INTRODUCTION
In the emergency department (ED), trauma is a major cause of death.
12 Half of deaths due to trauma occur within 24 hours of admission.
3 Among the several causes of death in the early phase of trauma, exsanguination is as prominent as central nervous system injury.
4 It has been reported that 16%–44% of patients with trauma developed disseminated intravascular coagulation (DIC) on ED arrival, depending on the diagnostic criteria.
56 DIC increases proinflammatory cytokines, inhibits the anticoagulant pathway, and sustains a systemic inflammatory response in trauma.
7 Patients with DIC had a higher risk for mortality and received more transfusions than those with non-DIC in the early phase of trauma.
6 DIC at early phase of trauma continues into the late phase of trauma, eventually leading to multiple organ dysfunction syndrome.
67 Therefore, early diagnosis of DIC and rapid intervention for DIC patients is important to decrease mortality in the early phase of trauma.
For a diagnosis of DIC, the International Society on Thrombosis and Hemostasis (ISTH) score is the most frequently used diagnostic criteria.
8 The ISTH score facilitates an accurate diagnosis of DIC in trauma, and DIC diagnosed by ISTH has been associated with mortality or massive transfusions in trauma.
9 The Korean Society on Thrombosis and Hemostasis (KSTH) score has also been useful in diagnosing DIC in critically ill patients.
10 In patients with complicated sepsis, the KSTH score showed a good prognostic performance for intensive care unit (ICU) mortality.
11 However, most previous studies have focused on the relationships between the two scoring systems and prognosis in critically ill patients, whereas comparative prognostic performance analysis of these two scoring systems regarding trauma patients has been lacking. In the present study, we aimed to analyze and compare the prognostic performances of the ISTH and KSTH scores in the early phase of trauma.
METHODS
Study design and population
We performed a retrospective observational study involving patients with severe trauma, at Chonnam National University Hospital, Gwangju, Korea, admitted between January 2012 and December 2015. Severe trauma was defined as having an injury severity score (ISS) greater than 16.
12 The following exclusion criteria were applied: age less than 18 years; lack of DIC laboratory tests (platelet counts, activated partial thromboplastin time [aPTT], prothrombin time, fibrinogen level, fibrin/fibrinogen degradation product [FDP] level, and D-dimer level) within 1 hour of admission; specific trauma mechanisms, such as drowning or hanging; cardiac arrest following trauma; conditions resulting in coagulation abnormalities, such as hematologic malignancy, pregnancy, severe hepatic dysfunction, and current use of anticoagulant agents; and missing data.
Data collection
The following variables were obtained for each patient: age, sex, mechanism of trauma, time interval from accident to arrival at our ED, systolic arterial blood pressure (mmHg) on admission, respiratory rate on admission, initial Glasgow Coma Scale (GCS) data, laboratory data on admission (pH, PaCO2, base excess, white blood cell count, hemoglobin, platelet count, aPTT, international normalized ratio of prothrombin time [PT-INR], fibrinogen level, FDP level, and D-dimer level), amounts of transfusion packed red blood cells (PRCs), fresh frozen plasma (FFP), and platelet concentrates (PCs) during the first 24 hours after trauma, and 24-hour mortality.
The revised trauma score (RTS) was calculated based on vital signs and the GCS. The Abbreviated Injury Scale (AIS) score and ISS were calculated on arrival. Massive transfusion was defined as transfusion of ≥ 10 units PRC from initial presentation in the ED to 24 hours after arrival. The ISTH and KSTH scores were calculated based on the data collected on admission. The primary outcome was 24-hour mortality and the secondary outcome was massive transfusion.
Statistical analysis
Continuous variables did not satisfy the normality test and are presented as median values with interquartile ranges (IQRs). Categorical variables are presented as frequencies and percentages. Differences between the two groups were tested using the Mann-Whitney U-test for continuous variables. The Fisher's exact test or χ2 test was used for comparison of categorical variables, as appropriate.
