Dear Editor:
Sebaceous glands are skin appendages that provide lipid complex, the sebum, to the surface of skin. The sebocytes are the major cells comprising sebaceous glands, contributing to the production of sebum. At puberty, sebum production is increased by the multiple factors including androgens, corticotropin-releasing hormone, vitamin D and insulin-like growth factor-1 (IGF-1)1. The increase of sebum production often relates with the inflammatory skin diseases, of which most prevalent is acne. The excess sebum production is the primary event, followed by hyperkeratinization of pilosebaceous duct, hyperproliferation of commensal Propionibacterium acnes, and perifollicular inflammation23. For treatment of acne, many drugs have been developed targeting multiple action points. Examples include antibiotics targeting commensal bacteria (tetracycline, doxycycline and minocycline), drugs targeting hyperkeratinization (adapalene, isotretinoin and tazarotene), and anti-inflammatory drugs (corticosteroids and nonsteroidal anti-inflammatory drugs)4. Since sebum hypersecretion is believed to be the starting event for acne, there is still high clinical need for new and better treatments targeting the sebum production in sebocytes.
In a preliminary study, we screened anti-lipogenic materials using cultured human sebocytes. We first evaluated the effect of various medicinal plants, and found that the extract of Ginkgo biloba L. leaves had strong inhibitory potential on IGF-1-induced sebum production in sebocytes. We further delineated the active ingredients and identified isoginkgetin as one powerful compound. In this study, we demonstrated that isoginkgetin inhibited IGF-1-induced sebum production, providing evidence that isoginkgetin can be developed for acne treatment.
Normal human scalp specimens were obtained under the written informed consent, and the present study was approved from the ethical committee of the Institutional Review Board of Chungnam National University School of Medicine. The sebaceous glands were dissected under the stereomicroscope. Isolated sebaceous glands were attached to the culture dish, and incubated in Sebomed® medium (Biochrom, Berlin, Germany) supplemented with 10% fetal bovine serum and 5 ng/ml recombinant human epidermal growth factor (Life Technologies Corporation, Grand Island, NY, USA). Generally, sebocytes were outgrown from explanted sebaceous gland tissues in 1 week. Sebocytes at 3rd~7th passage were used for all experiments. Isoginkgetin was purchased from Merck Millipore (Darmstadt, Germany), and dissolved in dimethyl sulfoxide (DMSO), then diluted with culture medium (final concentrations of DMSO is 0.1%).
Isoginkgetin is a biflavonoid in which two flavone groups are linked covalently (Fig. 1A). We first checked the cytotoxicity of isoginkgetin on sebocytes. As a result, isoginkgetin showed no cytotoxicity up to the concentration of 20 µM (Fig. 1B). We then determined the effect of isoginkgetin on sebum production using a well-established IGF-1-induced lipogenesis model35. Thin layer chromatography analysis showed that isoginkgetin dramatically inhibited IGF-1-induced squalene synthesis. In addition, production of wax ester was also remarkably inhibited by isoginkgetin (Fig. 1C). Since the squalene and wax ester are the unique components of sebum1, this result suggested that isoginkgetin specifically inhibited sebum production in sebocytes.
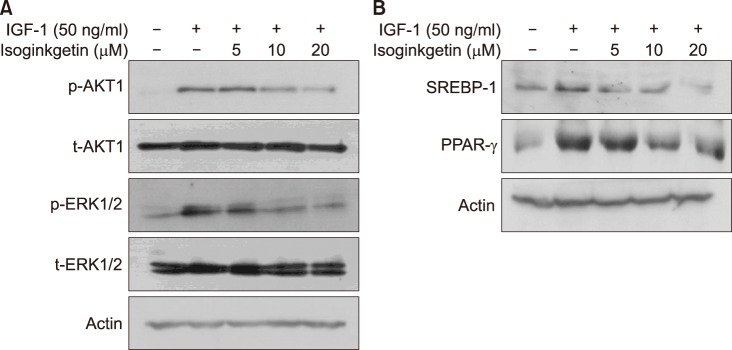
To investigate whether isoginkgetin influences intracellular signaling related to lipogenesis, we examined the phosphorylation of AKT1 and ERK1/2. When sebocytes were activated by IGF-1, the phosphorylation of AKT1 and ERK1/2 was remarkably increased. Pretreatment with isoginkgetin significantly inhibited the IGF-1-induced phosphorylation of AKT1 and ERK1/2 (Fig. 2A). Next, we examined whether isoginkgetin affected the expression of sterol response element-binding protein-1 (SREBP-1) and peroxisome proliferator-activated receptor-γ (PPAR-γ), the important transcription factors for lipid production in human sebocytes67. Consistent with previous reports, IGF-1 increased SREBP-1 and PPAR-γ. And, isoginkgetin significantly inhibited IGF-1-induced increase of SREBP-1 and PPAR-γ (Fig. 2B).
Isoginkgetin is one of biflavonoids found in Ginkgo biloba L. leaves, which possesses a variety of biological activities. For example, isoginkgetin shows the suppressive activity against lymphocyte proliferation induced by concanavalin A or lipopolysaccharides8. In other example, isoginkgetin is a general inhibitor for pre-mRNA splicing9. It has been also demonstrated that isoginkgetin inhibits tumor cell invasion by regulating PI3K/AKT1-dependent matrix metalloproteinase-9 expression10. In this study, we demonstrated that isoginkgetin inhibited IGF-1-induced sebum production in sebocytes. In addition, isoginkgetin significantly inhibited IGF-1 induced increase of SREBP-1 and PPAR-γ. Consistent with previous study in other system10, isoginkgetin significantly blocked the IGF-1-induced AKT1 and ERK1/2 signaling in sebocytes. These results suggest that isoginkgetin exerts its inhibitory role on sebum production via the inhibition of IGF-1 signaling. As notified, IGF-1 is one of important factors to affect the pathogenesis of acne1, thus efficient blockage of this signaling is a good strategy in the treatment of acne. In this regard, isoginkgetin can be applied as therapeutics for acne treatment.
In summary, we demonstrated that isoginkgetin inhibited IGF-1-induced sebum production in sebocytes, providing a novel candidate for acne drug.
ACKNOWLEDGMENT
This work was supported by the Technological Innovation R&D Program (S2315118) funded by the Small and Medium Business Administration (SMBA, Korea).
References
1. Shi VY, Leo M, Hassoun L, Chahal DS, Maibach HI, Sivamani RK. Role of sebaceous glands in inflammatory dermatoses. J Am Acad Dermatol. 2015; 73:856–863. PMID: 26386632.

