1. Hopps E, Noto D, Caimi G, Averna MR. A novel component of the metabolic syndrome: the oxidative stress. Nutr Metab Cardiovasc Dis. 2010; 20:72–77.

2. Iyer A, Fairlie DP, Prins JB, Hammock BD, Brown L. Inflammatory lipid mediators in adipocyte function and obesity. Nat Rev Endocrinol. 2010; 6:71–82.

3. Evans JL, Goldfine ID, Maddux BA, Grodsky GM. Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev. 2002; 23:599–622.

4. Hadjigogos K. The role of free radicals in the pathogenesis of rheumatoid arthritis. Panminerva Med. 2003; 45:7–13.
5. Augustin AJ, Kirchhof J. Inflammation and the pathogenesis of age-related macular degeneration. Expert Opin Ther Targets. 2009; 13:641–651.
6. Van der Velden U, Kuzmanova D, Chapple IL. Micronutritional approaches to periodontal therapy. J Clin Periodontol. 2011; 38:Suppl 11. 142–158.

7. Chapple IL. Potential mechanisms underpinning the nutritional modulation of periodontal inflammation. J Am Dent Assoc. 2009; 140:178–184.

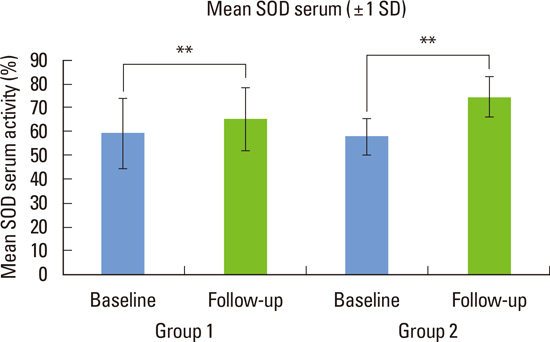
8. Baltacioglu E, Akalin FA, Alver A, Balaban F, Unsal M, Karabulut E. Total antioxidant capacity and superoxide dismutase activity levels in serum and gingival crevicular fluid in post-menopausal women with chronic periodontitis. J Clin Periodontol. 2006; 33:385–392.

9. Vural P, Akgul C, Canbaz M. Effects of menopause and tibolone on antioxidants in postmenopausal women. Ann Clin Biochem. 2005; 42(Pt 3):220–223.

10. Bednarek-Tupikowska G, Tupikowski K, Bidzinska B, Bohdanowicz-Pawlak A, Antonowicz-Juchniewicz J, Kosowska B, et al. Serum lipid peroxides and total antioxidant status in postmenopausal women on hormone replacement therapy. Gynecol Endocrinol. 2004; 19:57–63.

11. Brock GR, Butterworth CJ, Matthews JB, Chapple IL. Local and systemic total antioxidant capacity in periodontitis and health. J Clin Periodontol. 2004; 31:515–521.

12. Enwonwu CO, Ritchie CS. Nutrition and inflammatory markers. J Am Dent Assoc. 2007; 138:70–73.

13. Fredriksson M, Gustafsson A, Asman B, Bergström K. Hyper-reactive peripheral neutrophils in adult periodontitis: generation of chemiluminescence and intracellular hydrogen peroxide after in vitro priming and FcgammaR-stimulation. J Clin Periodontol. 1998; 25:394–398.

14. Petelin M, Pavlica Z, Ivanusa T, Sentjurc M, Skaleric U. Local delivery of liposome-encapsulated superoxide dismutase and catalase suppress periodontal inflammation in beagles. J Clin Periodontol. 2000; 27:918–925.

15. Chapple IL. Oxidative stress, nutrition and neutrogenomics in periodontal health and disease. Int J Dent Hyg. 2006; 4:Suppl 1. 15–21.

16. Chapple IL, Milward MR, Ling-Mountford N, Weston P, Carter K, Askey K, et al. Adjunctive daily supplementation with encapsulated fruit, vegetable and berry juice powder concentrates and clinical periodontal outcomes: a double-blind RCT. J Clin Periodontol. 2012; 39:62–72.

17. Page RC, Eke PI. Case definitions for use in population-based surveillance of periodontitis. J Periodontol. 2007; 78:7 Suppl. 1387–1399.

