Abstract
Purpose
The purpose of this study was to evaluate the relationship between masseter muscle thickness, facial morphology, and mandibular morphology in Korean adults using ultrasonography.
Materials and Methods
Ultrasonography was used to measure the masseter muscle thickness bilaterally of 40 adults (20 males, 20 females) and was performed in the relaxed and contracted states. Facial photos and panoramic radiography were used for morphological analyses and evaluated for correlations with masseter muscle thickness. We also evaluated the correlations of age, body weight, stature, and body constitution with masseter muscle thickness.
Results
In the relaxing, the masseter was 9.8±1.3 mm in females and 11.3±1.2 mm in males. In the contracted state, it was 12.4±1.4 mm in females and 14.7±1.4 mm in males. Facial photography showed that bizygomatic facial width over facial height was correlated with masseter muscle thickness in both sexes in the relaxed state, and was statistically significantly correlated with masseter muscle thickness in males in the contracted state. In panoramic radiography, correlations were found between anterior angle length and posterior angle length and masseter muscle thickness in females, and between body length and posterior angle length, between anterior angle length and body length, between ramal length and body length, and between body length and condyle length in males.
Facial morphology is influenced by hard tissues such as bones and soft tissues such as muscles. Aside from tooth, bone is the hardest tissue in the body, but it has been reported that its form and image continuously change through the process of modeling and remodeling. Factors that can lead to a change in bone tissue form include electric stimulation, mechanical stimulation, hormones, and general diseases, and it is understood that bone tissue form is most affected by nearby soft tissues such as muscles.12 In his functional matrix theory, Moss claimed that the growth of bone tissues is affected by nearby soft tissues that work as a functional matrix.3 He claimed that muscles attached to the mandible affect the growth of the mandible and that the orbit affects the growth and development of the orbital bone.3456 Muscle function has a major impact on bone tissues, not only in the growth phase, but also in adulthood.4 For example, patients with sarcopenia have a higher risk of contracting osteoporosis and, likewise, after mandibular osteotomy the bone tissue in the mandible experiences re-deposition. Therefore, the evaluation of muscular shape and function is important in analyzing facial features as well as in analyzing related bone tissues.
However, the evaluation of facial soft tissues—in particular, muscles—has presented more technical difficulties than the evaluation of hard tissues. In other words, hard tissues can be analyzed for the morphology of facial bone through lateral radiography,78 and recently, it became easier to analyze the 3-dimensional skeletal morphology and features of the jaw due to the development of cone-beam computed tomography (CBCT).9 However, it is more difficult to assess soft tissues using radiography. While it is possible to measure the thickness and other characteristics of masticatory muscles through soft tissue imaging by computed tomography (CT), patient exposure to radiation is an added risk. Thus, CT is of limited value in performing common examinations. It is also possible to evaluate soft tissues through magnetic resonance imaging (MRI), but it is expensive and time-consuming; furthermore, the fact that MRI is a static imaging modality, not a dynamic one, makes it difficult to analyze the shape during muscle contraction and relaxation.10
There have been many recent attempts to apply ultrasonography in the dental field. Unlike CT and other imaging modalities that expose the patient to a clinically significant radiation dosage, ultrasonography does not pose the problem of radiation exposure and dynamic analysis is possible. It is also possible to assess the blood vessel flow and speed;11 this is, therefore, being attempted for a number of anatomical areas including the mastication muscles,12 salivary glands,13 and cervical lymph nodes.14 Applying ultrasonography to these assessments has several limitations. No oral probe suitable for dentists has been developed, the ultrasonographic signal cannot pass through hard tissues, and no method of probe application has been standardized, thus requiring a learning curve period for clinical application. Among measurements using ultrasonography (US), masticatory muscle thickness has been the most common type of analysis. Though masticatory muscle thickness measurement using US does not provide precise evaluations of masticatory force or muscular contractile force, the thickness of muscle displays a proportional relationship with muscular function and hence, several studies have attempted to analyze masticatory force indirectly through measurement of muscle thickness.81015161718 Masticatory muscles affect masticatory function and also play a major role in shaping the facial appearance. The masseter originates from the zygomatic arch, attaches to the masseteric tuberosity, and is located closer to the surface than other masticatory muscles, providing the advantage of being easier to assess. Researchers from many countries have published data measuring the masticatory muscle thickness of residents of their respective countries,81015161718 but few studies have investigated the average thickness of the masticatory muscles of Koreans or the relationship of such values with the facial morphology or the shape of the mandible.
The purpose of this study was to measure masticatory muscle thickness with ultrasonography and to evaluate its correlation with facial morphology and mandible shape to assess the impact of facial muscle thickness on bone tissues and facial morphology.
