INTRODUCTION
Sarcopenia is an age-related disease described by a progressive loss of muscle mass and function. In addition, sarcopenia has its own International Classification of Diseases in the 10th revised Clinical Modification (ICD-10-CM). The assigned code is M62.84 and has been in use since October 1, 2016.
1 Since then, the number of sarcopenia studies has dramatically increased. Although the relationship between sarcopenia and osteoporosis is well recognized, most sarcopenia studies have focused on metabolic diseases, such as diabetes, obesity, cachexia, and some specific diseases, including chronic renal failure, congestive heart failure, and chronic obstructive pulmonary disease.
234567
The concept of osteosarcopenia is defined as patients with osteoporosis and sarcopenia.
89 The combined effect of sarcopenia and osteoporosis represents a serious problem in the elderly, because of their propensity for falls, ending in fragility fractures.
10 Yu et al.
11 reported that the fracture risk was increased by 3.5-fold in men with osteosarcopenia and was significantly higher than in sarcopenia and osteoporosis alone.
Hip fracture is considered to be a significant fracture as a result of osteoporotic fracture, due to the resulting high mortality, morbidity, and socioeconomic burden.
1213 In addition, hip fractures are known to be a prototype condition in patients with sarcopenia. Several epidemiological studies have reported the prevalence of sarcopenia in patients with hip fracture.
1415 However, the prevalence of osteosarcopenia and its clinical outcomes, including mortality in patients with hip fracture, have rarely been reported.
The purpose of the present study was to determine the prevalence of osteosarcopenia and the relationship of osteosarcopenia and mortality in a consecutive series of patients with hip fracture, with a minimum follow-up of 1-year.
METHODS
Between November 2011 and December 2014, all patients with a fresh hip fracture who were at least age 60 and admitted to our hospital, were eligible for this study. During the study period, 406 hip fracture patients age 60 and older were admitted to the study institution. Of these, 34 (8.1%) were excluded because there was no time to perform dual-energy X-ray absorptiometry (DXA) preoperatively due to the need for urgent surgical repair, 31 (7.3%) were excluded because of denial of examination and 17 (4.0%) were excluded due to incorporation, such as dementia, delirium, and depression. A total of 324 hip fracture patients were finally included in this study (
Fig. 1).
Fig. 1
Flow chart of study subjects.
DXA = dual-energy X-ray absorptiometry.

Body composition was measured by whole-body DXA (DPX-NT; GE Medical Systems Lunar, Madison, WI, USA). Bone mineral content (BMC), fat mass, and lean soft tissue mass were measured separately for each part of the body, including the arms and legs. The lean soft tissue masses of the arms and legs were almost equal to the skeletal muscle mass. As absolute muscle mass correlates with height, the skeletal muscle mass index (SMI) was calculated by the following formula:
which is directly analogous to body mass index (BMI); BMI is calculated by dividing weight by height squared (kg/m
2). Arm SMI was defined as arm lean mass (kg)/height
2 (m
2). Leg SMI was defined as leg lean mass (kg)/height
2 (m
2). Appendicular SMI was defined as the sum of the arm and leg SMIs. Serum 25-hydroxyvitamin D (25[OH]D) levels were assayed using a radioimmunoassay kit (SIEMENS Healthcare, Erlangen, Germany). Muscle strength was assessed by handgrip strength. The participant held a Jamar adjustable dynamometer (Asimow Engineering, Los Angeles, CA, USA) in their dominant hand with his/her arm fully extended at an angle of 30° with respect to the trunk, and the palm of the hand perpendicular to the shoulder line. Sarcopenia was defined according to the Asia Working Group for Sarcopenia (AWGS) criteria for low muscle strength (hand grip strength below 18 kg in women and below 26 kg in men) and low muscle mass (SMI below 5.4 kg/m
2 in women and below 7.0 kg/m
2 in men).
