Abstract
To evaluate methicillin-resistance (MR) rates among community-associated (CA) Staphylococcus aureus infections in the Korean military, we screened electronic medical records of 223 patients with S. aureus infection in a military referral hospital from 2012 to 2017. During the study period, MR rates did not change annually, and were not different between officers and conscripted personnel. Among conscripted personnel, MR rates in CA S. aureus infections did not increase with longer duration of military service, both in trend analysis and multivariate analysis. In conclusion, MR rates among CA S. aureus infections did not increase during military service in Korea.
Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) has become a serious healthcare concern worldwide, with dominant CA-MRSA strains showing specific distributions in each country.12 Since the early 2000s, the Panton-Valentine leukocidin (PVL)-negative sequence type 72-SCCmec type IV (ST72-SCCmecIV) strain has been reported as the dominant CA-MRSA strain in Korea, and its prevalence in both CA and healthcare-associated (HA) infections has been increasing.34 Although congregate settings including military barracks have been reported to represent a risk for PVL-positive ST8 MRSA (USA300) colonization,56 epidemiologic risk factors for ST72 strains in the community are not well-identified.7 In Korea, participation in military service for about a two-year period is an obligation for all male citizens, constituting the largest congregated community of young adults. Since around 260,000 persons newly enter the service and return to community every year, whether CA-MRSA spreads through military service or not is an important issue for the epidemiology of CA-MRSA in Korean society. To answer this question, we conducted an epidemiologic evaluation in a Korean military hospital for a five-year period.
An observational and case-control study was conducted in the Armed Forces Capital Hospital (AFCH), a 660-bed military hospital which serves as a community hospital for neighboring troops and the only referral center for other military hospitals. We screened microbiologic data from June 2012 to May 2017 and reviewed the electronic medical records (EMRs) of patients with S. aureus infection. Only the first infection episode for each patient was included in the analysis. An episode of S. aureus infection was defined as isolation of S. aureus from a clinical specimen with relevant clinical symptoms and signs of infection.8 Cases of infection that improved without the use of proper antibiotics or surgical drainage were considered to be colonization or contamination and were excluded from the analysis. We followed the CA-MRSA case definition of the United States Centers for Disease Control and Prevention (CDC) Active Bacterial Core Surveillance Program: specifically, a CA-MRSA case was a patient with a MRSA infection without healthcare factors (i.e., surgery; hospitalization; or residence in a long-term care facility within the year before infection, presence of a percutaneous device or indwelling catheter, dialysis within the previous year, hospitalization > 48 hours before MRSA culture, or previous MRSA infection or colonization).910 Hospital-onset MRSA infection and community-onset MRSA infection with any of above described healthcare factors were classified as HA infection. Other medical histories including visiting outpatient department (OPD) of military hospitals or using primary medical care at military troops within three months were additionally identified among patients with CA infections. Conscripted personnel were soldiers who served or were serving obligatory military service for a two-year period as enlisted soldiers. Military officers were those in occupational positions, including commissioned and non-commissioned officers. This study was approved by the Institutional Review Board of Armed Forces Capital Hospital (IRB-2017-02-02).
For identification and antimicrobial susceptibility testing, including for methicillin, the VITEK 2 automated system (bioMérieux Inc., Marcy l'Etoile, France) was used with a standard identification card and the modified broth microdilution method. Minimum inhibitory concentration breakpoints and quality control protocols were used according to the standards established by the Clinical and Laboratory Standards Institute.11 A standard of < 4 μg/mL was used as a breakpoint for susceptibility to mupirocin,12 and a standard of < 1 μg/mL was used for fusidic acid.13
A linear regression model was used to evaluate trends of methicillin-resistance (MR) rates according to year of acquisition and duration of military service. Student's t-test was used for the comparison of continuous variables, while χ2 and Fisher's exact tests were used for categorical variables. Factors that can affect MR rates were evaluated with multivariate analysis using a logistic regression model. Age at the time of enlistment, military branch, and military rank were included in the multivariate analysis. All P values were two-tailed, and those that were < 0.05 were considered to be statistically significant. IBM SPSS Statistics version 20.0 for Windows (IBM, Armonk, NY, USA) was used for all statistical analyses.
