Abstract
Purpose
Autosomal dominant polycystic kidney disease (ADPKD) is the most common hereditary kidney disease, and 20% of patients eventually require nephrectomies due to compressive symptoms or renal-related complications. Traditionally, nephrectomies were performed via the open approach in view of space constraints. We evaluate our institution's outcomes for laparoscopic nephrectomy (LN) for ADPKD.
Materials and Methods
We retrospectively reviewed 33 patients with ADPKD who underwent nephrectomies from November 2005 to December 2016 at a tertiary institution. Preoperative kidney volume was calculated via the ellipsoid method by using computed tomography scan.
Results
The median age was 51.0 years (interquartile range [IQR], 44.5–56.0 years). Sixteen patients (48.5%) underwent open nephrectomy (ON), 15 patients (45.5%) had LNs, and 2 patients (6.1%) had laparoscopic converted to ON due to dense adhesions. Thirteen patients had bilateral while 18 patients had unilateral nephrectomies. Median kidney volume in the open group was 1,042 cm3 (IQR, 753–2,365 cm3) versus 899 cm3 (IQR, 482–1,914 cm3) in the laparoscopy group and did not differ significantly. The operative time was comparable between both groups. Patients who underwent LN had lesser blood loss (350 mL vs. 650 mL; 95% confidence interval [CI], 1.822–3.533; p=0.016) and shorter length of hospital stay (4.0 days vs. 6.5 days; 95% CI, 1.445–5.755; p=0.001) compared to patients who underwent ON. Both groups had similar low morbidity rate and no mortality.
Autosomal dominant polycystic kidney disease (ADPKD) is a progressive, systemic disorder characterised by multiple bilateral cysts of the renal parenchyma. It is the most common hereditary kidney disease with a global prevalence between 1:400 to 1:1,000 [1]. The progressive development of cysts will replace renal parenchyma and cause worsening renal function, with more than half of patients eventually developing end stage renal failure (ESRF) requiring renal replacement therapy [23]. Globally, ADPKD accounts for approximately 10% of ESRF [4] whilst it accounts for 2% of ESRF cases in our country [5].
The affected kidneys frequently grow to a large size, causing compressive symptoms, such as abdominal distension or pain, back pain, nausea, and early satiety. Complications include recurrent gross hematuria from hemorrhagic cyst, recurrent urinary tract infections from infected cyst, nephrolithiasis, hypertension, and predisposition to malignancy. ADPKD increases the risk of renal cell carcinoma in ESRF patients by 2 to 3 times compared to the general ESRF population without ADPKD [6]. About 20% of patients will eventually have their kidneys removed [7] due to aforementioned complications. Additionally, nephrectomy of the native polycystic kidneys which extend into the true pelvis are often performed to create space in anticipation of subsequent kidney transplantation.
Open nephrectomy (ON) for huge kidneys requires an elaborate midline laparotomy incision. The sheer size of the polycystic kidneys and the adhesions which arise from previous cysts ruptures and infections present significant technical challenges. This can give rise to significant morbidity for the patient. Multiple studies have described the successful removal of polycystic kidneys through a minimally invasive approach with some demonstrating simultaneous bilateral laparoscopic nephrectomies (LNs). Known benefits of LN include shorter hospital stay, decreased morbidity, and quicker recovery. However, unlike LN in a normal sized kidney, LN in ADPKD is challenging due to the sheer size of the kidneys and the consequent lack of space for dissection even with pneumoperitoneum. A larger incision for specimen extraction of huge polycystic kidney may increase the risk of incision-related complications and negate the benefits of traditional LN with a smaller incision. Guo et al. [8] conducted a systematic review through meta-analysis of observational comparative studies that compared ON versus LN in ADPKD up to October 2014. The study concluded that LN might have a longer operative time, shorter length of hospital stay (LOS), lower complication rate, less estimated blood loss (EBL), and lower blood transfusion rate but no significant difference in analgesic requirement compared to the open approach.
The aim of our study is to review Singapore General Hospital experience in managing patients with ADPKD who required nephrectomies. We aimed to compare the perioperative outcomes between these 2 nephrectomy approaches to determine if the results are similar to that in current literature.
We performed an Institutional Review Board approved retrospective analysis of all 35 consecutive ADPKD patients who underwent nephrectomy from November 2005 to December 2016 at Singapore General Hospital (approval number: 2017/2327). Thirty-three patients were included in our study after exclusion of 2 patients due to incomplete data. Eighteen patients (54.5%) underwent open of which 2 patients (6.1%) were laparoscopic converted to ON versus 15 patients (45.5%) who had LN.
Indications f or nephrectomy, baseline clinical characteristics and preoperative parameters were analyzed between ON and LN. Indications for nephrectomy were hemorrhagic cyst, infected cyst, or suspected malignancy. Baseline clinical characteristics included age, gender, body mass index (BMI), and baseline Eastern Cooperative Oncology Group performance (ECOG) status (Table 1).