2. Chen W, Obermayer-Pietsch B, Hong JB, Melnik BC, Yamasaki O, Dessinioti C, et al. Acne-associated syndromes: models for better understanding of acne pathogenesis. J Eur Acad Dermatol Venereol. 2011; 25:637–646. PMID: 21198949.

3. Kim H, Moon SY, Sohn MY, Lee WJ. Insulin-like growth factor-1 increases the expression of inflammatory biomarkers and sebum production in cultured sebocytes. Ann Dermatol. 2017; 29:20–25. PMID: 28223742.

4. Krautheim A, Gollnick HP. Acne: topical treatment. Clin Dermatol. 2004; 22:398–407. PMID: 15556726.

5. Hwang YL, Im M, Lee MH, Roh SS, Choi BW, Kim SJ, et al. Inhibitory effect of imperatorin on insulin-like growth factor-1-induced sebum production in human sebocytes cultured in vitro. Life Sci. 2016; 144:49–53. PMID: 26631504.

6. Smith TM, Gilliland K, Clawson GA, Thiboutot D. IGF-1 induces SREBP-1 expression and lipogenesis in SEB-1 sebocytes via activation of the phosphoinositide 3-kinase/Akt pathway. J Invest Dermatol. 2008; 128:1286–1293. PMID: 17989724.

7. Trivedi NR, Cong Z, Nelson AM, Albert AJ, Rosamilia LL, Sivarajah S, et al. Peroxisome proliferator-activated receptors increase human sebum production. J Invest Dermatol. 2006; 126:2002–2009. PMID: 16675962.