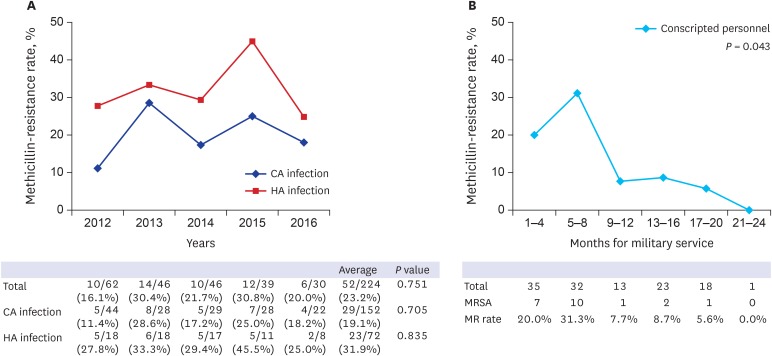
During the study period, a total of 223 patients with S. aureus infection were identified, including 151 CA infection (67.7%) and 72 HA infection (32.3%) infections. Among 151 CA infections, 29 were MRSA (19.2%) and 122 were methicillin-susceptible S. aureus (MSSA, 80.8%). Annual MR rate did not show an increasing nor decreasing trend during the study period, demonstrating specific rates of 16.1%, 30.4%, 21.7%, 30.8%, and 20.0% from 2012 to 2016, respectively (P = 0.751 by linear regression; Fig. 1A). A subgroup analysis of CA and HA infections also did not show a certain trend.
With regard to CA infections, patient age, sex, military branch, and military rank were not statistically different between those with CA-MRSA and those with CA-MSSA (Supplementary Table 1). Among conscripted personnel, the cumulative days of military service were significantly shorter for those with CA-MRSA infections versus those with CA-MSSA (192.8 vs. 279.9 days, P = 0.013). MR rate showed a significantly decreasing trend according to cumulative days of service (P = 0.043 by linear regression; Fig. 1B). Patients with corporal and sergeant ranks (those served ≥ 12 months) showed a significantly lower MR rate (Supplementary Table 2; P = 0.010). In the evaluation of CA-MRSA infection among conscripted personnel, corporal or sergeant ranks (odds ratio [OR], 0.19; 95% confidence interval [CI], 0.04–0.60; P = 0.011) were reversely associated with CA-MRSA infection in the multivariate analysis (Supplementary Table 3).
Skin and soft tissue infection (SSTI, 69.0%) was the most common type of CA-MRSA infection, followed by ear infection (31.0%). Although significantly higher proportion of CA-MRSA SSTI patients (20.0%) had history of OPD or primary care visit compared to CA-MSSA SSTI (1.4%), only one patient in each group was previously treated with antibiotics. Among ear infections, previous history of visitation to the ear, nose, and throat (ENT) OPD within three months was significantly associated with MRSA infection (P = 0.043). Patients with CA-MRSA infection rarely had underlying diseases (only one patient had diabetes mellitus).
Korean male citizens are conscripted in their early 20s and serve as enlisted grade soldiers for about two years, depending on the branch. After four weeks of training, approximately 30 to 35 soldiers are designated to constitute a platoon (in the army) and henceforth reside in a barrack together. Contact with persons outside of the platoon is limited. However, since most enlisted soldiers return to their own community after service, evaluation of MR rates in CA S. aureus infections among soldiers is not only important for the healthcare of military personnel, but is also essential for understanding CA-MRSA epidemiology in Korean society. In addition, although the present study was performed in a single military hospital, the AFCH is the only referral hospital in the Korean military and the patient population is overall representative of Korean military personnel.
