Abstract
Background and Purpose
The various tests that are routinely used to diagnose generalized myasthenia gravis, such as the edrophonium test, serum anti-acetylcholine-receptor antibodies (AChR-Ab), and repetitive nerve stimulation (RNS) tests, have lower diagnostic sensitivity in ocular myasthenia gravis (OMG). Diagnosing OMG becomes even more difficult when the clinical symptoms are subtle. There is no gold-standard diagnostic test available for OMG patients, and so this study compared the diagnostic sensitivity of gaze photographs with conventional tests in OMG.
Methods
Records of gaze photographs were available for 25 of 31 consecutive patients diagnosed with OMG. Each patient underwent a neuro-ophthalmologic examination, serum AChR-Ab, RNS, edrophonium test, ice tests, and the acquisition of gaze photographs. The margin reflex distance 1 (MRD1) was measured on each of the gaze photographs, with MRD1 <2 mm or an interlid MRD1 difference of ≥2 mm on any of the gaze photographs defined as a positive sign of OMG. The diagnostic sensitivities of the tests were assessed.
Myasthenia gravis (MG) is an autoimmune disorder characterized by weakness and fatigability of voluntary muscles due to defects in neuromuscular transmission.12 Ocular myasthenia gravis (OMG) is a subset of MG in which the clinical manifestations are restricted to the ocular muscles. Diagnosing OMG presents neurologists and ophthalmologists with a complex problem.1345 Even in the current era of evidence-based medicine, diagnosing OMG often relies heavily on the typical clinical history of fluctuating diplopia and/or ptosis, with symptoms worsened by exertion.6 Diagnosing OMG becomes much more difficult when the clinical symptoms are subtle. Moreover, there is no gold-standard diagnostic test available for this subgroup of patients.7
Anti-acetylcholine-receptor antibodies (AChR-Ab) are present in approximately 85% of patients with generalized MG, but they are found in only about 55% of OMG patients.3 Furthermore, the response to the repetitive nerve stimulation (RNS) test is decreased in at least 75% of generalized MG patients but in fewer than 50% of OMG patients.2 Although single-fiber electromyography (SFEMG) has high diagnostic sensitivity (83–92%), it is limited by major drawbacks such as low specificity, the requirement for specially trained and experienced examiners, and long test sessions that are wearisome for both patients and electrodiagnosticians.23456 All of these factors limit the general implementation of the test.124 The edrophonium test is known to be highly sensitive to OMG, but is characterized by a relatively high false-positive rate and potentially serious cardiac complications.47 Clinical tests such as the ice test and the rest test can be easily performed without patient morbidity, but their diagnostic value might be limited with variable results.8
Gaze photographs, which are primarily used to document ocular motility dysfunction, are simultaneously capable of demonstrating abnormalities in the lid position. These photographs are taken while the patient is asked to sustain gaze in a specified direction for several seconds. We considered the possibility of using gaze photographs to demonstrate the presence of variable degrees of ptosis, and subsequently to use this information as an ancillary diagnostic test for OMG. There are no previously published reports on the use of gaze photographs for diagnosing OMG. In this study we measured the margin reflex distance 1 (MRD1)—which is the distance between the center of the pupillary light reflex and the upper eyelid margin—for each gaze photograph.
The goal of this study was to determine the diagnostic efficacy of gaze photographs in patients with OMG.
We retrospectively reviewed the medical records of patients diagnosed with OMG whose weakness had been limited to extraocular, levator palpebrae superioris, and orbicularis oculi muscles from August 2003 to October 2007 at Seoul National University Bundang Hospital. The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-0807/059-103). Six of 31 consecutive OMG patients were excluded from the study since no records of gaze photographs were available for them. OMG was diagnosed using the following criteria: 1) typical clinical history of ptosis and/or diplopia with variability, fatigability in muscle function, exacerbation of muscle weakness after repetitive or sustained effort, and improvement after rest, 2) positive findings on the edrophonium, RNS, or AChR-Ab test, and 3) improvement of clinical symptoms after a therapeutic trial with pyridostigmine even if the edrophonium, RNS, and AChR-Ab tests all have negative findings.19
Collected data included presenting symptoms, type of strabismus and duction limitation present at the initial examination, and type of treatment received by the patient. The diagnostic sensitivities of the RNS, AChR-Ab, ice tests, and the gaze photographs were assessed and compared. The RNS test was recorded over the orbicularis oculi, flexor carpi ulnaris, and abductor digiti quinti muscles following previously described methods.10 The threshold for an abnormal decrease in response varied according to the rate of electrical stimulation: 8% for the orbicularis oculi, 8–11% for the flexor carpi ulnaris, and 5–7% for the abductor digiti quinti muscles.10 AChR-Ab were tested using a standard radioimmunoassay of serum samples, with values ≥0.2 nmol/L considered positive. The ice test was performed by placing a frozen 50-mL sterile normal saline pack on the more-ptotic eyelid for 5 minutes. Complete or almost complete resolution of ptosis, or in increase in the palpebral fissure width of at least 2 mm was considered a positive result.
