Abstract
Objective
The aim of this study was to assess the analgesic effect of a single application of low-level laser therapy (LLLT) on spontaneous pain and pain on chewing after placement of initial archwires.
Methods
Forty-two patients (26 women, 16 men) were randomly recruited for this split-mouth randomized clinical trial. Each patient received super-elastic nickel-titanium (NiTi) initial archwires (0.012, 0.014, 0.016, and 0.018-inch [in]) in the maxilla for leveling and alignment for an interval of 4 weeks between archwires. One side of the mouth was randomly designated as experimental, while the other side served as placebo. After insertion of each archwire, the experimental side was irradiated with a diode laser for 3 seconds each on 5 points facially and palatally per tooth, from the central incisor to first molar. On the placebo side, the laser device was held the same way but without laser application. A numerical rating scale was used to assess the intensity of spontaneous and masticatory pain for the following 7 days. The Mann-Whitney U test was used to compare pain scores between sides.
Results
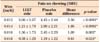
Patients in the LLLT group exhibited significantly lower mean scores for spontaneous pain after insertion of the initial two archwires (0.012-in and 0.014-in NiTi; p < 0.05), while there was no significant difference for 0.016-in and 0.018-in wires between the LLLT and placebo groups. LLLT significantly reduced chewing pain scores (p < 0.05) for all archwires.
Pain is a subjective feeling of distress caused by stimulation of specialized nerve endings.1 Patients undergoing orthodontic treatment usually experience pain of varying degrees during treatment,2 which leads to decreased acceptance of treatment and noncompliance.3 After the activation of an appliance, pain usually begins within 4 hours, increases over the following 24 hours, and diminishes within 7 days.4 Pain is a major factor dampening patients' determination for pursuing orthodontic treatment5 and some even consider ceasing the treatment prematurely due to the pain they experience.6 For this reason, orthodontists have been searching for effective methods to reduce patient discomfort that are not associated with undesirable effects over the course of treatment and on patient health.
One common method of pain reduction is the use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid7 and ibuprofen,8 among others. However, the use of NSAIDs during tooth movement may result in aberrant remodeling of the periodontal vasculature, causing impairment in tooth movement, eventually affecting orthodontic treatment efficacy.9101112 Other methods of pain management include anesthetic gels,13 xylitol chewing gums,13 bite wafers,14 transcutaneous electrical nerve stimulation,1516 and vibratory stimulation of the periodontal ligament17; however, these methods have yielded inconsistent results.
Recently, the application of low-level laser therapy (LLLT) to periodontal tissues has been introduced as a method of pain reduction.318192021 The effect of LLLT in terms of reducing pain is two-fold: the first is the inhibition of the release of arachidonic acid, which leads to decreased levels of prostaglandin E22223; the second is the release of beta-endorphin, an endogenous opioid neuropeptide that produces potent analgesic effects.12 Because the energy output of the laser device is very low, it does not increase the temperature of the irradiated tissue above normal,20 which makes LLLT a noninvasive, nonthermal procedure.1819
A review of the literature highlights the role of LLLT in minimizing postoperative pain after insertion of elastomeric separators.1924 Although multiple applications of LLLT have been used in previous studies to reduce orthodontic pain,19 very few investigations have evaluated the analgesic effect of LLLT on pain in relation to the initial stage of alignment of the teeth.20 Therefore, the aim of this study was to assess the analgesic effects of a single application of LLLT on postoperative spontaneous and masticatory pain associated with the placement of initial archwires in orthodontic patients during alignment of teeth.
The present study was a single-blinded, placebo-controlled randomized clinical trial using a split-mouth design. The study was conducted at the Department of Orthodontics at Baqai Medical University and Liaquat College of Medicine and Dentistry. The study was approved by the Ethics Committee of both centers. Forty-two patients (26 women, 16 men; 12 to 25 years of age) of Pakistani ethnic background were selected for this study. Informed consents were obtained from all participants. The sample comprised 24 adolescents (≤ 18 years of age) and 18 adults (> 18 years of age). The sample size was calculated using G power version 3.1.9 software. The power of the study was set at 0.80 with a 95% confidence interval, and the effect size was set at 0.8. Hence, the total sample size intended for this research was 42 subjects. Although the inclusion criteria involved patients with Class I, II, and III molar relationships, symmetric malocclusion was the essential criterion for eligibility. Patients who required extractions for initial alignment and leveling were excluded from the sample. Because this was a split-mouth clinical trial, special consideration was given to the extent of crowding between both sides. Patients with differences > 1 mm in crowding between sides were also excluded. Other exclusion criteria included patients taking periodic prescription drugs, parafunctional habits, temporomandibular joint dysfunction, impacted teeth (except third molars), or periodontally compromised patients. Participants who used analgesics during the trial were also excluded from the study.