The preoperative kidney volume, an objective size criterion readily available in a clinical setting, was determined from preoperative computed tomography (CT) abdomen and pelvis scan with contrast. Each CT scan sequence included coronal and axial images, whereby length was measured from the coronal view (cm), and lateral and anteriorposterior diameters (cm) were measured from the axial view. The ellipsoid method, kidney volume=length×lateral diameter×anterior-posterior diameter×(π/6) [910], was employed to derive an estimated kidney volume using the measurements obtained. Two independent study members measured the length, lateral and anterior-posterior diameters of both left and right kidneys of each CT scan. After ascertaining that inter-observer variability was negligible, the measured kidney volumes from the 2 observers were averaged to obtain the left and right kidney volumes.
Perioperative outcomes measured included duration of nephrectomy, blood loss, and intraoperative blood transfusion rate. The LOS and postoperative complications, graded using the Clavien-Dindo system, were compared between the open and laparoscopic approaches. Altogether, 5 surgeons participated in this retrospective study. All of them had been accredited and had performed at least 30 cases of open and LNs previously. We believed there were negligible differences in their surgical experiences.
Statistical analyses were carried out using IBM SPSS ver. 20 (IBM Co., Armonk, NY, USA). Categorical and continuous variables were analyzed via chi-square test and Mann-Whitney U-test respectively. Multivariate analyses were performed using binary logistic and linear regression model to adjust for any confounding effects. Hazard ratio was used for categorical analyses while B, mean differences, was used for multivariate analyses. The type of nephrectomy (open vs. laparoscopic), the number of nephrectomy (unilateral vs. bilateral), and kidney volume were compared in multivariate analyses as they had been previously determined to affect perioperative outcomes based on our literature review.
Thirty-five consecutive patients with ADPKD underwent nephrectomy of which 33 had complete records for analysis. There were 20 males (60.6%) and 13 females (39.4%), with a median age of 51.0 years (interquartile range [IQR], 44.5–56.0 years). Twenty-seven patients (81.8%) were ECOG 0 whilst 6 patients (18.2%) were ECOG 1 at baseline. All patients were ESRF prior to surgery except for 1 patient (3.0%) with stage 3 chronic kidney disease. Median BMI was 24.7 kg/m2 (IQR, 21.0–26.6 kg/m2). Indications for nephrectomy included: hemorrhagic cyst in 21 patients (63.7%), suspected malignancy in 8 patients (24.2%), and infected renal cyst in 4 patients (12.1%). Sixteen patients (48.5%) underwent open, 15 patients (45.5%) laparoscopic, and 2 patients (6.0%) had laparoscopic converted to open due to dense adhesions between the right kidney and duodenum. Thirteen patients (39.4%) had bilateral nephrectomy performed in the same setting. There was no significant difference in the choice of nephrectomies (ON vs. LN) when stratified into 2 separate time periods, suggesting that the surgeons in our study were proficient in both techniques.
All preoperative variables were compared between the ON and LN groups (Table 2). There were no differences between patient demographics (age, gender, BMI, comorbidities), blood results (hemoglobin, Hb), number of nephrectomies (unilateral and bilateral), or kidney volumes. The median kidney volume for ON was 1,042.0 cm3 (IQR, 753.0–2,365.0 cm3) compared to 899.0 cm3 for LN (IQR, 482.5–1,914.0 cm3).
There was no difference in the operating time between the two approaches (Table 3). The median operating time for ON was 172.5 minutes (IQR, 122.8–249.8 minutes), which was invariably similar to LN, with median time of 180.0 minutes (IQR, 153.0–287.0 minutes). The difference remained insignificant on multivariate analyses. On the other hand, there was a significant difference for blood loss between the two approaches (Table 4). The median blood loss for ON was 650.0 mL (IQR, 300.0–1,225.0 mL), which was much greater than LN, 350.0 mL (IQR, 200.0–450.0 mL). This difference remained significant after adjusting for the numbers of nephrectomies and kidney volume (B: −326.5, confidence interval [CI], −579.7 to −77.4; p=0.013). Six patients (33.3%) who underwent ON required intra-op transfusions. This was much greater than the 1 patient (6.7%) in the LN group that required transfusions, with a statistical significance reached on multivariate analysis (odds ratio, 3.8; 95% CI, 1.1 to 7.0; p=0.043) (Table 5).
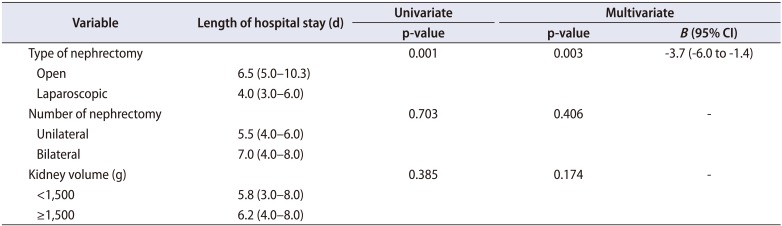
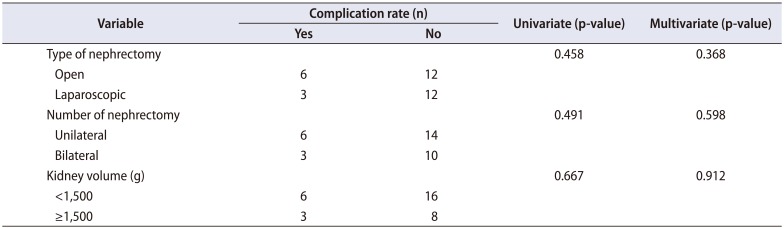
There was no 30-day mortality between both approaches. However, patients undergoing LN had a shorter LOS, median 4.0 days (IQR, 3.0–6.0 days), compared to patients who underwent an open approach, median 6.5 days (IQR, 5.0–10.3 days), and remained significant on multivariate analysis (B: −3.7; 95% CI, −6.0 to −1.4; p=0.003) (Table 6). Six patients (33.3%) undergoing ONs had complications. Three patients had persistently low Hb levels that required further postoperative blood transfusions, 2 patients had hyperkalemia that required intravenous calcium gluconate and immediate dialysis and 1 patient had wound dehiscence that required a relook laparotomy. Three patients (20.0%) in the LN group had complications, of which 2 patients had low Hb that required postoperative blood transfusions and 1 patient suffered from aspiration pneumonitis. There was no statistical difference between the complication rates in both surgical techniques (Table 7). In terms of final pathological diagnosis, all except one patient had benign disease consistent with ADPKD. The remaining patient who underwent ON had a left sided renal cell carcinoma, pT1bN0M0, Fuhrman grade 2.