16
BMC and bone mineral density (BMD) at total femur, femoral neck, and lumber spine (L1–L4) sites were measured by trained technicians using DXA (Lunar Prodigy; GE Healthcare, Madison, WI, USA).
Osteoporosis was defined as a BMD 2.5 standard deviations (SDs) below the peak bone mass of a young, healthy, gender- and race-matched reference population according to the World Health Organization (WHO) diagnostic classification. The relation between BMD (T-score) and SMI was used for classification of osteosarcopenia (T-score ≤ −2.5 and low SMI), sarcopenia only (low SMI and T-score > −2.5), osteoporosis only (low T-score and high SMI), and normal (high T-score and high SMI).
Patients were followed up at 1, 3, 6, and 12 months postoperatively, and every 6 months thereafter. At each visit, patients were interviewed using a questionnaire that addressed their activity level. Activity levels were defined as follows: I, independent community ambulatory; II, community ambulatory with cane; III, community ambulatory with walker/crutches; IV, independent household ambulatory; V, household ambulatory with cane; VI, household ambulatory with walker/crutches, and VII, nonfunctional ambulatory. In the analysis, Koval's grade I, II, and III cases were also classified as ambulatory outdoors, whereas Koval's grade IV, V, VI, and VII cases were classified as housebound. American Society of Anesthesiologists (ASA) classifications were defined as follows: I, healthy; II, mild systemic disease; III, severe systemic disease that is not incapacitating; IV, severe, incapacitating disease that is a constant threat to life; V, moribund and not expected to live more than 24 hours or without surgery; VI, brain-dead organ donor.
17
Patients unable to return for a follow-up evaluation were interviewed using a questionnaire by telephone. The follow-up evaluations were made taking care to interview the same caregiver who had been previously interviewed during the patient's hospitalization. This clinical information was collected by 1 orthopedic surgeon and 2 nurses. In all, 342 patients completed the follow-up evaluation by telephone interview.
Mortality was identified from hospital records or by interviewing a member of the family of the patient involved. We analyzed the morbidity in patients, who were still alive until the latest follow-up, which was performed at 6 to 12 postoperative months.
Statistical analysis
The age, gender, BMI, ASA score (≥ grade 3), Koval (≥ grade 4), type of fracture (femur neck and intertrochanter), number of deaths at the minimum 1-year follow-up, type of surgery (arthroplasty, internal fixation, and conservative treatment), and 25(OH)D were assessed to determine the relationship between these variables and between groups (normal, osteoporosis only, sarcopenia only, and osteosarcopenia). The osteosarcopenia group and other groups (normal, osteoporosis only, sarcopenia only) were compared in terms of the mortality rate at the minimum 1-year follow-up and the related risk factors by gender difference.
We used a χ2 test to assess differences in categorical variables and a t-test or analysis of variance (ANOVA) test for numerical variables. All reported P values were 2-sided, and a P value of < 0.05 was used to determine significance.
To best determine the risk factors of mortality for hip fracture in patients with osteosarcopenia, multivariate analysis was performed. Variables that had a P value of < 0.20, age, BMI, type of surgery, and 25(OH)D in women, and age, BMI, ASA, Koval, and 25(OH)D in men were included in the multivariate model. Cox proportional hazard models were used to calculate the crude hazard ratios (HRs), adjusted HRs, and 95% confidence intervals (CIs). All statistical tests were 2-tailed, and P < 0.05 was considered significant. Statistical analyses were carried out using SPSS for Windows software (version 22.0; SPSS Inc., Chicago, IL, USA). A P value of < 0.05 was considered significant.
Ethics statement
The design and protocol of this retrospective study were approved by the Institutional Review Board of Chung-Ang University Hospital (C2016212 [1955]). Informed consent was waived by the board.