This study was approved by the institutional review board of the Dental Hospital of Yonsei University College of Dentistry (IRB No. 2-2015-0045). Over the period between December 10, 2015 and October 30, 2016, 40 volunteers (20 males, 20 females) were enrolled from among inpatients who visited the Department of Advanced General Dentistry Yonsei University College of Dentistry.
Subjects who met the following selection criteria were enrolled: 1) adults over 20 years of age 2) who did not have dental disease such as temporomandibular joint disorder, myofascial pain syndrome, or the like; 3) who had a Class I molar relationship; and 4) who had not received orthodontic treatment. Excluded were those whose masticatory muscles were abnormal or could not be measured due to congenital anomaly, trauma, or tumor. Images taken to measure the masseter muscle were acquired using an ultrasound scanner (E-CUBE 15EX, Alpinion Medical Systems, Seoul, Korea) and a linear probe (L3-12H, Alpinion Medical Systems, Seoul, Korea). The images were acquired in the following sequence: 1) The subjects were taken to a dark and quiet room, guided into an upright position, and examined by palpation to locate the masseter muscle. 2) The transducer was placed at the most prominent area of the masseter muscle at the same angle as the occlusal plane (Fig. 1). 3) During the scan, the masseter muscle was placed in a position where it was perpendicular to the mandible. 4) The mandible was clearly visible as a white (hyperechoic) line, and images were acquired upon adjusting the transducer to present myofascial regions as white lines under the cutaneous and subcutaneous fat layers (Fig. 2). A relaxed state was defined as when both cusps of the upper and lower teeth were gently occluded (Fig. 3A). A contracted state was defined as the maximum contraction of muscles when the upper and lower molars were forcefully occluded (Fig. 3B). Ultrasonographic images were acquired by 2 observers, who each took measurements at intervals of 5 minutes or more and repeated the measurements twice, with the subjects in a relaxed state and in a contracted state. The thickness of the masseter muscle was measured at the thickest points presented in the images (Fig. 3). The images were then displayed on a computer monitor using a computer program installed within the ultrasonographic device.
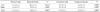
Facial photographs of the subjects were taken to assess facial morphology, using the following indicators: facial height (FH), bizygomatic facial width (BFW), and intergonial facial width (IGW), along with form of the face (FH/BFW, FH/IGW) (Fig. 4, Table 1).15
Panoramic radiography was performed to confirm the relationship between the mandibular morphology and the masseter muscle thickness, and the following points were identified: center point of the mandibular foramen (C), condyle (Con), coronoid (Cor), posterior gonion (PGo), anterior gonion (AGo), and mental foramen (MF) (Fig. 5, Table 1). However, since panoramic radiography has different magnification ratios in each region, the ratio of the length of each measurement item was used to overcome this problem (Table 2).19
The age, body weight (bw), and stature (s) of the subjects were measured, and body constitution (bw/s) was checked for correlation with masseter muscle thickness.
Measurement data were statistically analyzed using IBM SPSS 23.0 (IBM Corp., Armonk, NY, USA). Interclass and intraclass correlation coefficients were used to reduce the measurement error of masseter muscle thickness. The Student t test was performed to evaluate the gender and analysis of left/right measurements from ultrasonography and panoramic radiography. The Spearman rho test was performed to assess the correlations of facial photography, panoramic radiography, age, body weight, stature, and body constitution with masseter muscle thickness.
Both intraclass and interclass correlation coefficients showed that the masseter muscle thickness data measured twice by 2 observers were reliable (Table 3).20 The masseter muscle thickness measured by ultrasonography showed a significant difference according to gender (Table 4). No statistically significant differences were found between the left and right sides in mandibular morphology measured by ultrasonography or masseter muscle thickness parameters measured using panoramic radiography (Table 5).
In the facial morphology data, FH/IGW and the thickness of the masseter muscle measured in the relaxed state were found to be correlated in both sexes. In the contracted state, the thickness of the masseter muscle and the value of FH/IGW were also statistically significant in males (Table 6).
In mandibular morphology measured by panoramic radiography, a correlation was found between PGo-C/AGo-C and masseter muscle thickness in the relaxed state in females (Table 7). Con-C/MF-C and MF-C/Con-AGo also showed a significant correlation in the contracted state of the males, while PGo-C/MF-C, MF-C/AGo-C, and MF-C/Con-AGo showed a significant correlation in the relaxed state (Table 7).
The masseter muscle thickness measured by ultrasonography was 9.8 ±1.3 mm (relaxed state) and 12.4±1.4 mm (contracted state) in females, and 11.3±1.2 mm (relaxed state) and 14.7±1.4 mm (contracted state) in males. The facial width and height tended to become wider and lower as the masseter muscle thickened. Moreover, the values related to the mandibular angle were affected by the thickness of the masseter muscle.
