This article has been
cited by other articles in ScienceCentral.
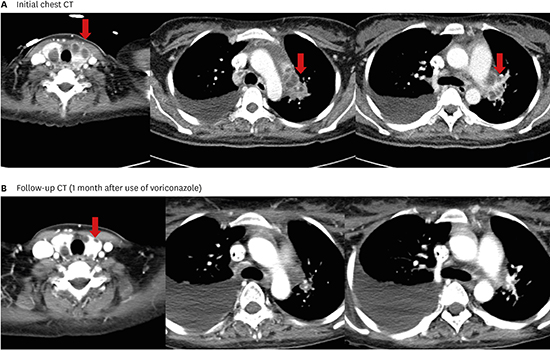
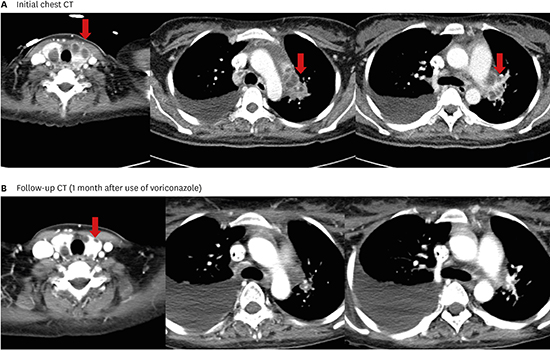
A 29-year-old woman who was diagnosed with lupus nephritis and treated with steroid pulse therapy and cyclophosphamide two months ago, readmitted to our hospital because of fever. A computed tomography (CT) scan showed multiple cystic lesions in the thyroid gland and necrotic cervical and mediastinal lymphadenopathies. However, no parenchymal abnormalities were noted in either of the lungs (
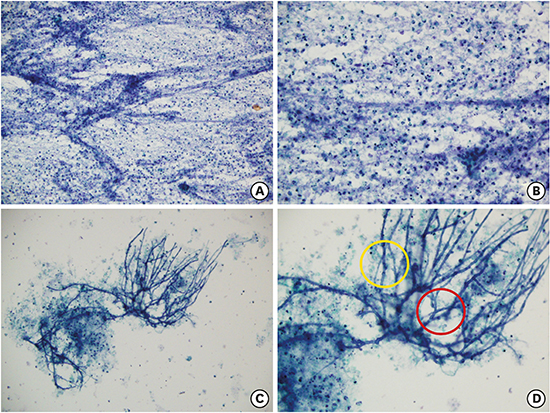
Fig. 1). We underwent an ultrasonography-guided aspiration for the lesion in the thyroid gland and cervical lymph node. Cytology of the thyroid aspiration showed acute angle branching fungal hyphae consistent with
Aspergillus species (
Fig. 2). Also, fungal culture of cervical lymph node was positive for
A. fumigatus. Consecutive tests for serum galactomannan antigen level (Platelia
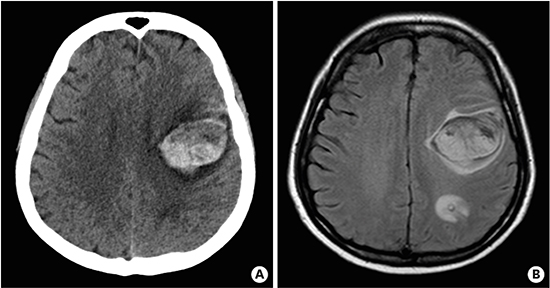
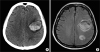
Aspergillus EIA; BioRad, Redmond, WA, USA) were positive (3.20 and 3.66). Being diagnosed with thyroid gland aspergillosis, she was treated with voriconazole. Two weeks after admission, she abruptly developed right hemiplegia and aphagia; and a brain CT showed multiple cerebral hemorrhagic lesions (
Fig. 3). We could not perform brain biopsy as the patient and her husband refused the option of surgery. Although we could not draw the definitive diagnosis of cerebral lesion without histological confirmation, we believed that cerebral hemorrhage could have been a consequence of either cerebral aspergillosis, or vasculitis associated with systemic lupus erythematosus (SLE) and planned a long-term antifungal therapy.
One month later, the neck and chest CT showed regression of the previous aspergillosis lesions (
Fig. 1). She received intravenous voriconazole (6 mg/kg q 12 hours for 2 doses followed by 4 mg/kg q 12 hours) for nine months until she died of a complicated intra-abdominal infection.
Herein we report a case of invasive thyroid aspergillosis in a patient with SLE. The present case has some implications. First, voriconazole may be a good option for treatment of thyroid aspergillosis. To our knowledge, there have been three reports of thyroid aspergillosis in patients with SLE, all treated with conventional amphotericin B.
123 Two are deceased,
23 and one patient has survived with total thyroidectomy.
1 However, our patient improved without thyroidectomy, and we believed voriconazole was associated with successful outcome, which is now considered to be a primary antifungal agent based on previous randomized controlled studies.
4 Second, it was unusual that her lungs were spared since invasive aspergillosis is mostly contracted by inhaling the conidia of
Aspergillus spp. followed by tissue invasion of lung and/or hematogenous dissemination.
5 It is easy to overlook positive galactomannan test result in a patient without lung lesion as there is a possibility of a false positive serum galactomannan test due to the use of antibiotics or transfusion.
5 Although rare, our case suggests that if an immunocompromised patient tests positive for serum galactomannan with normal finding in chest CT, the possibility of extrapulmonary aspergillosis such as thyroid aspergillosis should be considered.
Figures and Tables
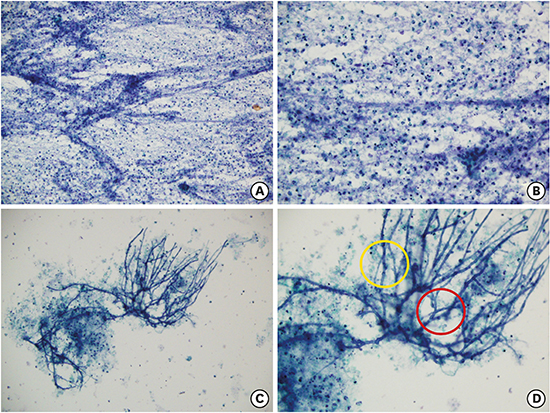
Fig. 1
Computed tomography (CT) images. (A) Initial chest CT shows multiple cystic lesions in both lobes of the thyroid gland (red arrows) and necrotic lymphadenopathy in the para-aortic, right lower paratracheal, and left hilar lymph nodes (red arrows). (B) CT scan at one-month follow-up after treatment with voriconazole shows a decrease in the size of cystic lesions in both the thyroid gland (red arrows) and necrotic lymph nodes.