Gaze photographs were taken with the patient's head in a standardized stationary position, with his/her chin and forehead rested on a fixation support (Fig. 1 with permission of the examinee). The patient was asked to fixate for about 5 seconds on nine predesignated locations, during which photographs of eye movements as well as lid position were taken. Two additional photographs were also taken with each eye occluded. We measured MRD1 on each of the gaze photographs using image analysis software (ImageJ, National Institutes of Health, Bethesda, MD, USA) assuming that the horizontal corneal diameter was 12 mm. MRD1 is measured in millimeters: it is positive if the upper eyelid margin is above the light reflex at the center of the pupil, and it is negative if the upper eyelid is ptotic and the upper eyelid margin covers the center of the pupil and also the light reflex.11 MRD1 <2 mm (the average MRD1 in Koreans is reportedly 2.6 mm)12 or an interlid MRD1 difference of ≥2 mm on any of the gaze photographs was considered a positive sign of OMG. In order to assess the false-positive rate of the gaze photographs with this criterion for diagnosing OMG, MRD1 was also analyzed in 25 age-matched nonmyasthenic controls.
Thirteen (52%) of the 25 included patients were men. The mean age at onset was 38.5 years (range, 2–76 years), and the mean follow-up period was 12.1 months (range, 1–29 months). At the initial visit, 10 patients (40%) presented with diplopia only, 9 (36%) presented with diplopia combined with ptosis, and 6 (24%) presented with ptosis only.
At the initial examination, strabismus was present in 21 patients (84%), and ocular motility limitation was present in 22 (88%) (Table 1 and 2). The initial therapy comprised pyridostigmine alone in 19 patients (76%), combined pyridostigmine and prednisone in 1 patient (4%), and prednisone alone in 1 patient (4%). Four patients (16%) were observed clinically without applying any specific treatment.
The RNS test was positive in 14 of 25 patients (56%), the AChR-Ab test was positive in 16 of 25 patients (64%), and the ice test was positive in 8 of 11 patients (73%). The gaze photographs were positive in 20 of 25 patients (80%) (Table 3). Analysis of gaze photographs in nonmyasthenic control patients produced a false-positive rate of 40%. When lateral gaze photographs were excluded, and only forward and upward gazes were included, the false-positive rate dropped to 28% and the specificity was calculated to be 72%.
Four patients had negative results on both the AChR-Ab and RNS tests. Three of these patients were admitted for further workup and were finally diagnosed with OMG on the basis of positive results on the edrophonium test. One of these three patients is described in detail in the next section. All four patients were positive for OMG on gaze photography.
A 26-year-old woman visited the neuro-ophthalmology clinic with horizontal diplopia and intermittent ptosis of the left eyelid. The patient reported that her symptoms worsened at nighttime and with physical fatigue. An ophthalmologic examination revealed a small degree of exotropia on alternative cover testing with distance fixation. MRD1 during attempted primary gaze was +3 mm in the right eye and +0.5 mm in the left eye. The ptosis was aggravated with monocular occlusion, with MRD1 values of +2.5 mm and −0.5 mm in the right and left eyes, respectively. The left-side ptosis was aggravated with sustained primary and leftward gaze. The RNS and AChR-Ab tests were performed under the impression of OMG, but both tests produced normal results. On gaze photographs, ptosis of the left eyelid was present on primary gaze, leftward gaze, rightward gaze, and with right-eye occlusion (Fig. 2).
The patient was admitted for further workup. The ptosis of the left eye showed marked improvement during the edrophonium test. SFEMG also demonstrated delayed neuromuscular transmission that was compatible with MG. Based on the positive findings on SFEMG and the edrophonium test, the patient was diagnosed with OMG and was treated with pyridostigmine.
All of the OMG patients in this study presented with eyerelated chief complaints, with diplopia alone present in 40% of patients, diplopia combined with ptosis in 36%, and ptosis alone in 24%. The RNS test, AChR-Ab test, and gaze photographs were performed in all patients, and the ice test was performed in 11 patients. The diagnostic sensitivities of the RNS test, AChR-Ab test, gaze photographs, and ice test were 56%, 64%, 80%, and 73%, respectively. The false-positive rate, which reflects the specificity of a given test, was 40% when MRD1 analysis was performed in nonmyasthenic controls, and 28% when lateral gaze photographs were excluded.
While 60% of the patients initially presented with ptosis, careful analysis of gaze photographs enabled ptosis to be detected in patients who were initially assumed to only be presenting with diplopia (7 out of 10 diplopia-only patients were positive for OMG on gaze photographs). This discrepancy in findings between the chief complaints of the patient and results from analyzing gaze photographs is most likely to be due to the absence of subjective discomfort arising from the mild nature of the ptosis.