The operator explained the procedure to all participants and informed consent was obtained. For participants under 18 years of age, consent forms were signed by their legal guardians. The orthodontic treatment was commenced by bonding the maxillary arch with preadjusted edgewise 0.022-inch [in] slot MBT prescription brackets (Ortho Organizers, Carlsbad, CA, USA). Alignment and leveling was achieved using 0.012-in super-elastic nickel-titanium (NiTi) wire followed by 0.014, 0.016, and 0.018-in NiTi wires, changed at 4-week intervals between each wire.
In each patient, the left and right sides were randomly designated as experimental and placebo by coin flip.25 Laser therapy was applied on the experimental side after placement of each archwire. The laser unit was a 940-nm aluminum-gallium-arsenide (Al-Ga-As) diode laser (iLase; Biolase, Irvine, CA, USA) set on continuous mode with power at 100 mW. The procedure was performed according to standard protocol (i.e., in a segregated room using protective eyewear for the operator, assistant, and patient). The fiber tip of the laser was held perpendicular to the mucosa overlying the roots of teeth, in close but light contact with the surface of the gingival tissues. The mucosa was irradiated for 3 seconds each on 5 points facially and palatally per tooth, starting from central incisor to the first molar. These points were mesial and distal over the cervical-third of the root and middle of the root, and mesial and distal over the apical-third of the root. Because the diameter of the optical fiber tip was 0.04 cm2, the energy density was calculated to be 7.5 J/cm2 for each point and total energy density was 75 J per tooth. While applying laser to the experimental side, a plastic shield was used as a barrier to protect the placebo side from the laser beam. The shield was fashioned by modifying a pair of safety goggles provided with the laser unit because of its wavelength specificity. On the placebo side, the laser device was held the same way for the same time without turning the laser unit on. Music was played at a high volume in the room so that the patient could not hear the beeping sound emitted by the device while in use.
A questionnaire was designed to measure pain intensity using a numerical rating scale (NRS). It included feedback for spontaneous pain and pain on mastication. After the application of laser, these questionnaires were given to the participants to be completed at home and returned at the following appointment. The participants were asked to record pain at consecutive 12 hours intervals for 7 days. In addition, telephone calls were made every day for 7 days to ensure accurate collection of data.
IBM SPSS Statistics version 20.0 (IBM Co., Armonk, NY, USA) was used to analyze the data. Descriptive analysis was performed to obtain the mean values of pain in both groups. The Mann-Whitney U test was used to compare the level of pain between experimental and placebo sides independently for spontaneous pain during day, night, and pain on chewing. The same test was also applied to compare pain reported by male and female patients. Pain experienced by adolescents (≤ 18 years of age) and adults (> 18 years of age) was also compared using the Mann-Whitney U test.
The duration of this study was 7 months (July 2014 to January 2015). Forty-two patients (mean age, 19.81 years) were recruited, all of whom met the inclusion criteria.
In this study, most of the patients reported an increase in pain intensity 12 hours after the insertion of each archwire. The intensity of pain persisted for 2 days and began to dissipate thereafter. Though LLLT reduced pain perception on chewing, it was still greater than spontaneous pain in that group. The maximum intensity of pain reported in this study was during mastication on the placebo side subsequent to the insertion of the 0.012-in NiTi archwire (Figure 1).
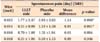
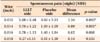
Pain perception in the patients was analyzed independently for each archwire. Pain intensity was more severe during alignment with the initial archwire than the latter wires (Tables 1, 2, 3 and Figures 1, 2, 3, 4). Most of the patients with 0.016-in and 0.018-in NiTi archwires did not experience considerable spontaneous pain, although some still reported pain on mastication (Table 3).
There was a statistically significant difference between LLLT and placebo groups in pain perceived by the patients during day, night, and on chewing for all NiTi archwires except 0.016-inand 0.018-in, which demonstrated no significant difference in spontaneous pain during day and night. However, the difference in pain on chewing remained statistically significant, as shown in Table 3.
The difference in pain was neither significant between males and females, nor between adolescents and adults (p < 0.05). Intragroup comparison revealed no significant difference in pain during day, night, or on chewing in the LLLT group (p = 0.8); however, it was significant in the placebo group (p = 0.02).
