Abstract
Purpose
PET/CT is useful in preoperative evaluation of invasive breast cancer (IBC) to predict axillary metastasis and staging workup. The usefulness is unclear in cases of ductal carcinoma in situ (DCIS) diagnosed at biopsy before surgery, which sometimes is upgraded to IBC after definitive surgery. The aim of this study is to find out the usefulness of PET/CT on DCIS as a preoperative evaluation tool.
Methods
We investigated 102 patients preoperatively diagnosed with DCIS who subsequently underwent definitive surgery between 2010 and 2015. The uptake of 18F-fluorodeoxyglucose was graded by visual and semiquantitative methods. We analyzed the maximum standardized uptake value (SUVmax) of each patient with clinicopathologic variables. We determined optimal cutoff values for SUVmax by receiver operating characteristic curve analysis.
Results
Fifteen cases out of 102 cases (14.7%) were upgraded to IBC after surgery. The SUVmax was higher in patients upgraded to IBC (mean: 2.56 vs. 1.36) (P = 0.007). The SUVmax was significantly higher in patients who had symptoms, palpable masses, lesions over 2 cm in size and BI-RAD category 5. Both visual and semiquantitative analysis were significant predictors of IBC underestimation. SUVmax of 2.65 was the theoretical cutoff value in ROC curve analysis in predicting the underestimation of IBC. The underestimation rate was significantly higher in patients with SUVmax >2.65 (P < 0.001), over the moderate enhanced uptake on visual analysis (P < 0.001).
About 14% of total breast cancer patients were newly diagnosed with ductal carcinoma in situ (DCIS) in Korea, and the incidence rate of DCIS has consistently increased every year [1]. DCIS is defined by malignant epithelial cells confined to the ductal system of the breast without invasion through the basement membrane into the surrounding stroma [2]. Axillary lymph node dissection (ALND) is not recommended for patients who are diagnosed with DCIS. After definite surgery, the final diagnosis is often upgraded to invasive breast cancer (IBC), thus, it is strongly recommended that patients undergo ALND or sentinel lymph node biopsy (SLNB).
For this reason, several studies have attempted to determine the preoperative clinical, radiologic, or pathologic risk factors of invasive cancer to avoid additional surgical treatment. However, there is still no consensus as to what the correct predictive factors are based on previous studies of the issue [34].
18F-fluorodeoxyglucose (18F-FDG) PET/CT has been used to detect various types of malignant tumors and to evaluate biological aggressiveness. Many studies have reported that the level of standardized uptake value (SUV) in IBC is strongly correlated with clinicopathological parameters and prognostic factors. Few studies have examined the association between the level of SUV and the underestimation of IBC in preoperatively diagnosed DCIS patients [56]. We therefore proposed to evaluate visual and semiquantitative assessments of 18F-FDG PET/CT to find out the usefulness of 18F-FDG PET/CT on DCIS patients as a preoperative evaluation tool.
Among 144 patients preoperatively diagnosed with DCIS who subsequently underwent definitive surgery between May 2010 and April 2015, we analyzed 102 cases who had received preoperative 18F-FDG PET/CT retrospectively. All of the patients were asked about their medical history, and received physical examinations, diagnostic mammographies, and ultrasonographic examinations. For the preoperative diagnostic procedure, ultrasound-guided core needle biopsies, ultrasound-guided vacuum-assisted breast biopsies (VABB), and excisional biopsies were performed according to the patient's symptoms and physician's choice. The clinicopathological variables, definitive treatments, and associated outcomes were reviewed in the hospital database. The surgical specimens were cut into serial sections of 5-mm thickness, and the final diagnoses were determined based on the results of immunohistochemistry analysis. This study was approved by Inje University Busan Paik Hospital Institutional Review Board (approval number: 16-0131) which waived the requirement for informed consent from individual patients because this study was a retrospective review of a patient database.
18F-FDG PET/CT images were obtained using a Discovery PET/CT scanner (GE Healthcare, Chicago, IL, USA). Before administration of 3–5 MBq/kg of 18F-FDG, patients fasted for at least 6 hours to ensure a serum glucose level of less than 150 mg/dL. Sixty minutes after administration of 18F-FDG, PET images were obtained containing 3.3-mm axial section CT scans and 1.25-mm section images were performed in the craniocaudal direction – the parameters were set to 120 kVp and 50 mAs using dose reduction software. 18F-FDG PET/CT was acquired with a 2-minute emission acquisition per bed position from the mid-thigh to the skull base. CT images were used as a transmission map for attenuation correction, and PET images were reconstructed using a conventional iterative algorithm (ordered subsets expectation-maximization, 2 iterations and 8 subsets with time of flight technique).