Four patients (16%) had negative results on both RNS and AChR-Ab tests. Three of these patients required admission and were diagnosed with OMG after the edrophonium test proved positive. The remaining patient underwent a therapeutic trial with pyridostigmine and was diagnosed with OMG based on the improvement of clinical symptoms. All four patients were positive for OMG on gaze photography. These findings illustrate the clinical relevance and high diagnostic sensitivity of gaze photography.
The implementation of a relatively simple and sensitive outpatient-based clinical test with low patient morbidity would help to prevent misdiagnoses of seronegative or RNS-negative OMG patients. Although the edrophonium test and SFEMG may enhance the diagnostic sensitivity, these are complex and time-consuming tests that are associated with patient morbidity.24 Gaze photographs can be used to demonstrate levator palpebrae muscle fatigability and any accompanying strabismus or ocular motility limitation. However, more importantly, these conditions can induce lid fatigability even when ocular symptoms are not evident on primary gaze. MRD1 may be calculated in gaze photographs to provide a more accurate analysis of eyelid position. Gaze photographs can also be used to simultaneously document such ocular abnormalities while the test is being performed. The test can therefore be used as a past reference and as a follow-up guide for monitoring how patients respond to treatment.
MRD is the distance between the corneal light reflex and the eyelid position. MRD is an important parameter for objectively quantifying eyelid position and is essential for evaluating several diseases including ptosis, MG, and thyroid ophthalmopathy, as well as documentation for insurance reimbursement and surgical planning. Many studies have demonstrated the high reliability of MRD when assessing eyelid measurements in a clinical setting.1314 In addition to clinical measurements, photographic documentation using digital photography has become commonplace.15 Digital images have been shown to be comparable to traditional methods of measurement, in terms of repeatability and reproducibility.161718 In addition, we used a digital single-lens-reflex camera (Canon EOS60D with EF 100 mm lens, Canon Corporation, Tokyo, Japan) with a lens-mounted ring flash unit (Macro Ring Lite MR-14EX II, Canon Corporation), which is known to correspond well with clinical MRD measurements, and all gaze photographs were taken with the patient's head in a standardized stationary position with his/her chin and forehead resting on a fixation support.19
In contrast to the edrophonium test or SFEMG, gaze photographs are not only simple to perform and free of patient morbidity, they also do not require highly trained personnel or a long testing time. The ability to objectively analyze variability in eyelid position using simple computer software does away with the need for an additional process of reader standardization. In this study, the false-positive rate in the normal controls was 40% when gaze photographs were used and 28% when lateral gaze photographs were excluded. Reasons for false positives were asymmetric blepharochalasis resulting in differences in eyelid margin due to droopy upper eyelid skin, and so the diagnostic efficacy when using gaze photographs could be reduced in elderly patients with blepharochalasis. However, the false-positive rate improved to 28% when we excluded the lateral gaze photographs. Applying stricter criteria such as excluding lateral gaze photographs would improve diagnoses in elderly patients. It would also be necessary to rule out pseudoptosis, whose differential diagnoses include blepharophimosis, blepharochalasis, or a vertical deviation such as hypotropia.
The limitations of this study are the small number of cases and the retrospective nature of data collection, which inherently restricts data analyses. Prospective studies involving larger numbers of patients are warranted to further investigate the diagnostic value of gaze photographs in OMG. Also, the MRD1 criteria suggested in this study are rudimentary, and so future studies should attempt to find the optimal MRD1 for acceptable specificity and sensitivity values when utilizing gaze photographs to diagnose OMG.
Despite these limitations, our study is the first to use gaze photographs in diagnosing OMG. A variable degree of ptosis is a known clinical hallmark of OMG, and yet there are no diagnostic tools to objectively measure or record this important clinical finding. We believe that gaze photographs are an indispensable diagnostic tool that can overcome this diagnostic shortcoming.
In conclusion, our study has demonstrated that the diagnostic sensitivity when using gaze photographs is comparable to those of conventional tests for OMG. We believe that using gaze photographs in conjunction with established diagnostic tests for OMG will enhance the diagnostic accuracy and aid neurologists and ophthalmologists in solving the often enigmatic puzzle of OMG.
Figures and Tables
Fig. 1
A fixation support for use when taking gaze photographs. The patient's head could be fixed in a standardized stationary position with the chin and forehead resting on the support.