Patients who underwent bilateral nephrectomies have a higher intraoperative blood loss compared to unilateral nephrectomy (890.0 mL vs. 400.0 mL). This remained significant after adjusting for the type of nephrectomy and kidney volume (B: −454.3; 95% CI, −716.4 to −192.0; p=0.001) (Table 4). Other perioperative outcomes, such as operating times, postoperative complications, and LOS remained similar between both groups.
Altogether there were 22 patients with preoperative kidney volume <1,500 g and 11 patients with kidney volume ≥1,500 g. There was no difference in the type of nephrectomies (laparoscopic vs. open) or the perioperative outcomes (operating time, blood loss, intraoperatiove transfusion, LOS, and postoperative complications).
In this retrospective review of our institution's experience in managing patients with ADPKD, we have demonstrated that LN is a feasible alternative to ON. Patients who underwent LN had similar operative times, less intraoperative blood loss and blood transfusions, and shorter hospital stay. Postoperative complication rates were similar in both groups with no 30-day mortality.
The laparoscopic approach is the current standard of care for most kidney conditions requiring nephrectomy. The advantages and safety of LN over the open approach are now well established and has been shown to have better perioperative outcomes such as intraoperative blood loss, LOS, blood transfusion rate, analgesic usage, and cosmesis [1111213141516].
However, in patients with ADPKD, the large kidney size poses much technical challenges due to space constraints in the abdomen, difficulty in approaching the renal hilum and an occasional intense perinephric inflammatory reaction making dissection of tissue planes more challenging [16]. While conventional ONs were previously performed for these patients, there is an increasing trend towards laparoscopy with current literature reporting it to be safe and feasible [1718].
Elashry et al. [11] first reported a small series of 4 LNs for ADPKD, in particularly emphasizing on one case that involved laparoscopic removal of a 2,200 g specimen, demonstrating that size may not be a contraindication to laparoscopic surgery. However, operating times were significantly longer (mean, 257.5 minutes). Gill et al. [12] subsequently demonstrated the use of balloon dilatation in the upper and lower retroperitoneum external to Gerota's fascia in order to create a larger operating field, expanding the largest specimen weight in their series to 2,600 g.
Till date, Guo et al. [8] published the most comprehensive summary of the comparison between ON and LN via a meta-analysis, reviewing 6 published articles that contained 7 studies, and compared 118 cases of LN and 77 cases of ON. In his analyses, he concluded a few key findings: Firstly, LN had a significantly longer operative time than ON. Secondly, LN had a lower EBL and transfusion requirements. Thirdly, reporting specimen weight significantly showed that LN might not extract specimens as heavy as ON, suggesting that ON might be safer for larger kidneys. Fourthly, patients who underwent LN had a significantly short LOS. Lastly, there was no difference in complication rate or analgesia usage between the two groups.
However, there were many limitations that would have affected the validity of the conclusions. The meta-analysis consisted of 7 studies with limited sample size, ranging from 6 to 34 patients who underwent LNs for ADPKD. Furthermore, the study represented a very heterogeneous group of patients with significant differences in demographics. While the operating time for LNs seem longer, this should be taken into account that the meta-analysis consists of studies over a span of 13 years, during which laparoscopy surgery has advanced rapidly and most surgeons today are significantly more skilled in LNs than a decade ago. Instead, there was no difference in operating times between ON and LN in our study. This could be contributed by the fact that nephrectomies for ADPKD remained a technically more challenging procedure than routine nephrectomies, and in Singapore General Hospital, such nephrectomies were carried out by a small group of urologists with significant surgical expertise.
On the other hand, there was no stratification between the number of nephrectomies (unilateral vs. bilateral) in the laparoscopy and open groups. Instinctively, if there were more bilateral nephrectomies in the laparoscopic group, perioperative outcomes such as blood loss, operating times, and LOS may have been significantly confounded. We attempted to address this stratification and showed that there is no significant difference in the number of nephrectomies between the laparoscopic and open surgery groups (Table 2). Multivariate analyses were performed to eliminate the confounding role of the number of nephrectomies in perioperative outcomes (Tables 3,4,5,6,7).
Lastly, in one of the studies, Eng et al. [19] also commented that there is a significantly learning curve for LN in ADPKD and less experienced surgeons would have taken a much longer time for such operations. In our study, however, we had demonstrated that there was no difference in operating time between the two techniques. This could be attributed to the increased familiarity with LN performed by a few urologists sub-specialized in minimally invasive kidney surgery in our center, as previously described in our methodology.