Of note, MR rates in CA S. aureus infections did not increase during obligatory military service. Overall MR rate did not increase during the study period, which might increase if transmission of CA-MRSA in barracks actively occurred. The MR rate of conscripted personnel decreased according to cumulative days of military service, and higher ranks were reversely associated with CA-MRSA infection in the multivariate analysis. These findings suggest the widespread transmission of MRSA through communal living in a barrack is not likely to occur, and that obligatory military service may not be a significant source of CA-MRSA in Korean society. Although the MR rate of conscripted personnel during the initial eight months of service (25.4%) was higher than the average of CA infection in the present study (19.1%), the values were within the range of previously reported MR rates of CA infections in Korea (13.0% to 33.0%).271415 For a more detailed evaluation of CA-MRSA epidemiology of Korean community and military, the initial colonization status at the time of enlistment and changes during military service need to be assessed.
The decreasing MR rates in CA S. aureus infections during military service should be cautiously interpreted. Although statistical analysis showed reverse association of CA-MRSA infection and duration of military service, included patients with corporal or sergeant ranks were fewer than lower ranks (39.3% of the conscripted personnel). Degree of physical activity and accessibility to military hospital would be different according to the ranks, which is difficult to be adjusted. Considering such limitations, it would be more relevant to interpret the current study result as an evidence of non-increasing MR rates of CA S. aureus infection during obligatory military service rather than decreasing MR rates.
In addition to the limited number of cases and above mentioned cautions in interpreting data, the present study has several limitations. First, since our study is based on a retrospective review of microbiologic database and EMR, we did not perform molecular tests using clinical isolates. Second, we reviewed MR rates among patients with S. aureus infection, while the carriage or colonization rate of CA-MRSA was not evaluated. Since cultures are more likely to be performed in refractory infections or abscess-forming SSTI, MR rates in this study would be higher than the actual colonization rate of CA-MRSA. A previous epidemiologic study evaluating Korean military recruits from November 2004 to March 2005 reported 6.6% of CA-MRSA colonization rate,16 and a follow-up study is required for the evaluation of current epidemiologic status. Third, although we followed a previously used definition of CA-MRSA, a certain portion of cases would be originated from OPD or primary care. History of OPD visit was more frequently noticed in cases with CA-MRSA, and higher antimicrobial resistance was observed in isolates from ear infections. These findings suggest that a certain proportion of CA-MRSA isolates would be originated from healthcare environment. Lastly, although we did not include self-limiting cases, colonization or contaminations were not perfectly excluded, because non-sterile clinical specimens, especially ear discharge swab culture, were included. Despite these limitations, our study results suggest that Korean military barracks would not be a source of CA-MRSA transmission.
In conclusion, in a retrospective epidemiologic study evaluating a five-year period in a Korean military referral hospital, MR rates among CA S. aureus infections did not increase during military service.
References
1. Chen CJ, Huang YC. New epidemiology of Staphylococcus aureus infection in Asia. Clin Microbiol Infect. 2014; 20(7):605–623. PMID: 24888414.
2. Song JH, Hsueh PR, Chung DR, Ko KS, Kang CI, Peck KR, et al. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: an ANSORP study. J Antimicrob Chemother. 2011; 66(5):1061–1069. PMID: 21393157.
3. Ma SH, Lee YS, Lee SH, Kim HK, Jin JS, Shin EK, et al. Meticillin-resistant Staphylococcus aureus clones with distinct clinical and microbiological features in a Korean community. J Med Microbiol. 2007; 56(Pt 6):866–868. PMID: 17510277.
4. Joo EJ, Chung DR, Ha YE, Park SY, Kang SJ, Kim SH, et al. Community-associated Panton-Valentine leukocidin-negative meticillin-resistant Staphylococcus aureus clone (ST72-MRSA-IV) causing healthcare-associated pneumonia and surgical site infection in Korea. J Hosp Infect. 2012; 81(3):149–155. PMID: 22652522.
