This article has been
cited by other articles in ScienceCentral.
A previously healthy 11-year-old male child presented with severe chest pain, dysphagia, and tearing heartburn that started 3 weeks prior. He was diagnosed as having ileus at another hospital, and proton-pump inhibitor (PPI) and probiotics were given. Within two weeks, he suddenly presented high fever and severe heartburn, and was therefore admitted to a hospital. Esophagogastric endoscopy revealed multiple deep ulcers in the esophagus that are usually seen in herpes simplex virus (HSV)-infectious esophagitis. Intravenous acyclovir was administered despite the lack of any pathologic evidence. However, his symptoms became even more serious. On admission to our hospital, he was extremely emaciated with a weight loss of 14% of his original body weight of 34.4 kg, and could not swallow a spoonful of water due to severe dysphagia and odynophagia. He had no underlying diseases and immunodeficiency. Physical examination yielded tenderness on the epigastric and lower abdominal area. Blood tests yielded the following results: white blood cell (WBC) 26,200/mm
3 with 90% of polynucleotide WBC, normal hemoglobin and platelet count, erythrocyte sedimentation rate 2 mm/hr, and C-reactive protein 11.15 (normal range 0–0.3). Serum biochemistry laboratory data and CD3 and CD4 were within normal ranges. Blood polymerase chain reaction for human immunodeficiency virus and HSV were negative.
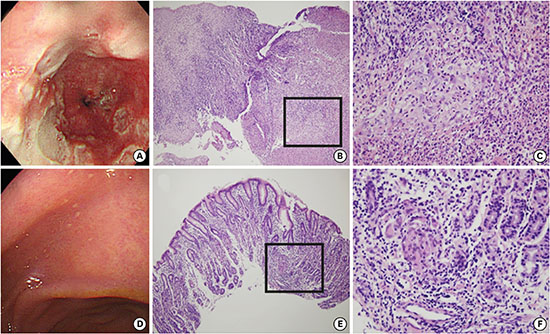
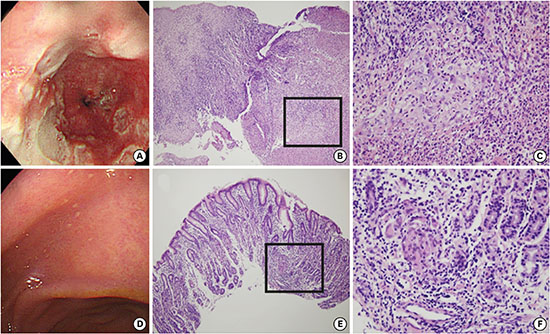
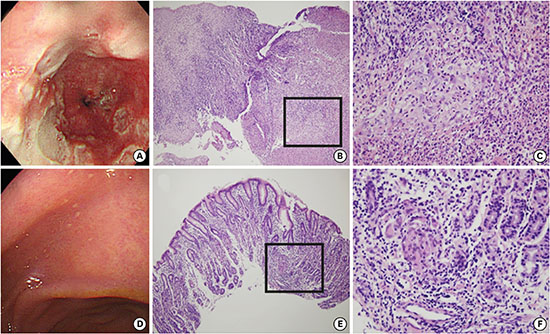
Helicobacter pylori (HP) were negative in the stool HP-antigen, rapid urease test, serum HP-immunoglobulin G, and stomach pathology. Stool occult blood and stool WBC were negative. Esophagogastric endoscopy revealed numerous deep ulcers still persistent in the proximal and mid portion of esophagus and a number of aphthous fine ulcers in the cardia and the body (
Fig. 1). Colonoscopy showed no specific lesion. Non-caseous granulomas were found in the lamina propria with positivity for CD68 and ulcers with granulation tissue formation without evidence of viral infection were seen in both the stomach and esophagus. Crohn's disease (CD) of the esophagus and stomach was confirmed. Anti-tumor necrosis factor α (TNFα) was started. He gained 2 kg in two weeks, and his chest symptoms gradually subsided, suffering from brief epigastric postprandial discomfort. At the time of his third anti-TNFα injection, he was free of his initial life-threatening symptoms; he gained enough weight to reach his original body weight.
A recent study on pediatric inflammatory bowel disease revealed that even though esophageal CD prevalence is increasing worldwide, there are very few reports of CD in the esophagus and stomach in Korea.
1 A retrospective analysis of 24 esophageal CD patients of the Mayo Clinic (12–60 years old) showed the major lesion site was the mid or distal part, and only 13% showed deep ulcerations.
2 Our case had severe esophageal deep ulcers in the proximal and mid sections.
A representative endoscopic finding of gastroduodenal CD is a bamboo-joint-like (BJL) appearance.
3 However, our patient had multiple aphthous lesions, not BJL appearance.
A very recent case report of ileocecal CD with esophageal involvement in a young woman showed almost the same symptoms seen in our patient.
4 Treatment with first line drugs and proton pump inhibitor (PPI) was successful; therefore, it was suggested that an esophageal CD should be considered in patients presenting with esophageal ulcer.
Treatment Guideline for severe esophagogastric CD by European Crohn's and Colitis Organization is PPI with or without systemic corticosteroid, and anti-TNFα.
5 Treatment with methotrexate or thiopurines was omitted from the guideline in 2017.
Ethics statement
The authors obtained approval from the Institutional Review Board (IRB) of Hanyang University Hospital (2017-01-062), and informed consent was waived by the IRB.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download