In the meta-analysis, Guo et al. [8] also commented that the extract specimen size was relatively smaller in LNs compared to ONs, suggesting that ONs may be more feasible in larger specimens. However, in one of the studies, Desai et al. [14] reported that in LNs, renal cysts are often deliberately ruptured to allow the delivery of the specimens via smaller incisions. Such deliberate cystic decompressions would have contributed to the significant difference in specimen size between a LN and ON.
A more objective comparison would be a preoperative volumetric assessment of the kidney sizes instead of postoperative specimen weighing, as the effects of surgical decompression would be negated. In our study, preoperative CT scans were reviewed and the renal volumes were calculated via the ellipsoid method by 2 separate independent observers, with negligible inter-observer variability. As such, there was no significant difference between the kidney volumes in the LN and ON groups. Similarly, our surgeons also practised deliberate cystic decompressions as necessary to facilitate extraction of specimens. Although technically, such maneuvers may increase the risk of peritonitic-like symptoms or prolonged ileus [20] that could be the result of cyst puncture [21] and infectious cyst fluid, none of these complications were seen in Guo's meta-analysis or our study.
Separately, other studies have discussed the feasibility of LN in larger kidney specimens. Lipke et al. [16] commented a higher rate of conversion to open surgeries for kidney size >3,500 cm3. He concluded that increased operative time, increased blood loss, and transfusion rate in these conversions to open, may have been decreased if patients with larger kidneys had undergone open bilateral nephrectomies from the outset. Unfortunately, Lipke's study was limited by the small sample size of 14 patients, and there was an alarmingly high complication rate of 50%, which may be attributed by the surgical technical aspects rather than solely due to the specimen size. Another retrospective study by Ivey et al. [17] reviewed reasons for conversion to open surgery in 44 out of total 399 LNs performed in a single center over a 9-year period. The study reported that ADPKD was associated with the highest rate of open conversion (13%) and specifically, a higher open conversion rate of 40% versus 8.2% (p<0.001) was associated with kidney specimens weighing >1,500 g compared to <1,500 g.
In our study, there was no significant difference in kidney volumes between LNs and ONs, after stratifying according to ≥1,500 g and <1,500 g. There was no kidney specimen larger than 3,500 g for stratification. This reflected that size itself is not a primary consideration for the nature of operation (LN vs. ON). In particular, of the 2 patients who had laparoscopic converted to ONs, only one patient had kidney size >1,500 g. More importantly, there was no difference in the perioperative outcomes as shown in Tables 3,4,5,6,7. We believed that while the space constraints and difficulties in approaching the hilum in a larger kidney size posed greater surgical challenges, the potential benefits of LN could be replicated in the hands of experienced surgeons.
On the other hand, our study concurred with Guo's observation that LN achieved a lower intraoperative blood loss compared to ON. A likely reason for this is due to the creation of the pneumoperitoneum in laparoscopic surgery, conferring a tamponade effect which decreases blood loss and therefore the need for intraoperative blood transfusion. In addition, the improved visualization in laparoscopic surgery allows for more meticulous surgical dissection as well as hemostasis translating to less blood loss and transfusion. Although more patients who underwent ON required blood transfusions, these results did not reach statistically significance, but was significant in Guo's meta-analysis. Blood transfusion is of particular importance to potential renal transplant recipients, as the transfusion might expose the patient to new antigens and hence form antibodies that can affect the recipient's compatibility with a graft kidney in future [22].
Lastly, our study had demonstrated the benefits of shorter LOS in LN could be replicated specifically in ADPKD. This is exceptional paramount for patients with ADPKD, who are mostly end-stage renal failure, making them immunocompromised and more susceptible to nosocomial infections than the general public undergoing nephrectomies for other indications. Furthermore, most of these ADPKD patients are candidates for subsequent renal transplants and may have already been started on some form of immunosuppressant to reduce rejection.
Our study is limited by its retrospective nature. It is a relatively small series possibly affected by the low prevalence of the ADPKD in our country compared to the prevalence of approximately 15 million people worldwide and 500,000 people in the United States, being responsible for 5% to 10% of all ESRF [24]. However, our study size remained comparative to the studies documented in Guo's meta-analysis.
LN for ADPKD patients in our Asian population is a safe and feasible alternative to ON with reduced blood loss and LOS, and comparable perioperative outcomes in terms of operative time and complication rates. While larger kidney size may pose a greater challenge, the benefits of LNs can replicated in the hands of experienced surgeons.
References
1. Gabow PA. Autosomal dominant polycystic kidney disease. N Engl J Med. 1993; 329:332–342. PMID: 8321262.

2. Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007; 369:1287–1301. PMID: 17434405.

3. Grantham JJ. Clinical practice. Autosomal dominant polycystic kidney disease. N Engl J Med. 2008; 359:1477–1485. PMID: 18832246.
4. 2014 USRDS Annual Data Report. Chapter 1: Incidence, prevalence, patient characteristics, and treatment modalities. Am J Kidney Dis. 2015; 66(Suppl 1):93–110.
5. Woo KT. The Singapore Renal Registry: an overview. Singapore Med J. 1993; 34:157–163. PMID: 8266160.
6. Hajj P, Ferlicot S, Massoud W, Awad A, Hammoudi Y, Charpentier B, et al. Prevalence of renal cell carcinoma in patients with autosomal dominant polycystic kidney disease and chronic renal failure. Urology. 2009; 74:631–634. PMID: 19616833.

7. Patel P, Horsfield C, Compton F, Taylor J, Koffman G, Olsburgh J. Native nephrectomy in transplant patients with autosomal dominant polycystic kidney disease. Ann R Coll Surg Engl. 2011; 93:391–395. PMID: 21943464.

8. Guo P, Xu W, Li H, Ren T, Ni S, Ren M. Laparoscopic nephrectomy versus open nephrectomy for patients with autosomal dominant polycystic kidney disease: a systematic review and meta-analysis. PLoS One. 2015; 10:e0129317. PMID: 26053633.