RESULTS
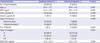
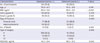
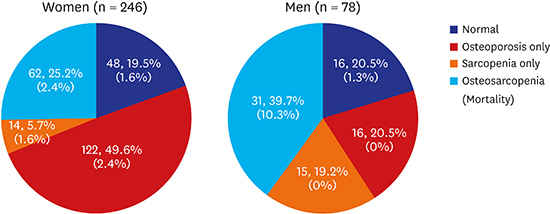
Of the 324 patients with hip fracture (78 men and 246 women), the prevalence of each category (normal, osteoporosis only, sarcopenia only, and osteosarcopenia) were 19.8%, 42.6%, 9.0%, and 28.7%, respectively. The age (
P < 0.001), gender (
P < 0.001), BMI (
P < 0.001), ASA (≥ grade 3;
P = 0.012), Koval activity (≥ grade 4;
P = 0.035), and number of deaths (
P = 0.050) were significantly different between each category, respectively. The demographic data of the patients are shown in
Table 1. The prevalence of each category in men and women (normal, osteoporosis only, sarcopenia only, and osteosarcopenia) were 20.5%, 19.5%, 20.5%, and 49.6%, and 19.2%, 5.7%, 39.7%, and 25.2%, respectively (
Fig. 2).
Table 1
Demographic data of patients classified by status of each categories

|
Characteristics |
Total |
Normal |
Osteoporosis only |
Sarcopenia only |
Osteosarcopenia |
P value |
|
No. of patients |
324 |
64 (19.8) |
138 (42.6) |
29 (9.0) |
93 (28.7) |
- |
|
Age, yr |
77.8 ± 9.7 |
73.8 ± 8.0 |
80.3 ± 8.7 |
76.9 ± 6.1 |
79.5 ± 8.5 |
< 0.001 |
|
Female gender |
246 (75.9) |
48 (74.3) |
122 (88.7) |
14 (48.5) |
62 (66.7) |
< 0.001 |
|
BMI, kg/m2
|
22.2 ± 3.8 |
25.1 ± 3.4 |
22.1 ± 3.6 |
21.8 ± 2.9 |
20.7 ± 3.5 |
< 0.001 |
|
ASA (≥ grade 3) |
275 (84.9) |
46 (71.6) |
120 (87.3) |
25 (84.8) |
84 (90.3) |
0.012 |
|
Koval (≥ grade 4) |
64 (19.8) |
3 (5.4) |
30 (21.8) |
5 (18.2) |
26 (28.0) |
0.035 |
|
Type of fracture |
|
|
|
|
|
0.126 |
|
Femoral neck |
119 (38.6) |
27 (43.2) |
42 (32.4) |
16 (54.5) |
36 (38.7) |
|
Intertrochanteric |
205 (61.4) |
37 (56.8) |
96 (67.6) |
13 (45.5) |
57 (61.3) |
|
No. of death |
29 (9.0) |
5 (7.8) |
7 (5.1) |
3 (10.3) |
14 (15.1) |
0.050 |
|
Type of surgery |
|
|
|
|
|
0.434 |
|
A |
210 (64.8) |
39 (61.0) |
85 (61.6) |
17 (58.6) |
67 (72.0) |
|
IF |
107 (33.0) |
23 (35.9) |
50 (36.2) |
12 (41.4) |
24 (25.8) |
|
CT |
7 (2.1) |
2 (3.1) |
3 (2.2) |
0 (0) |
2 (2.2) |
|
25(OH)D, ng/mL |
15.4 ± 10.8 |
16.1 ± 9.4 |
14.1 ± 9.5 |
15.7 ± 10.9 |
16.6 ± 12.9 |
0.513 |
Fig. 2
Prevalence of osteosarcopenia and 1-year mortality according to gender.
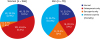
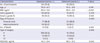
In total, 9.0% (29 of 324) of patients died during the 1-year follow-up. A 1-year mortality of osteosarcopenia (15.1%) was higher than that of other groups (normal: 7.8%, osteoporosis only: 5.1%, sarcopenia only: 10.3%) (
P = 0.050). In men, a 25.8% mortality rate at the 1-year follow-up in the osteosarcopenia group was significantly higher than the 2.1% in the non-osteosarcopenia group (
P = 0.001) (
Table 2). However, in women, there was no difference in mortality rate at the 1-year follow-up in both groups (
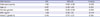
Table 3). Osteosarcopenia after adjusting for covariates had a 1.8 times higher mortality rate than non-osteosarcopenia (HR, 1.84; 95% CI, 0.69–4.92) (
Table 4).