18. Loe H, Silness J. Periodontal disease in pregnancy: I. prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.

19. Silness J, Loe H. Periodontal disease in pregnancy: II. correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.

20. Tamaki N, Tomofuji T, Ekuni D, Yamanaka R, Yamamoto T, Morita M. Short-term effects of non-surgical periodontal treatment on plasma level of reactive oxygen metabolites in patients with chronic periodontitis. J Periodontol. 2009; 80:901–906.

21. Agnihotri R, Gaur S. Chemically modified tetracyclines: novel therapeutic agents in the management of chronic periodontitis. Indian J Pharmacol. 2012; 44:161–167.

22. Singh A, Sharma RK, Siwach RC, Tewari S, Narula SC. Association of bone mineral density with periodontal status in postmenopausal women. J Investig Clin Dent. 2013; 06. 14. [Epub].
http://dx.doi.org/10.1111/jicd.12047.

23. Singh N, Chander Narula S, Kumar Sharma R, Tewari S, Kumar Sehgal P. Vitamin E supplementation, superoxide dismutase status, and outcome of scaling and root planing in patients with chronic periodontitis: a randomized clinical trial. J Periodontol. 2014; 85:242–249.

24. Kim SC, Kim OS, Kim OJ, Kim YJ, Chung HJ. Antioxidant profile of whole saliva after scaling and root planing in periodontal disease. J Periodontal Implant Sci. 2010; 40:164–171.

25. Berger MM, Baines M, Raffoul W, Benathan M, Chiolero RL, Reeves C, et al. Trace element supplementation after major burns modulates antioxidant status and clinical course by way of increased tissue trace element concentrations. Am J Clin Nutr. 2007; 85:1293–1300.

26. Wang Y, Yang M, Lee SG, Davis CG, Kenny A, Koo SI, et al. Plasma total antioxidant capacity is associated with dietary intake and plasma level of antioxidants in postmenopausal women. J Nutr Biochem. 2012; 23:1725–1731.

27. Huang W, Glass CK. Nuclear receptors and inflammation control: molecular mechanisms and pathophysiological relevance. Arterioscler Thromb Vasc Biol. 2010; 30:1542–1549.

28. Rizvi M, Pathak D, Freedman JE, Chakrabarti S. CD40-CD40 ligand interactions in oxidative stress, inflammation and vascular disease. Trends Mol Med. 2008; 14:530–538.

29. Opara EC, Rockway SW. Antioxidants and micronutrients. Dis Mon. 2006; 52:151–163.

30. Bozkurt S, Arikan DC, Kurutas EB, Sayar H, Okumus M, Coskun A, et al. Selenium has a protective effect on ischemia/reperfusion injury in a rat ovary model: biochemical and histopathologic evaluation. J Pediatr Surg. 2012; 47:1735–1741.
31. Chapple IL, Milward MR, Dietrich T. The prevalence of inflammatory periodontitis is negatively associated with serum antioxidant concentrations. J Nutr. 2007; 137:657–664.
32. Linden GJ, McClean KM, Woodside JV, Patterson CC, Evans A, Young IS, et al. Antioxidants and periodontitis in 60-70-year-old men. J Clin Periodontol. 2009; 36:843–849.

33. Kushiyama M, Shimazaki Y, Murakami M, Yamashita Y. Relationship between intake of green tea and periodontal disease. J Periodontol. 2009; 80:372–377.
34. Fridovich I. Superoxide anion radical (O2-.), superoxide dismutases, and related matters. J Biol Chem. 1997; 272:18515–18517.
35. Wei D, Zhang XL, Wang YZ, Yang CX, Chen G. Lipid peroxidation levels, total oxidant status and superoxide dismutase in serum, saliva and gingival crevicular fluid in chronic periodontitis patients before and after periodontal therapy. Aust Dent J. 2010; 55:70–78.

36. Misaki H, Suzuki M, Yoshie H, Hara K. The effect of superoxide dismutase on the inflammation induced by periodontal pathogenic bacteria and wound healing of gingival incision. Nihon Shishubyo Gakkai Kaishi. 1990; 32:93–110.

37. Shingu M, Takahashi S, Ito M, Hamamatu N, Suenaga Y, Ichibangase Y, et al. Anti-inflammatory effects of recombinant human manganese superoxide dismutase on adjuvant arthritis in rats. Rheumatol Int. 1994; 14:77–81.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download