9. Lim KS, Tay S, Gostelow M, Fook-Chong SMC, Ng LG. Does size really matter? A retrospective analysis of donor renal volume and its effects on renal function in donors after donation. J Biomed Graphics Comput. 2016; 6:14–21.

10. Breau RH, Clark E, Bruner B, Cervini P, Atwell T, Knoll G, et al. A simple method to estimate renal volume from computed tomography. Can Urol Assoc J. 2013; 7:189–192. PMID: 23826046.

11. Elashry OM, Nakada SY, Wolf JS Jr, McDougall EM, Clayman RV. Laparoscopy for adult polycystic kidney disease: a promising alternative. Am J Kidney Dis. 1996; 27:224–233. PMID: 8659498.

12. Gill IS, Kaouk JH, Hobart MG, Sung GT, Schweizer DK, Braun WE. Laparoscopic bilateral synchronous nephrectomy for autosomal dominant polycystic kidney disease: the initial experience. J Urol. 2001; 165:1093–1098. PMID: 11257645.

13. Wisenbaugh ES, Tyson MD 2nd, Castle EP, Humphreys MR, Andrews PE. Massive renal size is not a contraindication to a laparoscopic approach for bilateral native nephrectomies in autosomal dominant polycystic kidney disease (ADPKD). BJU Int. 2015; 115:796–801. PMID: 24903738.

14. Desai MR, Nandkishore SK, Ganpule A, Thimmegowda M. Pretransplant laparoscopic nephrectomy in adult polycystic kidney disease: a single centre experience. BJU Int. 2008; 101:94–97. PMID: 17922857.