Pain is a subjective response and is expressed with wide individual variation. It depends on many factors such as age, sex, individual pain threshold, magnitude of force applied, emotional state, dental anxiety level, motivation for orthodontic treatment, and previous pain experience.2627 A split-mouth design was used in the present study because it eliminates inter-individual variability from estimations of the treatment effect. Despite several benefits, an inherent shortcoming of this design was the likelihood of carry-across effects from one side to the other.28 A plastic shield was positioned over the placebo side while applying laser to the experimental side so that any laser beams that may have been reflected did not penetrate the placebo side and, perchance, alter the results. Another prerequisite for a split-mouth design is that the disease to be investigated should be uniformly distributed.29 For this reason, patients with symmetrical malocclusions were included in this study. None of the patients reported any sense of temperature variation while the laser therapy was applied because of the very lower power output and energy dose delivered by the unit. This also kept the study design intact.
A diode (Al-Ga-As) laser, with wavelength at the beginning of the near-infrared electromagnetic spectrum, was used. Infrared radiation has a low absorption coefficient in hemoglobin and water; thus, more depth of penetration in the irradiated tissue.1 It has been established previously that infrared radiation can achieve deeper penetration of irradiated tissues than laser therapy in the visible spectrum, possibly reaching cortical and alveolar bone tissues.13031 Laser was applied to 5 precise points over the root of each tooth facially and palatally, as described by Tortamano et al.20
The frequency of laser treatment was only once (i.e., single dose) after ligation of the archwires, unlike other studies that applied laser multiple times.1921 The laser unit beeps every second when in function; therefore, to keep patients blinded to the experimental and placebo sides, loud music was played in the room while the laser therapy was performed so that the patients were not able to appreciate the audible sound emitted by the laser unit. Moreover, none of the patients reported any discomfort or heating during treatment, which can be explained by the lower densities of light energy used in the therapy.32
An 11-point NRS was used, with 0 signifying no pain and 10 representing the other pain extreme (i.e., worst pain imaginable). In contrast, many previously published studies192124 have used a visual analogue scale. However, the NRS proved to be an effective assessment tool and has been shown to be highly correlated with the visual analog scale.33 Additionally, an NRS has the benefit of being administered verbally34; therefore, collecting data over the telephone was possible.
In this study, the most intense pain was associated with chewing. This is consistent with the results of previous studies,35 which concluded that chewing pain is sufficiently high to impede mastication and even swallowing performance. Both spontaneous and chewing pain peaked on the first 2 days after insertion of most of the archwires in both groups and began to dissipate thereafter. It has been established that postoperative pain reaches its maximum for 2 to 3 days, after which it gradually diminishes by day 5 or 6.535
Because orthodontic pain increases proportionally with the amount of force exerted, it is believed to have a linear relationship with contact point displacement.36 This could explain why there was intense pain during alignment with the initial archwires but reduced with 0.016-in and became negligible with 018-in NiTi wires. However, previous investigations did not find a linear relationship between pain and contact displacement.537 Another rationale for lower pain scores reported in the later stages of alignment could be the fact that patients become acclimated to the fixed appliance and pain, although this phenomenon is yet to be supported by research in the literature.
There was a significant difference between LLLT and placebo groups in the levels of spontaneous pain (p < 0.05) except in the 0.016-in and 0.018-in NiTi archwire groups, in which patients did not report any perceptible pain. Although this finding was consistent with that of the study by Tortamano et al.,20 that investigation used individualized stainless steel wires for alignment. It has been recognized that NiTi wires are ideal for initial alignment, and are most commonly used for the first phase of fixed appliance therapy.38 Domínguez and Velásquez35 also supported the analgesic effect of LLLT on pain following activation of orthodontic appliances; however, they evaluated this effect in the final stage of orthodontic treatment (i.e., after insertion of 0.019 × 0.025-in stainless steel wire).
Our results demonstrate that all LLLT groups exhibited significantly lower mean scores for masticatory pain after the insertion of archwires. The data substantiate the precedent studies320 and show that pain on the LLLT side had reduced intensity, and had shorter duration when compared with the placebo side of the mouth.
The aim of our study was to determine the analgesic effect of LLLT on postoperative pain during the initial alignment and leveling stage of orthodontic treatment. Further studies are required to validate the results of this study on larger sample size and the effects of LLLT on overall quality of life should be assessed.
Figures and Tables
Figure 1
Comparison between low-level laser therapy (LLLT) and placebo groups during day (A), night (B), and on chewing (C) for 0.012-in nickel-titanium archwire.
NRS, Numerical rating scale.

