1. Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine. 2006; 31(23):2747–2755.
2. Teyssédou S, Saget M, Pries P. Kyphopasty and vertebroplasty. Orthop Traumatol Surg Res. 2014; 100(1):Suppl. S169–S179.

3. Zhao S, Xu CY, Zhu AR, Ye L, Lv LL, Chen L, et al. Comparison of the efficacy and safety of 3 treatments for patients with osteoporotic vertebral compression fractures: a network meta-analysis. Medicine (Baltimore). 2017; 96(26):e7328.
4. Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Skeletal Radiol. 2004; 33(9):493–505.

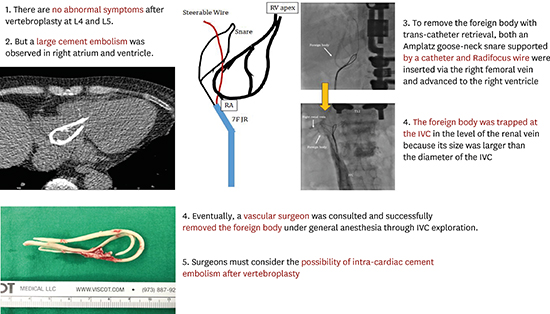
5. Audat ZA, Alfawareh MD, Darwish FT, Alomari AA. Intracardiac leakage of cement during kyphoplasty and vertebroplasty: a case report. Am J Case Rep. 2016; 17:326–330.

6. Al-Nakshabandi NA. Percutaneous vertebroplasty complications. Ann Saudi Med. 2011; 31(3):294–297.

7. Luetmer MT, Bartholmai BJ, Rad AE, Kallmes DF. Asymptomatic and Unrecognized Cement Pulmonary Embolism Commonly Occurs with Vertebroplasty. AJNR Am J Neuroradiol. 2011; 32(4):654–657.

8. Kim YJ, Lee JW, Park KW, Yeom JS, Jeong HS, Park JM, et al. Pulmonary cement embolism after percutaneous vertebroplasty in osteoporotic vertebral compression fractures: incidence, characteristics, and risk factors. Radiology. 2009; 251(1):250–259.

9. Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg. 2017; 101:633–642.

10. Janssen I, Ryang YM, Gempt J, Bette S, Gerhardt J, Kirschke JS, et al. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017; 17(6):837–844.

11. Prokop A, Hägele M, Pfeilsticker U, Koll S, Chmielnicki M. Pericardial perforation 2.5 years after kyphoplasty. A rare complication after cement extravasation. Unfallchirurg. 2013; 116(1):80–84.
12. Zhao Y, Liu T, Zheng Y, Wang L, Hao D. Successful percutaneous retrieval of a large pulmonary cement embolus caused by cement leakage during percutaneous vertebroplasty: case report and literature review. Spine. 2014; 39(26):E1616–E1621.
13. Grifka RG, Tapio J, Lee KJ. Transcatheter retrieval of an embolized methylmethacrylate glue fragment adherent to the right atrium using bidirectional snares. Catheter Cardiovasc Interv. 2013; 81(4):648–650.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download