Abstract
Intraoperative bovine-derived topical thrombin is still widely used for hemostasis during surgery. A 38-year-old woman with chronic spontaneous urticaria was referred to the orthopedic surgery department for herniated disk and myelopathy. During the first stage of operation, bovine-derived thrombin powder soaked in Gelfoam was used as a hemostatic aid. After 30 minutes, the patient developed anaphylactic shock with systemic skin rash and angioedema. Repeated intravenous bolus and infusion of vasopressor were carried out, and her blood pressure normalized. Skin test and specific immunoglobulin E test showed positive results for bovine thrombin and beef, respectively. During the second stage of operation (After 10 days from first stage of operation), bovine-derived thrombin powder was excluded and the operation was successful without any unexpected events. Therefore, bovine thrombin should be used with caution because it might cause anaphylaxis.
Topical thrombin is one of the major hemostatic aids, which is often used when surgical ligation or electrocautery of bleeding vessels is not effective. It has been used during surgery since the 1940s and exponentially after their effect on hemostasis during surgery was proved effective.12 Currently, it is used for more than 1 million patients per year in the United States.3 Despite its popular use, adverse reactions have rarely been reported.4 However, bovine thrombin formulations are linked to the development of antibodies against human coagulation proteins.56 Therefore, human thrombin formulations and recombinant protein thrombin formulations have been developed.7 However, bovine thrombin formulations are still widely used today because of the extremely low incidence of adverse event, and cost-effectiveness.
Herein, we describe a case of anaphylaxis after the use of intraoperative bovine-derived thrombin powder for hemostasis during anterior cervical discectomy and fusion.
A 38-year-old woman was referred to the orthopedic surgery department for herniated disk from C2 to C7 level. Her medical history showed brain artery aneurysm, hypertension (on losartan potassium and clopidogrel daily), and chronic spontaneous urticaria. Staged anterior and posterior cervical diskectomy and fusion were performed to relieve her symptoms.
During the first stage of anterior cervical diskectomy, intravenous ephedrine, rocuronium, glycopyrrolate, lidocaine, and propofol were administered for anesthesia induction and intubation. After 40 minutes from anesthesia induction, the operation was started. During operation, bleeding was controlled with the use of bovine-derived thrombin-soaked gelatin form. Thirty minutes after the first incision, her blood pressure suddenly dropped (from 102/58 to 35/28 mmHg) with a relatively slow pulse rate (from 68 to 61 bpm/min). She developed systemic rash and facial angioedema (Fig. 1). After several injections of epinephrine and continuous intravenous injection of norepinephrine and vasopressin, her blood pressure normalized. Intravenous methylprednisolone (125 mg) and pheniramine (4 mg) were administered to relieve the rash. The operation was restarted and lasted for 2 hours. At the end of the operation, extubation could not be performed due to tongue swelling and edematous airway. Subsequently, she was transferred to the intensive care unit. She fully recovered and was transferred to the ward after 1 day.
The laboratory results are as follows: white blood cell count, 17,090/mm3 (eosinophils 0.1%); hemoglobin, 14.4 g/dL, and platelet count, 193,000/µL. Specific immunoglobulin E (IgE) test showed positive to beef (1.10 kU/L) and pork (1.05 kU/L) and negative to galactose-α-1,3-galactose (α-gal) (0.09 kU/L) and gelatin (0.03 kU/L) (UniCAP, Phadia, Uppsala, Sweden). Component resolved diagnosis test showed positive to bovine serum albumin (Bos d 6) (3.47 kU/L) and porcine serum albumin (Sus s 1) (1.84 kU/L) (UniCAP, Phadia).
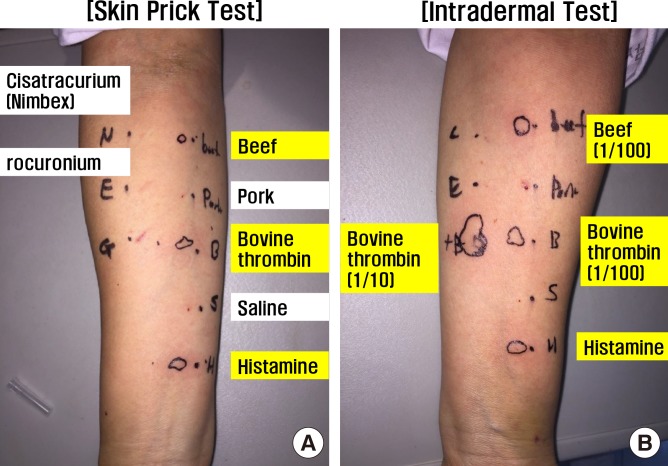
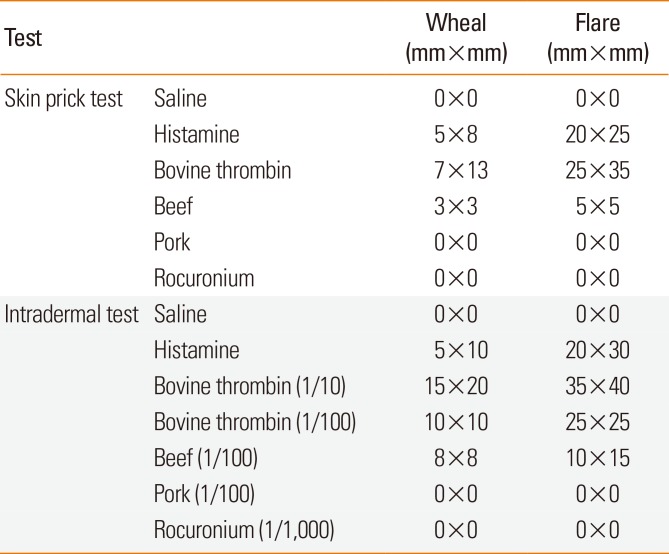