Table 2
Characteristics of participants classified by the presence of osteosarcopenia in men
|
Characteristics |
Osteosarcopenia (−) |
Osteosarcopenia (+) |
P value |
|
No. of participants |
47 (60.3) |
31 (39.7) |
- |
|
Age, yr |
75.0 ± 7.2 |
78.8 ± 8.8 |
0.107 |
|
BMI, kg/m2
|
21.4 ± 3.0 |
21.4 ± 2.9 |
0.915 |
|
ASA (≥ grade 3) |
42 (84.8) |
30 (95.2) |
0.236 |
|
Koval (≥ grade 4) |
5 (12.1) |
11 (38.1) |
0.025 |
|
Type of fracture |
|
|
0.455 |
|
Femoral neck |
16 (33.3) |
7 (23.8) |
|
Intertrochanteric |
31 (66.7) |
23 (76.2) |
|
No. of death |
1 (2.1) |
8 (25.8) |
0.001 |
|
Type of surgery |
|
|
0.813 |
|
A |
32 (68.1) |
22 (70.9) |
|
IF |
12 (25.5) |
8 (25.8) |
|
CT |
3 (6.4) |
1 (3.2) |
|
25(OH)D, ng/mL |
17.3 ± 10.3 |
13.3 ± 9.7 |
0.199 |
Table 3
Characteristics of participants classified by the presence of osteosarcopenia in women
|
Characteristics |
Osteosarcopenia (−) |
Osteosarcopenia (+) |
P value |
|
No. of participants |
184 (74.8) |
62 (23.9) |
|
|
Age, yr |
79.0 ± 8.7 |
79.6 ± 8.8 |
0.741 |
|
BMI, kg/m2
|
23.0 ± 3.9 |
20.3 ± 3.5 |
< 0.001 |
|
ASA (≥ grade 3) |
162 (87.8) |
56 (91.7) |
0.509 |
|
Koval (≥ grade 4) |
30 (16.3) |
12 (19.4) |
0.655 |
|
Type of fracture |
|
|
0.990 |
|
Femoral neck |
71 (38.8) |
24 (38.9) |
|
Intertrochanteric |
113 (61.2) |
38 (61.1) |
|
No. of death |
14 (7.6) |
6 (9.7) |
0.524 |
|
Type of surgery |
|
|
0.896 |
|
A |
109 (59.2) |
45 (72.6) |
|
IF |
73 (39.7) |
16 (25.8) |
|
CT |
2 (1.1) |
1 (1.6) |
|
25(OH)D, ng/mL |
14.3 ± 9.4 |
18.5 ± 15.5 |
0.043 |
Table 4
Cox proportional hazard models of the potential risk factors for 1-year mortality
|
Risk factors |
HR |
95% CI |
P value |
|
Osteosarcopenia |
1.84 |
0.69–4.92 |
0.023 |
|
Age, yr |
0.97 |
0.92–1.03 |
0.301 |
|
Female gender |
0.88 |
0.29–2.59 |
0.818 |
|
BMI, kg/m2
|
1.06 |
0.92–1.21 |
0.444 |
|
Koval (≥ grade 4) |
0.46 |
0.70–5.01 |
0.126 |
DISCUSSION
Although hip fracture is an important phenotype to study effect of sarcopenia, only the prevalence of sarcopenia in patients with hip fracture has been reported. Recently, the concept of interaction of bone and muscle was generalized, and as such osteosarcopenia is raising interest in patients with hip fracture. This study has demonstrated that the prevalence of osteosarcopenia after adjusting for covariates had a 1.8 times higher mortality rate than non-osteosarcopenia (HR, 1.84; 95% CI, 0.69–4.92). To the best of our knowledge, there have been no previous studies evaluating an association between osteosarcopenia and mortality in patients with hip fractures.