Fig. 2
Gaze photographs of a patient who showed negative results in anti-acetylcholine-receptor antibody and repetitive nerve stimulation tests, but showed a variable degree of ptosis of the left eye.

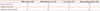
Table 1
Types of strabismus at presentation in patients with ocular myasthenia gravis

Table 2
Types of ocular motility limitation at presentation in patients with ocular myasthenia gravis

Acknowledgements
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. 2017R1A2 B4011450).
References
1. Weinberg DA, Lesser RL, Vollmer TL. Ocular myasthenia: a protean disorder. Surv Ophthalmol. 1994; 39:169–210.

2. Kusner LL, Puwanant A, Kaminski HJ. Ocular myasthenia: diagnosis, treatment, and pathogenesis. Neurologist. 2006; 12:231–239.
3. Palace J, Vincent A, Beeson D. Myasthenia gravis: diagnostic and management dilemmas. Curr Opin Neurol. 2001; 14:583–589.

4. Luchanok U, Kaminski HJ. Ocular myasthenia: diagnostic and treatment recommendations and the evidence base. Curr Opin Neurol. 2008; 21:8–15.

5. Benatar M. A systematic review of diagnostic studies in myasthenia gravis. Neuromuscul Disord. 2006; 16:459–467.

6. Padua L, Stalberg E, LoMonaco M, Evoli A, Batocchi A, Tonali P. SFEMG in ocular myasthenia gravis diagnosis. Clin Neurophysiol. 2000; 111:1203–1207.

8. Park JY, Yang HK, Hwang JM. Diagnostic value of repeated ice tests in the evaluation of ptosis in myasthenia gravis. PLoS One. 2017; 12:e0177078.

9. Kim JH, Hwang JM, Hwang YS, Kim KJ, Chae J. Childhood ocular myasthenia gravis. Ophthalmology. 2003; 110:1458–1462.

10. Oh SJ. Electromyography: Neuromuscular Transmission Studies. Baltimore: Williams & Wilkins;1988. p. 1–304.
11. Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthalmic Plast Reconstr Surg. 2012; 28:308–311.

12. Jun AK, Ahn CS. [MA statistical evaluation of the average value of margin reflex distance I and margin limbal distance in Koreans]. J Korean Ophthalmol Soc. 1990; 31:1243–1248.
13. Boboridis K, Assi A, Indar A, Bunce C, Tyers AG. Repeatability and reproducibility of upper eyelid measurements. Br J Ophthalmol. 2001; 85:99–101.

14. Small RG, Sabates NR, Burrows D. The measurement and definition of ptosis. Ophthalmic Plast Reconstr Surg. 1989; 5:171–175.

15. Parmar DN, Rose GE. Fundamentals of oculoplastic surgery. In : Chen WP, editor. Oculoplastic Surgery: the Essentials. 1st ed. New York: Thieme;2001. p. 512.
16. Cruz AA, Lucchezi MC. Quantification of palpebral fissure shape in severe congenital blepharoptosis. Ophthalmic Plast Reconstr Surg. 1999; 15:232–235.

17. Cruz AA, Coelho RP, Baccega A, Lucchezi MC, Souza AD, Ruiz EE. Digital image processing measurement of the upper eyelid contour in Graves disease and congenital blepharoptosis. Ophthalmology. 1998; 105:913–918.

18. Flowers RS, Flowers SS. Diagnosing photographic distortion. decoding true postoperative contour after eyelid surgery. Clin Plast Surg. 1993; 20:387–392.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download