8. Lee SJ, Choi JH, Son KH, Chang HW, Kang SS, Kim HP. Suppression of mouse lymphocyte proliferation in vitro by naturally-occurring biflavonoids. Life Sci. 1995; 57:551–558. PMID: 7623623.

9. O'Brien K, Matlin AJ, Lowell AM, Moore MJ. The biflavonoid isoginkgetin is a general inhibitor of Pre-mRNA splicing. J Biol Chem. 2008; 283:33147–33154. PMID: 18826947.
10. Yoon SO, Shin S, Lee HJ, Chun HK, Chung AS. Isoginkgetin inhibits tumor cell invasion by regulating phosphatidylinositol 3-kinase/Akt-dependent matrix metalloproteinase-9 expression. Mol Cancer Ther. 2006; 5:2666–2675. PMID: 17121913.

Fig. 1
(A) Structure of isoginkgetin. (B) Cytotoxicity of isoginkgetin. Sebocytes were treated with isoginkgetin at the indicated concentrations for 2 days. Cell viability was measured by MTT assay. The mean values±standard deviation are averages of triplicate measurements. (C) Effect of isoginkgetin on lipogenesis in sebocytes. Cells were treated with insulin-like growth factor-1 (IGF-1) and isoginkgetin at the indicated concentrations for 2 days. Effect of isoginkgetin on IGF-1-induced lipid production was determined by thin layer chromatography. Production of squalene and wax ester was significantly inhibited by isoginkgetin.
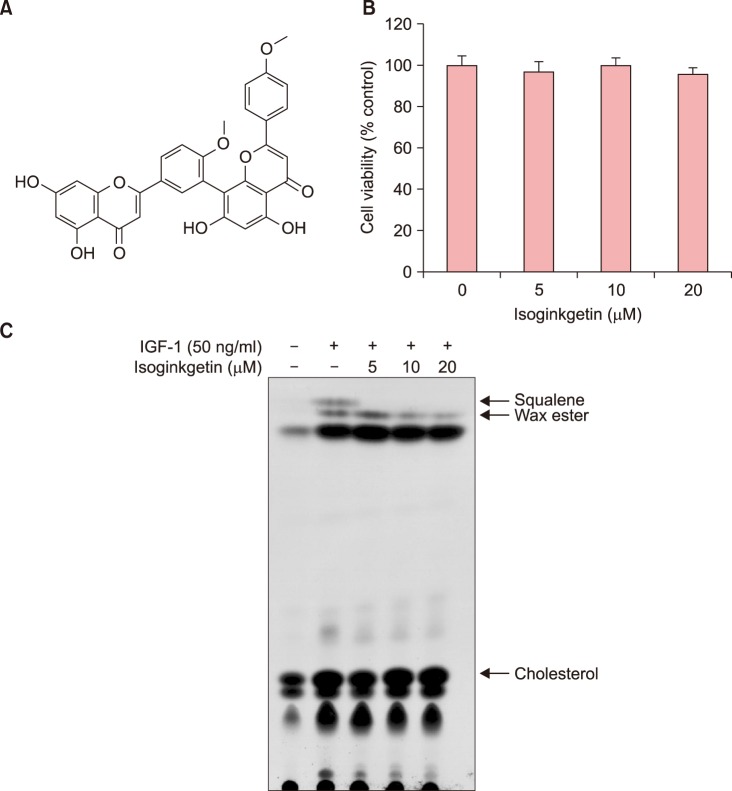
Fig. 2
(A) Effect of isoginkgetin on intracellular signaling. Sebocytes were pretreated with isoginkgetin at the indicated concentrations for 30 minutes, then insulin-like growth factor-1 (IGF-1) was added to the culture and incubated for a further 30 minutes. Cellular proteins were prepared and phosphorylation of signaling molecules was evaluated by Western blot. (B) Effect of isoginkgetin on the protein level for lipogenic transcription factors. Cells were treated with IGF-1 and isoginkgetin at the indicated concentrations for 2 days. Protein level for sterol response element-binding protein-1 (SREBP)-1 and peroxisome proliferator-activated receptor-γ (PPAR-γ) was evaluated by Western blot. Actin was used as a loading control.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download