Figure 2
Comparison between low-level laser therapy (LLLT) and placebo groups during day (A), night (B), and on chewing (C) for 0.014-in nickel-titanium archwire.
NRS, Numerical rating scale.

Figure 3
Comparison between low-level laser therapy (LLLT) and placebo groups during day (A), night (B), and on chewing (C) for 0.016-in nickel-titanium archwire.
NRS, Numerical rating scale.

Figure 4
Comparison between low-level laser therapy (LLLT) and placebo groups during day (A), night (B), and on chewing (C) for 0.018-in nickel-titanium archwire.
NRS, Numerical rating scale.

Table 1
Comparison of spontaneous pain during daytime between low-level laser therapy (LLLT) and placebo groups (n = 42)
References
1. Krishnan V. Orthodontic pain: from causes to management--a review. Eur J Orthod. 2007; 29:170–179.

2. Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop. 1998; 114:684–691.

3. Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006; 130:371–377.

4. Koritsánszky N, Madléna M. Pain and discomfort in orthodontic treatments. Literature review. Fogorv Sz. 2011; 104:117–121.
5. Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop. 1992; 102:373–381.

6. Krukemeyer AM, Arruda AO, Inglehart MR. Pain and orthodontic treatment. Angle Orthod. 2009; 79:1175–1181.

7. Polat O, Karaman AI. Pain control during fixed orthodontic appliance therapy. Angle Orthod. 2005; 75:214–219.
8. Ngan P, Wilson S, Shanfeld J, Amini H. The effect of ibuprofen on the level of discomfort inpatients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1994; 106:88–95.

9. Kyrkanides S, O'Banion MK, Subtelny JD. Nonsteroidal anti-inflammatory drugs in orthodontic tooth movement: metalloproteinase activity and collagen synthesis by endothelial cells. Am J Orthod Dentofacial Orthop. 2000; 118:203–209.

10. Tyrovola JB, Spyropoulos MN. Effects of drugs and systemic factors on orthodontic treatment. Quintessence Int. 2001; 32:365–371.
11. Walker JB, Buring SM. NSAID impairment of orthodontic tooth movement. Ann Pharmacother. 2001; 35:113–115.

12. Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006; 130:364–370.