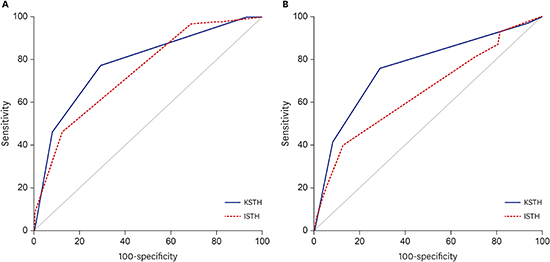
Receiver operating characteristics (ROCs) analysis was performed to examine the prognostic performance of the ISTH and KSTH scores for 24-hour mortality and massive transfusion. The comparison of dependent ROC curves was performed using the DeLong et al.'s method.
13
Multivariate analysis was used to estimate the prognostic impact of the ISTH and KSTH scores for 24-hour mortality and massive transfusion, after adjusting for relevant covariates. Then, the relationships between all measured independent variables and 24-hour mortality or massive transfusion were analyzed using a stepwise logistic regression analysis. The aPTT or fibrinogen level as continuous variables was entered at step 1. Step 2 included categorical variables for the aPTT and fibrinogen level. The aPTT was categorized as < 5 seconds and ≥ 5 seconds, defined according to the KSTH score.
14 The fibrinogen level was categorized as < 1.0, 1.0–1.5, and > 1.5 g/L, defined according to the KSTH and ISTH scores.
14 All variables with a
P value less than 0.1 on univariate analysis were included in the logistic regression. Backward selection was used to achieve the final model.
Data were analyzed using PASW/SPSS™ software, version 18 (IBM Inc., Chicago, IL, USA). The ROC curves were calculated and compared using MedCalc version 16.1 (MedCalc Software bvba, Ostend, Belgium). A two-sided significance level of 0.05 was used for statistical significance.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Chonnam National University College of Medicine (Reg. No. CNUH-2017-177). Informed consent was waived due to the retrospective nature of the study by the board.
DISCUSSION
In the present study, the KSTH score showed a higher performance than the ISTH score in predicting 24-hour mortality and massive transfusion in severe trauma. Overt DIC, according to KSTH criteria only, was independently associated with 24-hour mortality in severe trauma. Furthermore, the KSTH score was independently associated with massive transfusion in severe trauma.
The ISS standardizes the severity of trauma as an anatomical finding.
12 Several studies have shown that the ISS value has been associated with mortality in trauma patients.
315 In a previous study, the ISS value was higher in patients who died within the first 24 hours than in survivors, which is consistent with this study.
3 However, the ISS value of that study was higher than in our study, and we consider that the proportion of non-survivors with severe head injury was high in that previous study.
3 Another scoring system is the RTS, created by physiologic findings based on GCS, respiratory rate, and systolic blood pressure.
16 Orhon et al.
15 demonstrated that RTS values of survivors were higher than in non-survivors, which is similar to the present study.
In this study, patients with a penetrating injury were more massively transfused than those with a blunt injury in multivariate analysis (OR, 5.821; 95% CI, 1.932–17.538). In one retrospective study in which 91% of patients had penetrating injuries, damage to the inferior vena cava and aorta that could cause massive bleeding occurred in 58%.
17 In the same study, hemorrhagic shock was the most common cause of death.
17 Another study showed that penetrating injury was related to severe hypovolemic shock, and required early surgical bleeding control.
18
Our study showed that the ISTH score on admission was associated with specific outcomes in early phase of trauma. Hayakawa et al.
6 showed that overt DIC diagnosed by ISTH criteria led to higher mortality and received more transfusion than non-DIC, similar to the present study. In one retrospective study, non-survivors had a higher ISTH score and more overt DIC diagnosed by the ISTH score than survivors.
9 On the other hand, the ISTH score showed poor sensitivity in predicting mortality in critically ill patients,
19 which we considered, was related to the ISTH score being focused on the fibrinolysis associated with thrombocytopenia. Furthermore, in trauma, platelet counts remain at a moderate level during the first 24 hours, after which they decrease rapidly.
7 Therefore, the ISTH score may be less effective for the prediction of mortality in early phase of trauma.
The KSTH score was first proposed in 1993 and is used for diagnosis of DIC in Korea.
10 Although the KSTH score is not internationally accepted, it provides a clearer diagnosis of DIC, compared to the ISTH score.
1020 Two retrospective studies have reported that concordance rates between the KSTH score and the ISTH score were between 84.7% and 89.5%.