Sensitivity testing revealed a positive skin prick test to bovine thrombin (Reyon, Seoul, Korea) and beef (Allergopharma, Reinbek, Germany). Intradermal test also showed positive to bovine thrombin and beef. In addition, skin test results showed negative responses to pork (Allergopharma) and rocuronium (MSD, West Point, PA, USA) (Table, Fig. 2). In conclusion, she was allergic to beef and bovine-derived products.
After 10 days from first stage of operation, second stage of operation (posterior cervical discectomy at C2-7) was conducted. During operation, intraoperative bovine-derived thrombin was not used. The operation ended successfully without any unexpected event. She was discharged, and any adverse reaction was not observed during the 6-month follow-up period.
Thrombin has been widely used for hemostasis during surgery. Thrombin acts as a hemostatic aid.89 Its initial source was bovine in origin. Bovine thrombin-induced antibodies cause adverse drug reactions and even death. Then, human thrombin and recombinant thrombin have been developed. However, bovine thrombin formulations are still widely used until now because of the extremely low prevalence of adverse reactions and its cost-effectiveness.
Several patients suffered from anaphylaxis due to bovine thrombin. Tadokoro et al.10 showed that anaphylaxis is mediated by specific IgE to bovine thrombin antibody, and based on radioallergosorbent test inhibition analysis, the antigenic substances were bovine-specific moiety that is mainly involved in the contaminant rather than bovine thrombin itself. In this case, skin and specific IgE test results showed positivity to bovine thrombin, beef, and Bos d 6 which does not contain bovine thrombin itself.11 This means that bovine thrombin allergy was mediated by a specific IgE antibody, and allergic component was not thrombin itself. In addition, this case showed negative to α-gal which is usually used to diagnose red meat allergy syndrome; then we can exclude it. She suffered chronic urticaria; and it is aggravated when she eats beef. Then, she stopped eating beef. Overall, we concluded she has a true beef allergy (but not red meat allergy nor thrombin itself allergy).
Skin test showed negative result to pork; whereas serum specific IgE to pork and Sus s 1 was positive. Discrepancy in results from skin test and specific IgE has been well known.12 Although there are lots of debate, skin prick test is considered to be slightly more reliable than specific IgE in food allergy.1314 We can consider she is an asymptomatic sensitizer to pork. However, we should keep in mind that she can be allergic to pork someday.
In this case, the patient had difficulty recovering from anaphylactic shock; 2 causes were associated with this condition. First, she usually took losartan (angiotensin II receptor blocker) for hypertension. Angiotensin inhibitor causes an increased risk of anaphylaxis because the renin-angiotensin system is a compensatory mechanism response that decreases peripheral vascular resistance, which causes shock that is induced by anaphylaxis.15 Second, bovine-derived thrombin-soaked gelatin form was not removed during surgery, because, it was not suspected as a culprit of anaphylaxis at that time. It remained in her neck tissues even after end of operation. Burn out of allergic reactions related to the mediators might have caused a full recovery (called desensitization) in short period of time.16 The dissolution of bovine thrombin products in her neck tissues according to half-life may have led to long-term recovery.
Intraoperative bovine-derived topical thrombin is still widely used for hemostasis during surgery. This case report suggests that bovine thrombin should be used with caution because it can cause anaphylaxis.
References
1. Bae KC, Cho CH, Lee KJ, Son ES, Lee SW, Lee SJ, et al. Efficacy of intra-articular injection of thrombin-based hemostatic agent in the control of bleeding after primary total knee arthroplasty. Knee Surg Relat Res. 2014; 26:236–240. PMID: 25505706.