It is known that the thickness of the masseter can be used to indirectly evaluate not only the shape of the face, but also masticatory function.1015 Measuring the thickness of the masseter was first attempted with ultrasonography by Kiliaridis and Kälebo (1991)15, Bakke et al., (1992),21 and Raadsheer et al. (1994).10 Masseter thickness values have been reported in patients with temporomandibular disorder,12 facial asymmetry,16 bone lesion,22 and foreign body removal.23 Because the masseter muscle is located on the surface layer, it can easily be measured by ultrasonography. However, ultrasound is not widely used as a method of measurement in this context. The most important reason for this is that the image quality varies according to the imaging technique applied. Even if an external measurement point and the method to assess it are defined, it is not easy to obtain ultrasonography images without accurate anatomical knowledge. Because the waves used in ultrasonography wave show continuously changing patterns, a great deal of experience performing ultrasonographic measurements is required. In addition, the image could change according to the force applied to the tissue and the unique anatomical characteristics of each patient. Therefore, assessment by ultrasonography may be more subjective than CT and MRI, both of which can produce a clearer image. For these reasons, ultrasound has not often been used. Recently, the clinical usage of ultrasound has become more common because of its non-ionizing image modality. In dentistry, ultrasound has been used to make simple measurements of the thickness of the masseter muscle, to evaluate the neck nodes24 and the submandibular13 and sublingual glands,25 and to perform follow-up examinations in cancer patients.26 The development of new intraoral ultrasound probes has made it possible to use ultrasonography for various dental applications including pulpal diagnosis, measuring gingival thickness,27 and performing vascular measurements.14
In this study, 2 observers discussed the anatomical characteristics and external measurement points in order to reduce errors in measurement. A pilot test was used to calibrate the measurement site and the pressure of the ultrasound probe. The reproducibility of the measurements was confirmed through this calibration.
This study examined the relationship between the thickness of the masseter muscle and various parameters of facial and mandibular morphology. Because the ratio of measurement values was assessed, a 1:1 measurement photograph was not necessary. A previous study9 measuring the length of the condyle, coronoid, and gonion centering on the mandibular foramen reported that they were closely related to deformity of the jaw. In our results, no statistically significant differences were found between the left and right sides on panoramic radiography in adults without a jaw deformity. This observation supports the finding of a previous report that the left and right sides of the mandible were symmetrical in patients without a jaw deformity. In addition, the masseter muscle is known to affect the mandibular angle. In this study, there was a correlation between masseter muscle thickness and gonion length. This result was in agreement with previously reported studies based on computed tomography. Therefore, the measurement of masseter muscle thickness using ultrasound is meaningful and quite accurate.1028
Previous studies have reported a correlation between masseter muscle thickness and facial morphology.1015 In our results, regardless of gender, patients with a lower facial height and larger intergonial width tended to have a thicker masseter muscle.
Kiliaridis and Kälebo (1991)15 and Raadsheer et al. (1996)10 reported no correlation between masseter muscle thickness and age. However, in the present study, masseter muscle thickness and age in the relaxed state showed a positive correlation in males. This might be related to ethnicity, heredity, and eating habits.
In this study, the masseter muscle thickness of males (relaxed state: 11.3±1.2 mm; contracted state: 14.7± 1.4 mm) was thinner than in the studies of Kubota et al. (relaxed state: 15.8±3.0 mm; contracted state: 16.7± 2.7 mm)8 and Satiroğlu et al. (relaxed state: 15.5±2.0 mm; contracted state: 17.2±2.1 mm).17 Furthermore, in females, the measurements (relaxed state: 9.8±1.3 mm; contracted state: 12.4±1.4 mm) were lower than those of Satiroğlu et al. (relaxed state: 12.1±1.9 mm)17 and Tircoveluri et al. (12.5±0.5 mm)18 in the relaxed state (Table 9). These results might originate from variation in eating habits depending on ethnicity and age.
The limitations of this study were the small sample size and lack of comparison among various age groups. The correlation between the masseter muscle thickness and the masticatory force could not be assessed. It should be noted that computerized methods of imaging masticatory force and distribution, such as the T-scan, have only recently been introduced. It would be worthwhile to develop an objective method for measuring the relationship between bite force and masseter muscle characteristics, and to perform a clinical study using that method. In addition, the direction and length of the masseter muscle differ according to the position of the jaw. Therefore, it is necessary to consider the direction and length when we evaluate the thickness of the masseter muscle. That is, in the case of a class II patient with a short ramal height, the muscle length and the force may be the same as those of a patient with a longer ramal height, the masseter muscle thickness may be greater due to its short length. Despite the limitations of this study, it is meaningful because it provides data on muscle thickness and facial features using ultrasonography.
In conclusion, the thickness of the masseter muscle measured by ultrasound was found to be associated with facial and mandibular morphology in men. Ultrasonography is a simple and accessible technique for measuring masseter muscle thickness.
Figures and Tables
Fig. 2
Anatomical structure of masseter muscle in an ultrasound image. (A) skin layer; (B) fat layer; (C) masseteric fascia; (D) masseter muscle.