To date, studies regarding the prevalence of osteosarcopenia have been rare. Drey et al.
18 performed a randomized, controlled training study to investigate patient physical performance and the bone metabolism of osteosarcopenia in 68 prefrail, community-dwelling older adults (age range, 65–94 years). They found that the prevalence of osteosarcopenia was 27.9% (19/68) and osteosarcopenic participants showed significantly reduced hand grip strength, increased chair rising time, and the static transfer switch (STS) power time, as well as significantly increased bone turnover markers. Huo et al.
19 identified a phenotype of osteosarcopenia in 680 older individuals (mean age: 79 years, 65% women) with a history of falling, in a cross-sectional study. They reported that the prevalence of osteosarcopenia was 37% (258 of 680). They found that osteosarcopenia patients are older, mostly women, are at high risk for depression and malnutrition, have a BMI lower than 25, and showed a higher prevalence of peptic disease, inflammatory arthritis, maternal hip fracture, history of atraumatic fracture, and impaired mobility. In this study, we found a 28.7% (39.7% in men and 23.9% in women) prevalence of osteosarcopenia, similar to previous studies. However, because the patient demographic and the definition of osteosarcopenia in this study is totally different to 2 previous studies, a direct comparison between studies might be impossible. Nevertheless, the difference of prevalence of osteosarcopenia, and the combined effect of sarcopenia and osteoporosis are known to give rise to serious problems, such as fall and fragility fractures in elderly patients.
Mortality at the one-year follow-up period was 15.1% in the osteosarcopenia group, almost twice the 9.0% mortality observed in the total patient group. After adjustment, osteosarcopenia in men had a 1.8 times higher mortality rate than non-osteosarcopenia men (HR, 1.84; 95% CI, 0.69–4.92). These findings are much higher than mortality in patients with sarcopenia. Yalcin et al.
20 performed a prospective observational study using 170 older nursing home residents. They found that the prevalence of sarcopenia and severe sarcopenia were 29% and 25.4%, respectively. A total of 44% of sarcopenic participants died, whereas 15% of participants without sarcopenia died after 2-year of follow-up (
P < 0.001). After adjusting for confounding factors, sarcopenia was associated with all-cause mortality among older nursing home residents (HR, 2.38; 95% CI, 1.04–5.46;
P = 0.039). In addition, Landi et al.
21 performed a 7-year follow-up study using 364 frail elderly people living in the community and reported that participants with sarcopenia had a higher risk of death for all causes, compared with non-sarcopenic subjects (HR, 2.32; 95% CI, 1.01–5.43).
This study has several limitations. First, this was a retrospective single-center study, and selection bias may have been introduced when we chose the hip fracture patient subjects. Second, 9.0% of mortality at the 1-year follow-up period in this study was lower than the 16% mortality observed in the general population.
22 We think that the reason for this discrepancy might be related with the patients' general condition. In order to examine whole body densitometry, patients condition should be generally good and cooperative due to long-examination times. Because of these reasons, 51 patients were excluded. Therefore, survival rate in this study group is better than reported data. Third, the severity of sarcopenia could not be evaluated because a gait speed test was not possible prior to hip fracture surgery. Fourth, we could not confirm high prevalence or mortality in patients with osteosarcopenia. However, a previous study reported the high prevalence of osteosarcopenia in women.
19 A larger sample size might be essential to confirm the effectiveness of osteosarcopenia in patients with hip fracture. Finally, there might be confounding factors in measurements of body composition of leg origination from the hip fracture.
In conclusion, this is the first study evaluating the relationship between mortality and osteosarcopenia in patients with hip fracture. We demonstrate that the prevalence of osteosarcopenia is not rare and is associated with a higher mortality than non-osteosarcopenia at a minimum 1-year follow-up period.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download