13. Shenoy N, Shetty S, Ahmed J, Shenoy KA. The pain management in orthodontics. J Clin Diagn Res. 2013; 7:1258–1260.

14. Hwang JY, Tee CH, Huang AT, Taft L. Effectiveness of thera-bite wafers in reducing pain. J Clin Orthod. 1994; 28:291–292.
15. Roth PM, Thrash WJ. Effect of transcutaneous electrical nerve stimulation for controlling pain associated with orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 1986; 90:132–138.

16. Weiss DD, Carver DM. Transcutaneous electrical neural stimulation for pain control. J Clin Orthod. 1994; 28:670–671.
17. Marie SS, Powers M, Sheridan JJ. Vibratory stimulation as a method of reducing pain after orthodontic appliance adjustment. J Clin Orthod. 2003; 37:205–208. quiz 203-4.
18. Cruz DR, Kohara EK, Ribeiro MS, Wetter NU. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med. 2004; 35:117–120.

19. Lim HM, Lew KK, Tay DK. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop. 1995; 108:614–622.

20. Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009; 136:662–667.

21. Kim WT, Bayome M, Park JB, Park JH, Baek SH, Kook YA. Effect of frequent laser irradiation on orthodontic pain. A single-blind randomized clinical trial. Angle Orthod. 2013; 83:611–616.
22. Angelieri F, Sousa MVS, Kanashiro LK, Siqueira DF, Maltagliati LÁ. Effects of low intensity laser on pain sensitivity during orthodontic movement. Dental Press J Orthod. 2011; 16:95–102.
23. Mizutani K, Musya Y, Wakae K, Kobayashi T, Tobe M, Taira K, et al. A clinical study on serum prostaglandin E2 with low-level laser therapy. Photomed Laser Surg. 2004; 22:537–539.

24. Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Badiee MR, Fekrazad R. The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci. 2014; 29:559–564.

25. Schulz KF, Chalmers I, Grimes DA, Altman DG. Assessing the quality of randomization from reports of controlled trials published in obstetrics and gynecology journals. JAMA. 1994; 272:125–128.

26. Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989; 96:47–53.

27. Kavaliauskiene A, Smailiene D, Buskiene I, Keriene D. Pain and discomfort perception among patients undergoing orthodontic treatment: results from one month follow-up study. Stomatologija. 2012; 14:118–125.
28. Pandis N, Walsh T, Polychronopoulou A, Katsaros C, Eliades T. Split-mouth designs in orthodontics: an overview with applications to orthodontic clinical trials. Eur J Orthod. 2013; 35:783–789.

29. Antczak-Bouckoms AA, Tulloch JF, Berkey CS. Split-mouth and cross-over designs in dental research. J Clin Periodontol. 1990; 17:446–453.

30. Nóbrega C, da Silva EM, de Macedo CR. Low-level laser therapy for treatment of pain associated with orthodontic elastomeric separator placement: a placebo-controlled randomized double-blind clinical trial. Photomed Laser Surg. 2013; 31:10–16.

31. Katoh H. Effect of far-infrared rays radiation on pain reaction associated with orthodontic tooth movement. J Jpn Orthod Soc. 1997; 56:17–25.
32. Jawad MM, Husein A, Alam MK, Hassan R, Shaari R. Overview of non-invasive factors (low level laser and low intensity pulsed ultrasound) accelerating tooth movement during orthodontic treatment. Lasers Med Sci. 2014; 29:367–372.

33. Holdgate A, Asha S, Craig J, Thompson J. Comparison of a verbal numeric rating scale with the visual analogue scale for the measurement of acute pain. Emerg Med (Fremantle). 2003; 15:441–446.

34. Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986; 27:117–126.

35. Domínguez A, Velásquez SA. Effect of low-level laser therapy on pain following activation of orthodontic final archwires: a randomized controlled clinical trial. Photomed Laser Surg. 2013; 31:36–40.

36. Furstman L, Bernick S. Clinical considerations of the periodontium. Am J Orthod. 1972; 61:138–155.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download