Fig. 3
Cross-sectional view of an ultrasound image. A. Relaxed state. B. Contracted state. The yellow dotted line is the masseter muscle thickness.

Fig. 4
Schematic diagram of reference points and measurements of length on a facial photograph. Bizygomatic facial width (BFW); intergonial facial width (IGW); facial height (FH).

Fig. 5
Schematic diagram of reference points and measurements of length on a panoramic radiograph. Center point of mandibular foramen (C); condyle (Con); coronoid (Cor); posterior gonion (PGo); anterior gonion (AGo); mental foramen (MF).

Table 1
Definition of facial photograph and panoramic radiography measurements using the reference points

Table 2
Definition and description of facial morphology and mandibular morphology using the measurement items

References
1. Ingervall B, Bitsanis E. A pilot study of the effect of masticatory muscle training on facial growth in long-face children. Eur J Orthod. 1987; 9:15–23.

2. Proffit WR, Fields HW, Nixon WL. Occlusal forces in normal-and long-face adults. J Dent Res. 1983; 62:566–570.
3. Moss ML, Rankow RM. The role of the functional matrix in mandibular growth. Angle Orthod. 1968; 38:95–103.
4. Moss ML, Simon MR. Growth of the human mandibular angular process: a functional cranial analysis. Am J Phys Anthropol. 1968; 28:127–138.

5. Moss ML, Salentijn L. The primary role of functional matrices in facial growth. Am J Orthod. 1969; 55:566–577.

7. Uchida Y, Motoyoshi M, Shigeeda T, Shinohara A, Igarashi Y, Sakaguchi M, et al. Relationship between masseter muscle size and maxillary morphology. Eur J Orthod. 2011; 33:654–659.

8. Kubota M, Nakano H, Sanjo I, Satoh K, Sanjo T, Kamegai T, et al. Maxillofacial morphology and masseter muscle thickness in adults. Eur J Orthod. 1998; 20:535–542.

