INTRODUCTION
CASE DESCRIPTION
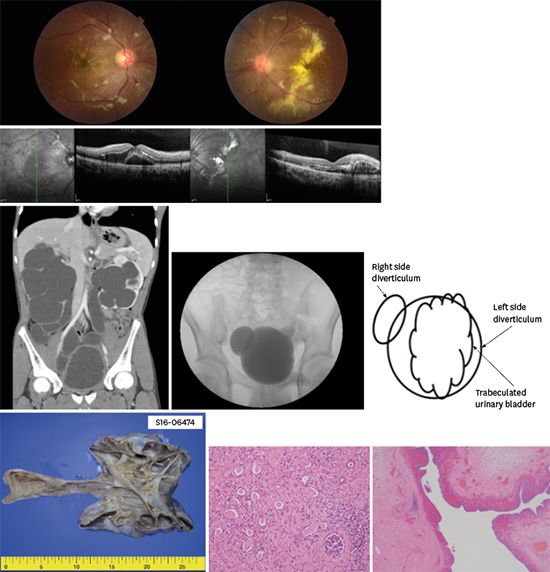
Fig. 1

Fig. 2

Fig. 3

Journal List > J Korean Med Sci > v.33(8) > 1107711



San Kim 
https://orcid.org/0000-0002-0436-5010
Sang-Hoo Park 
https://orcid.org/0000-0002-2355-9566
Dong Yoon Kim 
https://orcid.org/0000-0002-6058-0145
Seok-Joong Yun 
https://orcid.org/0000-0001-7737-4746
Ok-Jun Lee 
https://orcid.org/0000-0003-2065-3597
Heon-Seok Han 
https://orcid.org/0000-0003-0012-2545