors. Kidney Int. 1999; 56:206–210. PMID:
10411694.
13. Gare M, Haviv YS, Ben-Yehuda A, Rubinger D, Bdolah-Abram T, Fuchs S, Gat O, Popovtzer MM, Gotsman MS, Mosseri M. The renal effect of low-dose dopamine in high-risk patients undergoing coronary angiography. J Am Coll Cardiol. 1999; 34:1682–1688. PMID:
10577557.
14. Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000; 343:180–184. PMID:
10900277.
15. Spargias K, Alexopoulos E, Kyrzopoulos S, Iokovis P, Greenwood DC, Manginas A, Voudris V, Pavlides G, Buller CE, Kremastinos D, et al. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation. 2004; 110:2837–2842. PMID:
15492300.
16. Kidney Disease; Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012; 2:1–138.
17. Singh U, Devaraj S, Jialal I. Vitamin E, oxidative stress, and inflammation. Annu Rev Nutr. 2005; 25:151–174. PMID:
16011463.
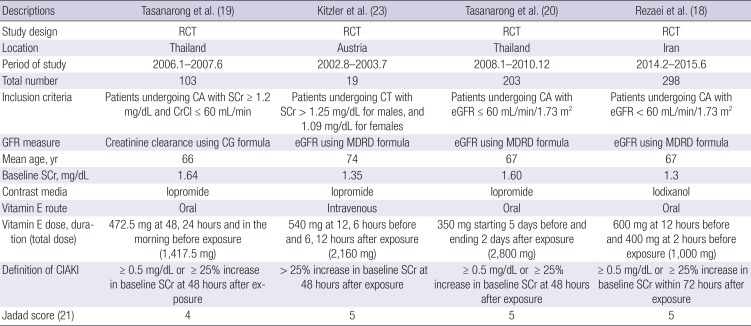
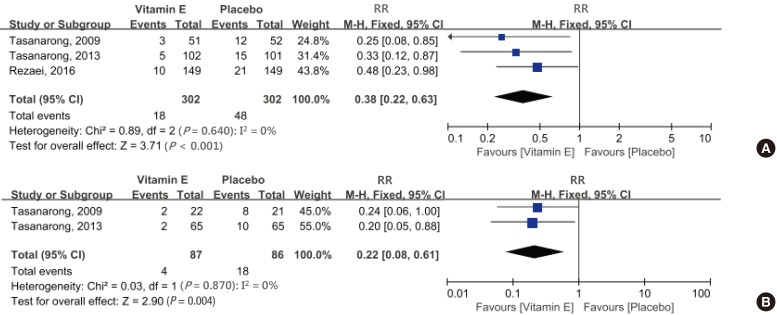
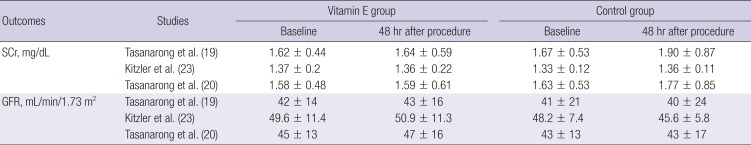
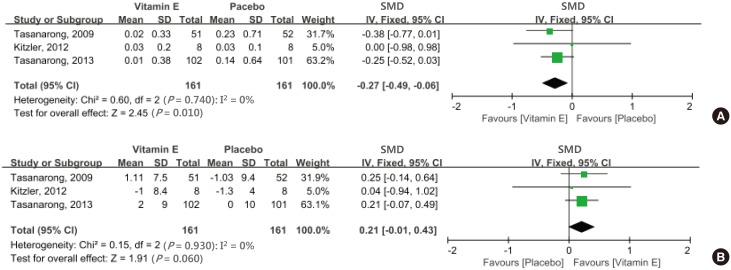
18. Rezaei Y, Khademvatani K, Rahimi B, Khoshfetrat M, Arjmand N, Seyyed-Mohammadzad MH. Short-term high-dose vitamin E to prevent contrast medium-induced acute kidney injury in patients with chronic kidney disease undergoing elective coronary angiography: a randomized placebo-controlled trial. J Am Heart Assoc. 2016; 5:e002919. PMID:
27068631.
19. Tasanarong A, Piyayotai D, Thitiarchakul S. Protection of radiocontrast induced nephropathy by vitamin E (alpha tocopherol): a randomized controlled pilot study. J Med Assoc Thai. 2009; 92:1273–1281. PMID:
19845233.
20. Tasanarong A, Vohakiat A, Hutayanon P, Piyayotai D. New strategy of α- and γ-tocopherol to prevent contrast-induced acute kidney injury in chronic kidney disease patients undergoing elective coronary procedures. Nephrol Dial Transplant. 2013; 28:337–344. PMID:
23314316.
21. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17:1–12. PMID:
8721797.
22. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID:
12958120.
23. Kitzler TM, Jaberi A, Sendlhofer G, Rehak P, Binder C, Petnehazy E, Stacher R, Kotanko P. Efficacy of vitamin E and N-acetylcysteine in the prevention of contrast induced kidney injury in patients with chronic kidney disease: a double blind, randomized controlled trial. Wien Klin Wochenschr. 2012; 124:312–319. PMID:
22527829.
24. Thomsen HS, Morcos SK. Contrast media and the kidney: European Society of Urogenital Radiology (ESUR) guidelines. Br J Radiol. 2003; 76:513–518. PMID:
12893691.
25. Brigelius-Flohé R, Traber MG. Vitamin E: function and metabolism. FASEB J. 1999; 13:1145–1155. PMID:
10385606.
26. Liu P, Feng Y, Wang Y, Zhou Y, Zhao L. Protective effect of vitamin E against acute kidney injury. Biomed Mater Eng. 2015; 26(Suppl 1):S2133–S2144. PMID:
26405992.
27. Firuzi O, Miri R, Tavakkoli M, Saso L. Antioxidant therapy: current status and future prospects. Curr Med Chem. 2011; 18:3871–3888. PMID:
21824100.
28. Biondi-Zoccai G, Lotrionte M, Thomsen HS, Romagnoli E, D'Ascenzo F, Giordano A, Frati G. Nephropathy after administration of iso-osmolar and low-osmolar contrast media: evidence from a network meta-analysis. Int J Cardiol. 2014; 172:375–380. PMID:
24502883.
29. Meinel FG, De Cecco CN, Schoepf UJ, Katzberg R. Contrast-induced acute kidney injury: definition, epidemiology, and outcome. Biomed Res Int. 2014; 2014:859328. PMID:
24734250.
30. Cochemé HM, Murphy MP. Can antioxidants be effective therapeutics? Curr Opin Investig Drugs. 2010; 11:426–431.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download