15. Bendavid Y, Moloo H, Klein L, Burpee S, Schlachta CM, Poulin EC, et al. Laparoscopic nephrectomy for autosomal dominant polycystic kidney disease. Surg Endosc. 2004; 18:751–754. PMID: 15026905.

16. Lipke MC, Bargman V, Milgrom M, Sundaram CP. Limitations of laparoscopy for bilateral nephrectomy for autosomal dominant polycystic kidney disease. J Urol. 2007; 177:627–631. PMID: 17222647.

17. Ivey BS, Lucas SM, Meyer CA, Emley TE, Bey A, Gardner TA, et al. Conversions in laparoscopic renal surgery: causes and outcomes. J Endourol. 2011; 25:1167–1173. PMID: 21671761.

18. Verhoest G, Delreux A, Mathieu R, Patard JJ, Vigneau C, Rioux-Leclercq N, et al. Transperitoneal laparoscopic nephrectomy for autosomal dominant polycystic kidney disease. JSLS. 2012; 16:437–442. PMID: 23318070.

19. Eng M, Jones CM, Cannon RM, Marvin MR. Hand-assisted laparoscopic nephrectomy for polycystic kidney disease. JSLS. 2013; 17:279–284. PMID: 23925022.

20. Park SK, Olweny EO, Best SL, Tracy CR, Mir SA, Cadeddu JA. Patient-reported body image and cosmesis outcomes following kidney surgery: comparison of laparoendoscopic single-site, laparoscopic, and open surgery. Eur Urol. 2011; 60:1097–1104. PMID: 21856076.

21. Yu HY, Hevelone ND, Lipsitz SR, Kowalczyk KJ, Hu JC. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol. 2012; 187:1392–1398. PMID: 22341274.