2. Suzuki R, Matsuhashi M, Kuwahara T, Kase T. Topical use of thrombin in prostatic surgery. Hinyokika Kiyo. 1986; 32:1461–1464. PMID: 2436462.
3. Lawson JH. The clinical use and immunologic impact of thrombin in surgery. Semin Thromb Hemost. 2006; 32(Suppl 1):98–110.

4. Clark JA, Humphries JE, Crean S, Reynolds MW. Topical bovine thrombin: a 21-year review of topical bovine thrombin spontaneous case safety reports submitted to FDA's Adverse Event Reporting System. Pharmacoepidemiol Drug Saf. 2010; 19:107–114. PMID: 20014051.

5. Ortel TL, Mercer MC, Thames EH, Moore KD, Lawson JH. Immunologic impact and clinical outcomes after surgical exposure to bovine thrombin. Ann Surg. 2001; 233:88–96. PMID: 11141230.

6. Streiff MB, Ness PM. Acquired FV inhibitors: a needless iatrogenic complication of bovine thrombin exposure. Transfusion. 2002; 42:18–26. PMID: 11896308.

7. Chapman WC, Singla N, Genyk Y, McNeil JW, Renkens KL Jr, Reynolds TC, et al. A phase 3, randomized, double-blind comparative study of the efficacy and safety of topical recombinant human thrombin and bovine thrombin in surgical hemostasis. J Am Coll Surg. 2007; 205:256–265. PMID: 17660072.

8. Ham SW, Lew WK, Weaver FA. Thrombin use in surgery: an evidence-based review of its clinical use. J Blood Med. 2010; 1:135–142. PMID: 22282693.
9. Tanaka KA, Key NS, Levy JH. Blood coagulation: hemostasis and thrombin regulation. Anesth Analg. 2009; 108:1433–1446. PMID: 19372317.

10. Tadokoro K, Ohtoshi T, Takafuji S, Nakajima K, Suzuki S, Yamamoto K, et al. Topical thrombin-induced IgE-mediated anaphylaxis: RAST analysis and skin test studies. J Allergy Clin Immunol. 1991; 88:620–629. PMID: 1918728.

11. Sim DW, Lee JS, Park KH, Jeong KY, Ye YM, Lee JH, et al. Accurate assessment of alpha-gal syndrome using cetuximab and bovine thyroglobulin-specific IgE. Mol Nutr Food Res. 2017; 61:1601046.

12. Liang KL, Su MC, Jiang RS. Comparison of the skin test and ImmunoCAP system in the evaluation of mold allergy. J Chin Med Assoc. 2006; 69:3–6. PMID: 16447919.

13. Yanagida N, Sato S, Takahashi K, Nagakura KI, Ogura K, Asaumi T, et al. Skin prick test is more useful than specific IgE for diagnosis of buckwheat allergy: a retrospective cross-sectional study. Allergol Int. Forthcoming 2017.

14. Nacaroglu HT, Erdem SB, Karaman S, Dogan D, U Karkiner CS, Kanık ET, et al. Diagnostic values for egg white specific IgE levels with the skin prick test in Turkish children with egg white allergy. Allergol Immunopathol (Madr). 2017; 45:445–451. PMID: 28237131.

15. Coop CA, Schapira RS, Freeman TM. Are ACE inhibitors and beta-blockers dangerous in patients at risk for anaphylaxis? J Allergy Clin Immunol Pract. 2017; 5:1207–1211. PMID: 28552379.

Fig. 2
Skin prick test (A) and intradermal test (B). The black line of circle reveals the outline of wheal.
Table
Results of skin test




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download