5. Millar EV, Rice GK, Elassal EM, Schlett CD, Bennett JW, Redden CL, et al. Genomic characterization of USA300 methicillin-resistant Staphylococcus aureus (MRSA) to evaluate intraclass transmission and recurrence of skin and soft tissue infection (SSTI) among high-risk military trainees. Clin Infect Dis. 2017; 65(3):461–468. PMID: 28419202.
6. Campbell KM, Vaughn AF, Russell KL, Smith B, Jimenez DL, Barrozo CP, et al. Risk factors for community-associated methicillin-resistant Staphylococcus aureus infections in an outbreak of disease among military trainees in San Diego, California, in 2002. J Clin Microbiol. 2004; 42(9):4050–4053. PMID: 15364988.
7. Kim ES, Kim HB, Kim G, Kim KH, Park KH, Lee S, et al. Clinical and epidemiological factors associated with methicillin resistance in community-onset invasive Staphylococcus aureus infections: prospective multicenter cross-sectional study in Korea. PLoS One. 2014; 9(12):e114127. PMID: 25485895.
8. Park GE, Ko JH, Cho SY, Ha YE, Lee NY, Kang CI, et al. Empirical combination of a β-lactam to vancomycin may not improve outcomes of methicillin-susceptible Staphylococcus aureus bacteremia, compared to vancomycin monotherapy. Eur J Clin Microbiol Infect Dis. 2017; 36(7):1091–1096. PMID: 28078559.
9. Buck JM, Como-Sabetti K, Harriman KH, Danila RN, Boxrud DJ, Glennen A, et al. Community-associated methicillin-resistant Staphylococcus aureus, Minnesota, 2000–2003. Emerg Infect Dis. 2005; 11(10):1532–1538. PMID: 16318692.
10. Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005; 352(14):1436–1444. PMID: 15814879.
11. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. Wayne, PA: Clinical and Laboratory Standards Institute;2016. CLSI supplement M100S.
12. Finlay JE, Miller LA, Poupard JA. Interpretive criteria for testing susceptibility of staphylococci to mupirocin. Antimicrob Agents Chemother. 1997; 41(5):1137–1139. PMID: 9145883.
13. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 7.1. Updated 2017. Accessed December 27, 2017. http://www.eucast.org.
14. Moon HW, Kim HJ, Hur M, Yun YM. Antimicrobial susceptibility profiles of Staphylococcus aureus isolates classified according to their origin in a tertiary hospital in Korea. Am J Infect Control. 2014; 42(12):1340–1342. PMID: 25444309.
15. Lee JY, Chong YP, Kim T, Hong HL, Park SJ, Lee ES, et al. Bone and joint infection as a predictor of community-acquired methicillin-resistant Staphylococcus aureus bacteraemia: a comparative cohort study. J Antimicrob Chemother. 2014; 69(7):1966–1971. PMID: 24695351.
16. Choi CM, Kang CI, Kim YK, Heo ST, Kim CH, Song JK, et al. Community-associated methicillin-resistant Staphylococcus aureus colonization in the upper respiratory tracts of Korean military recruits. Tuberc Respir Dis. 2009; 67(5):409–412.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Baseline characteristics and clinical presentation of CA-MRSA in comparison with CA-MSSA infections
Supplementary Table 2
Comparison of CA-MRSA and CA-MSSA infection in conscripted personnel
Supplementary Table 3
Univariate and multivariate analysis for factors associated with MR of CA Staphylococcus aureus infections among conscripted personnel
Fig. 1
Epidemiologic trends of MR rates in a military hospital. (A) MR rates during the study period did not show increasing or decreasing trends both in CA- and HA-infection. Each year covered June of the year in question to May of the following year. (B) MR rates of conscripted personnel did not increase according to the cumulative days of military service.
MR = methicillin-resistance, CA = community-associated, HA = healthcare-associated, MRSA = methicillin-resistant Staphylococcus aureus.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download