The major cause of hemorrhagic fever with renal syndrome (HFRS) in Korea is Hantaan virus. The vector for human infection is the rodent Apodemus agrarius, with rodent excrement entering the human respiratory system by aerosol transmission. It had been thought that there were two peak seasons throughout the year. The seeding season, from May to July, is the minor peak season; the harvest season, from October to December, when the ground is disturbed and a lot of dust is generated, resulting in an increase in incidence, is the major peak season [1]. However, according to infectious diseases statistics from the Korea Centers for Disease Control & Prevention (KCDC), since 2002, although HFRS cases have occurred throughout the year in Korea, the majority of cases have occurred during the major peak season from October to December, and the number of cases in the minor peak season from May to July has been gradually decreasing [2]. A study by Park et al. showed the same results, also reporting that there was no seasonal variation in Yeoncheon especially between 2002 and 2016 [3].
In Korea, areas with particularly high HFRS incidence, of over 5.0 persons per 100,000, were Paju, Yeoncheon, Pocheon, Yeoju, and Yangju in Gyeonggi province, Cheorwon, Hwacheon, Pyeongchang, Hoengseong, Yangyang, and Gangneung in Gangwon Province, Cheongju, Jincheon, Goesan, Eumseong, and Chungju in Chungcheongbuk province, and Yecheon, Andong, and Mungyeong in Gyeongsangbuk province [4]. Of these, Yeoncheon is unique as northernmost region, located in the northern part of Gyeonggi province.
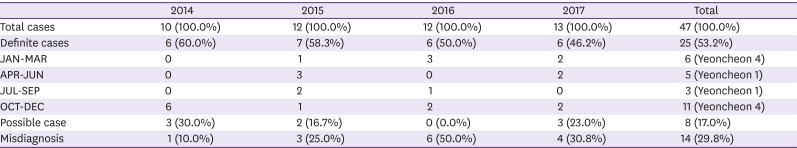
The 760-bed university hospital where the author works in Uijeongbu receives the majority of severe patients from Yeoncheon and Pocheon in the northern part of Gyeonggi province, and from the adjacent Donducheon, due to its geographical characteristics. At this hospital, I reviewed a total of 47 cases of HFRS, which are reported mandatorily as cases of a legally designated infectious disease, between 2014 and 2017.
Clinical diagnosis was prioritized over consistency with the reporting criteria for infectious diseases. Specifically, patients whose clinical presentation and serological test results were both consistent with HFRS were classified as a ‘definite case’, patients who were difficult to diagnose with HFRS based on both clinical presentation and serological test results were classified as a ‘misdiagnosis’, and patients who could be classified as neither a ‘definite case’ nor a ‘misdiagnosis’ were considered a ‘possible case’ (Table 1). We examined the antibody titers for 25 patients classified as a ‘definite case’; among 18 patients who underwent antibody (AB) tests once, the results were 1:2,560 for 4 patients, 1:1,280 for 6 patients, 1:640 for 3 patients, 1:320 for 1 patient, 1:160 for 2 patients, and 1:80 for 2 patients. Among 7 patients who underwent serial follow-up, 3 patients were initially negative but progressed to a positive result of 1:160 (1 person, 4-day interval), 1:320 (1 person, 4-day interval), and 1:1,280 (1 person, 5-day interval), while 4 patients showed an increase from an initial titer of 1:80 to a later titer of 1:160 (1 person, 4-day interval), 1:320 (2 persons, both 9-day intervals), and 1:1,280 (1 person, 5-day interval). Among 14 patients classified as a ‘misdiagnosis’, apart from 1 patient who was negative in two tests performed at a 4-day interval, the remaining 13 patients only underwent the antibody titer test once. The results were negative for 3 patients, 1:80 for 9 patients, and 1:160 for 1 patient (who also showed a Tsutsugamushi Ab titer of 1:1,280).
The proportion of reported cases classified as a ‘misdiagnosis’ shows a gradually increasing trend, and in nationwide statistics from the KCDC, since 2011, the number of reports of ‘suspected cases’ has become much higher than that of ‘genuine cases’ [2], which suggests that the accuracy of diagnosis may be decreasing. Of the 25 ‘definite cases’, 10 (40%) occurred in Yeoncheon, and the percentage of these occurring in each quarter of the year, respectively, was 40%, 10%, 10%, and 40%, which differs from the results reported by Park et al. [3], of 17.7%, 21.0%, 25.8%, and 35.5%. The study period for these results was different, with my study conducted over the last 4 years, and Park et al. [3] investigating the 15 years from 2002 to 2016. In addition, as shown in Table 1, the mean proportion of ‘misdiagnoses’ among reported HFRS cases at Uijeongbu St. Mary's Hospital in the last 4 years is 29.8%, demonstrating that detailed chart review by a clinician is essential to accurately ascertain the incidence of HFRS. However, because we do not have data for 2002–2013, it is difficult to compare directly with the results of Park et al.
It is clear that minor epdiemics of HFRS are disappearing and cases are being reported throughout the year. However, it seems that there is still seasonal variation, with most cases in the northern part of Gyeonggi province occurring between October and December. Notably, in our investigation, 4 of the 6 ‘definite cases’ between January and March occurred in Yeoncheon. In order to accurately analyze seasonal variation, it will be necessary to study other endemic areas with a high HFRS incidence, in addition to Yeoncheon, specifically investigating patterns for ‘definite cases’. In addition, serial serology tests will be essential to confirm diagnoses.
References
1. Park JH, Yeh MH, Hwang YJ, Dixon KE. A case-control study of risk factors for hemorrhagic fever with renal syndrome in Korean soldiers. Korean J Epidemiol. 1994; 16:41–53.
2. Korean Center for Disease Control and Prevention (KCDC). Infectious disease portal. Major statistics. Accessed 20 August 2018. Available at: http://www.cdc.go.kr/npt/biz/npp/ist/simple/simplePdStatsMain.do?icdCd=C0015&icdgrpCd=03.
3. Park YH. Absence of a seasonal variation of hemorrhagic fever with renal syndrome in Yoencheon compared to nationwide Korea. Infect Chemother. 2018; 50:120–127. PMID: 29968979.
4. Korean Center for Disease Control and Prevention (KCDC). Epidemiology and management of vaccine preventable disease: hemorrhagic fever with renal syndrome. 5th ed. Cheongju: KCDC;2017. p. 481–495.
Table 1
HFRS cases in Uijeongbu St. Mary's Hospital from 2014 to 2017




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download