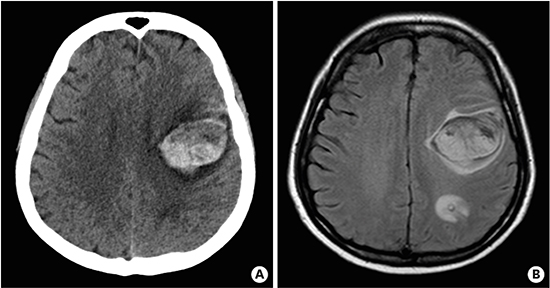
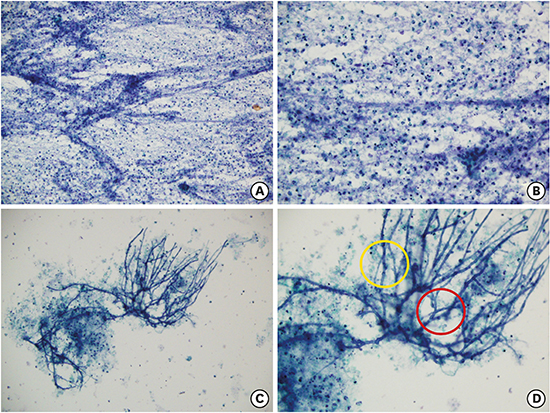
Fig. 2
Cytological findings. (A) Papanicolaou stain × 200. The aspiration smear shows moderate cellular aspirate of abundant necrotic debris. (B) Papanicolaou stain × 400. The aspiration smear shows abundant neutrophils, necrotic debris and occasional lymphoid cells indicating abscess. (C) Papanicolaou stain × 200. The aspiration smear shows fungal infection with necrotic debris. (D) Papanicolaou stain × 400. The fungus has regular, septate hyphae (yellow) with acute angle branching (red).

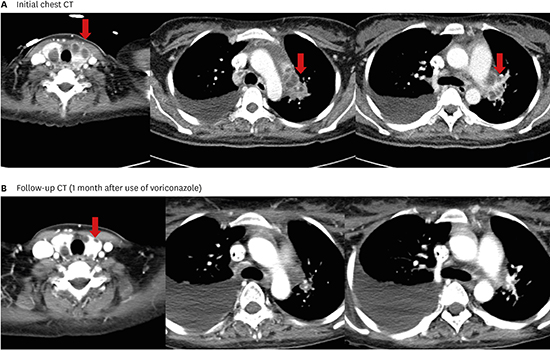
Fig. 3
Brain imaging. (A) Non-enhanced brain computed tomography scan, and (B) axial T2 FLAIR magnetic resonance image shows multifocal hemorrhagic lesions with surrounding edema in the left frontal and parietal lobe. A small amount of subarachnoid hemorrhage is also noted.
ACKNOWLEDGMENTS
We thank to Misung Kim and Gyeong Min Park for helpful comments.
References
1. Kim SH, Kim JY, Park WC, Kim MK, Kim TJ. Sequential sonographic features of primary invasive aspergillosis involving only the thyroid gland: a case report and literature review. Iran J Radiol. 2016; 13(1):e27890.

2. Marui S, de Lima Pereira AC, de Araujo Maia RM, Borba EF. Suppurative thyroiditis due to aspergillosis: a case report. J Med Case Reports. 2014; 8:379.

3. Torres AM, Agrawal S, Peters S, Khurana K, Feiglin D, Schroeder E, et al. Invasive aspergillosis diagnosed by fine-needle aspiration of the thyroid gland. Thyroid. 1999; 9(11):1119–1122.

4. Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002; 347(6):408–415.

5. Segal BH. Aspergillosis. N Engl J Med. 2009; 360(18):1870–1884.