22. Binsaleh S, Luke PP, Nguan C, Kapoor A. Comparison of laparoscopic and open nephrectomy for adult polycystic kidney disease: operative challenges and technique. Can J Urol. 2006; 13:3340–3345. PMID: 17187698.
Table 1
Patient profile
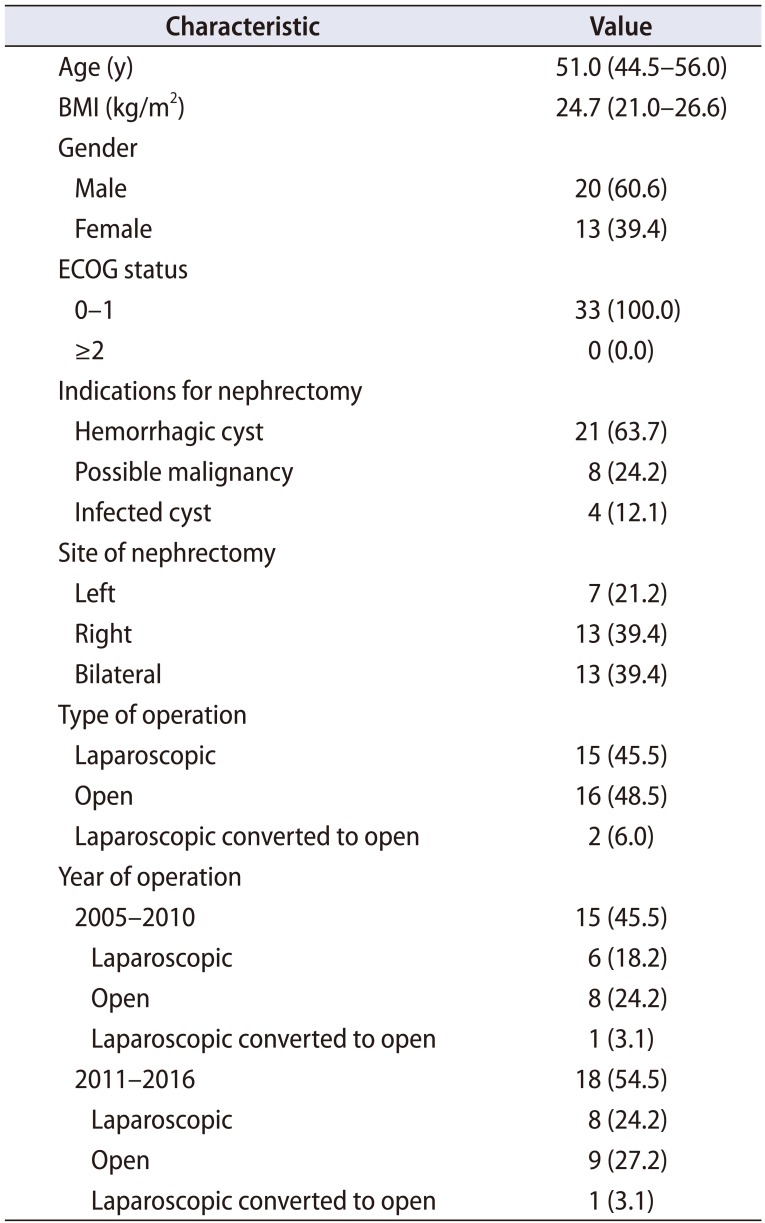
Table 2
Analysis between ON and LN
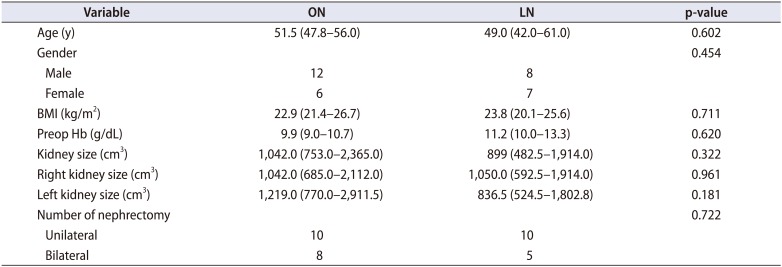
Table 3
Operating time
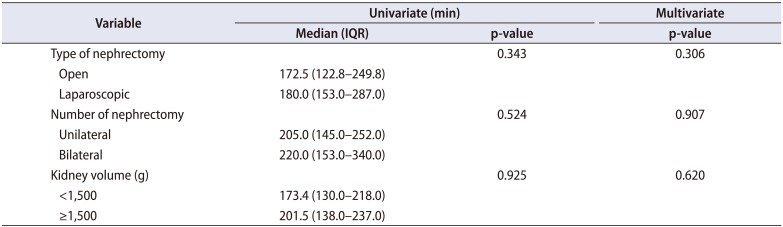
Table 4
Blood loss
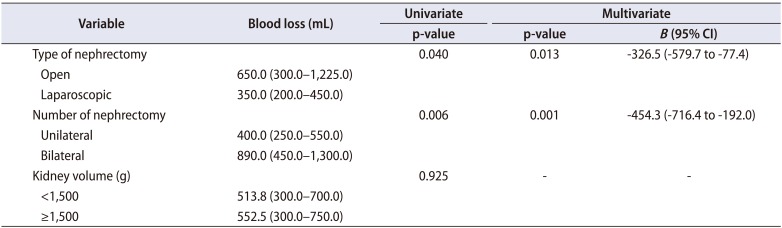
Table 5
Intraoperative blood transfusion
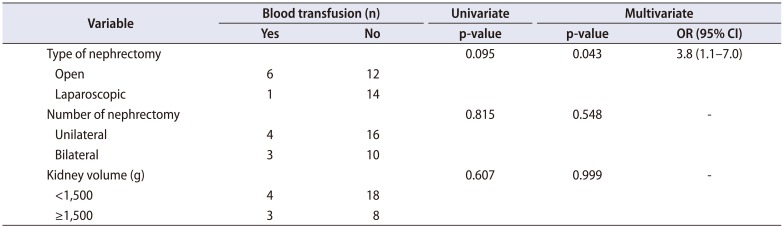
Table 6
Length of hospital stay




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download