9. Park W, Kim BC, Yu HS, Yi CK, Lee SH. Architectural characteristics of the normal and deformity mandible revealed by three-dimensional functional unit analysis. Clin Oral Investig. 2010; 14:691–698.

10. Raadsheer MC, Van Eijden TM, Van Spronsen PH, Van Ginkel FC, Kiliaridis S, Prahl-Andersen B. A comparison of human masseter muscle thickness measured by ultrasonography and magnetic resonance imaging. Arch Oral Biol. 1994; 39:1079–1084.

11. Ariji Y, Kimura Y, Gotoh M, Sakuma S, Zhao YP, Ariji E. Blood flow in and around the masseter muscle: normal and pathologic features demonstrated by color Doppler sonography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:472–482.

12. Ariji Y, Sakuma S, Izumi M, Sasaki J, Kurita K, Ogi N, et al. Ultrasonographic features of the masseter muscle in female patients with temporomandibular disorder associated with myofascial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:337–341.

13. Takagi Y, Kimura Y, Nakamura H, Sasaki M, Eguchi K, Nakamura T. Salivary gland ultrasonography: can it be an alternative to sialography as an imaging modality for Sjogren's syndrome? Ann Rheum Dis. 2010; 69:1321–1324.

14. Yonetsu K, Ikemura K. Ultrasonographic study of the relation of metastatic nodes to the carotid artery. Head Neck Surg. 1987; 9:279–283.

15. Kiliaridis S, Kalebo P. Masseter muscle thickness measured by ultrasonography and its relation to facial morphology. J Dent Res. 1991; 70:1262–1265.

16. Kiliaridis S, Mahboubi PH, Raadsheer MC, Katsaros C. Ultrasonographic thickness of the masseter muscle in growing individuals with unilateral crossbite. Angle Orthod. 2007; 77:607–611.

17. Satiroğlu F, Arun T, Işik F. Comparative data on facial morphology and muscle thickness using ultrasonography. Eur J Orthod. 2005; 27:562–567.
18. Tircoveluri S, Singh JR, Rayapudi N, Karra A, Begum M, Challa P. Correlation of masseter muscle thickness and intermolar width - an ultrasonography study. J Int Oral Health. 2013; 5:28–34.
19. Turpin DL. Growth and remodeling of the mandible in the Macaca mulatta monkey. Am J Orthod. 1968; 54:251–271.

20. Cicchetti DV, Nelson LD. Re-examining threats to the reliability and validity of putative brain-behavior relationships: new guidelines for assessing the effect of patients lost to follow-up. J Clin Exp Neuropsychol. 1994; 16:339–343.

21. Bakke M, Tuxen A, Vilmann P, Jensen BR, Vilmann A, Toft M. Ultrasound image of human masseter muscle related to bite force, electromyography, facial morphology, and occlusal factors. Scand J Dent Res. 1992; 100:164–171.

22. Cotti E, Campisi G, Garau V, Puddu G. A new technique for the study of periapical bone lesions: ultrasound real time imaging. Int Endod J. 2002; 35:148–152.

23. Caivano D, Bufalari A, Giorgi ME, Conti MB, Marchesi MC, Angeli G, et al. Imaging diagnosis–transesophageal ultrasound-guided removal of a migrating grass awn foreign body in a dog. Vet Radiol Ultrasound. 2014; 55:561–564.

24. Bruneton JN, Balu-Maestro C, Marcy PY, Melia P, Mourou MY. Very high frequency (13 MHz) ultrasonographic examination of the normal neck: detection of normal lymph nodes and thyroid nodules. J Ultrasound Med. 1994; 13:87–90.

25. Yasumoto M, Nakagawa T, Shibuya H, Suzuki S, Satoh T. Ultrasonography of the sublingual space. J Ultrasound Med. 1993; 12:723–729.

26. Ng TK, Vasilareas D, Mitterdorfer AJ, Maher PO, Lalak A. Prostate cancer detection with digital rectal examination, prostate-specific antigen, transrectal ultrasonography and biopsy in clinical urological practice. BJU Int. 2005; 95:545–548.





 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download