1020 In patients with sepsis, the KSTH score on day 1 after admission was independently significantly associated with overall ICU mortality.
11 In addition, the KSTH score may be easier to use because it has no weighted score, in contrast to the ISTH score.
14
In the present study, the platelet count was independently associated with 24-hour mortality in trauma. Several studies have shown that a low platelet count can be associated with specific outcomes in trauma.
2122 McQuilten et al.
21 demonstrated that a platelet count < 100 × 10
9/L was associated with in-hospital mortality more often than a platelet count > 150 × 10
9/L in severe trauma. In one retrospective multicenter study, the platelet count was lower in patients who had died within 24 hours or who had received massive transfusion than in those not in these categories.
22 In the same study, the platelet count was maintained above 100 × 10
9/L in the early phase of trauma, which is similar to the present study.
22 In the KSTH and ISTH scores, the cut-off value of platelet count is 100 × 10
9/L.
14 Therefore, we postulate that the platelet count of these two scores is too low to be appropriate for prognosis in early phase of trauma.
Many studies have revealed that D-dimer levels of fibrin degradation product can be associated with outcome in trauma.
922 Sawamura et al.
9 showed that the D-dimer level was higher in non-survivors than in survivors in the early phase of trauma. In one retrospective study, a high D-dimer level on admission was associated with 24-hour mortality or a requirement for massive transfusion.
22 However, the D-dimer levels presented by two studies
922 were higher than 1 or 5 mg/L of the D-dimer level suggested by the KSTH or ISTH score, respectively.
14 We consider that a high D-dimer level reflects the hyper-fibrinolytic state of trauma, unlike other medical conditions.
In this study, when aPTT was categorized as < 5 seconds and ≥ 5 seconds, aPTT was not associated with 24-hour mortality in multivariate analysis. Furthermore, aPTT was not independently associated with massive transfusion in trauma. In one study, aPTT showed 50% sensitivity to coagulopathy in acute trauma.
23 The authors considered that factor VIII, as an acute phase reactant, was high in acute trauma and that aPTT may be shortened by elevated factor VIII activity.
23 In the same study, 70% of patients with a false negative aPTT showed elevated factor VIII activity.
23
In the present study, multivariate analysis revealed that a fibrinogen level ≤ 1.5 g/L was an independent predictor for mortality. Several studies have also shown that fibrinogen levels ≤ 1.5 g/L are associated with a poorer outcome in trauma.
521 Hayakawa et al.
5 showed that the development of DIC is associated with a fibrinogen level ≤ 1.5 g/L, and that massive transfusions are performed more often in the DIC group. McQuilten et al.
21 demonstrated that a fibrinogen level ≤ 1.5 g/L is associated with increased in-hospital mortality, massive transfusion, and longer time in ICU.
In the KSTH score, the cut-off value of the fibrinogen level is 1.5 g/L and the proportion of the fibrinogen level is 25% of the total score.
14 On the other hand, in the ISTH score, the cut-off value of the fibrinogen level is 1.0 g/L and the proportion of the fibrinogen level is 12.5% of total score.
14 Therefore, the KSTH score gives more weight to the fibrinogen level than the ISTH score. Furthermore, the ISTH score does not consider the severity of patients with fibrinogen levels of 1.0–1.5 g/L. In this matter, the KSTH score estimates the severity of trauma more accurately than the ISTH score.
The present study has several limitations. First, it was retrospective and single centered, implying the need for further studies including larger sample sizes, multiple centers, and a prospective design to assess generalizability and causation rather than associations. Second, 630 patients with severe trauma were excluded because DIC laboratory tests were not completed within 1 hour of admission. The reasons for this included delayed blood sampling due to resuscitation, re-sampling due to hemolysis, and the relative high cost of coagulation biomarkers. Third, ED arrival was significantly later for the survivor group than for the non-survivor group. We assumed that patients with more severe conditions were transferred more promptly to the ED. Finally, we could not ascertain mortality in patients who were transferred to another hospital within 24 hours after arrival, so the overall 24-hour mortality from trauma figures may have been less accurate.
In conclusion, the KSTH score has a better prognostic performance for outcome than the ISTH score in the early phase of trauma. Further prospective study would be required to confirm the results of the present study.








 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download