The 18F-FDG PET/CT scans were analyzed visually and semiquantitatively by the same person who performed the CT examinations. Lesions on CT images were localized at the time of analysis. The intensity of 18F-FDG uptake by breast lesions relative to the background activity in the uninvolved adjacent breast parenchyma and the mediastinum was assessed visually, and the intensities were scored with a 4-point scale (none, faint, moderate, or high) as follows: none, not visible on the image display; faint, less intense than mediastinal activity; moderate, same in intensity to mediastinal activity; and high, more intense than mediastinal activity. For semiquantitative analysis, a 10-mm2 circular volume of interest (VOI) was placed over the area exhibiting the peak tracer activity. This VOI was used to derive maximum standardized uptake values (SUVmax). The SUV was calculated using the following formula: SUV = activity in region of interest (MBq/mL) / injected dose (MBq/kg body weight). The SUVmax of breast was measured on a PET/CT data set. The SUVmax was defined as the maximum SUV in the VOI.
Data was expressed as median, range, and mean ± standard deviation. Comparisons between the baseline variables were made with the independent t-test for continuous variables and the Pearson chi-square test for categorical variables. Receiver operating characteristic (ROC) curves were conducted to determine the optimal cutoff values for detecting underestimation of invasive breast cancer and confirming axillary lymph node metastasis. The sensitivity, specificity, and positive and negative predictive values were determined at the optimal cutoff values by use of the ROC curves. All statistical tests were performed 2-sided, and a P-value < 0.05 was considered statistically significant.
Characteristics of the 102 patients included in this study are presented in Table 1. The mean age at diagnosis was 49.6 years (range, 27–82 years). In 7 patients (6.9%), core needle biopsies were performed as preoperative diagnoses. Thirty-eight patients (37.3%) underwent vacuum assisted breast biopsies and 57 patients (55.8%) underwent excision biopsies. Of the 57 patients who underwent excisions, 22 patients underwent needle localized excisions due to clustered microcalcifications visible on the mammography, and 4 patients underwent microdochectomies due to bloody nipple discharge.
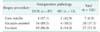
Fifteen patients (14.7%) were diagnosed with IBC at final surgery. We evaluated the association between clinicopathological variables and the SUVmax of the tumor (Table 2). The SUVmax was significantly higher in the patients who had symptoms, palpable masses (P = 0.001, P < 0.001), a lesion over 2 cm in size (P < 0.001), and BI-RAD category 5 (P = 0.049). There were no significant SUVmax differences with regard to nuclear grades and comedo necrosis. The upgrade rate by biopsy method was highest with core needle biopsies (42.9%) as compared with vacuum assisted breast biopsies (10.5%) and excision biopsies (14%) (Table 3). The SUVmax was higher in the patients upgraded to IBC (mean: 2.56 vs. 1.36), (P = 0.007).
A SUVmax of 2.65 was the theoretical cutoff value in ROC curve analysis in predicting the underestimation of IBC (Fig. 1). The underestimation rate was significantly higher in patients with a SUVmax > 2.65 (P < 0.001), over moderate enhanced uptake on visual analysis (P < 0.001), and positive axillary FDG uptake (P = 0.032) (Table 4). The sensitivity, specificity, and positive and negative predictive values of SUVtumor (>2.65), visual analysis over the moderate grade were 66.7%, 81.6%, 38.4% and 93.4%, and 66.7%, 77.0%, 33.3% and 93.1%, respectively. When SUVmax was added to clinical risk factors such as symptom presentation, palpability, and more than 2-cm-sized lesion, area under curve increased from 67% to 78% in multiple logistic regression analysis (Table 5).
We undertook 64 breast conserving surgeries (62.7%), 34 mastectomies (33.3%), and 4 nipple sparing mastectomies. Of 15 patients who were diagnosed with IBC, 6 patients were detected to have axillary lymph node involvement.
This study showed that 18F-FDG PET/CT would be helpful in predicting IDC in patients diagnosed with DCIS. The underestimation rate was significantly higher in patients with a SUVmax > 2.65 and patients with over moderate uptake and positive axillary FDG uptake on visual analysis.
It is widely accepted that axillary lymph node staging operation (ALND or SLNB) is not necessary during definitive surgery in pure DCIS patients. However, a proportion of DCIS patients are upgraded to IBC after definitive surgery because preoperative biopsies cannot represent the whole lesion [78]. ALND sometimes leads to arm lymphedema, though less frequently in SLNB. Therefore, it would be more ideal to avoid axillary staging operations when we can reveal that the primary breast lesion is pure DCIS.
The DCIS underestimation rate of preoperatively diagnosed patients showed a widely variable range depending on imaging modality, needle gauges, and biopsy procedures. DCIS underestimation rates of 11%–59% have been reported and a meta-analysis study identified that the random-effects pooled estimate was 25.9% [491011]. The overall DCIS underestimation rate of our study was 14.7% (15 of 102). This rate was relatively lower than other studies. The reason is that our study contained a large proportion of VABB and excisional biopsies. Underestimation of IBC is known to be lower in VABB and excisional biopsies in which the volume of biopsy is much higher than that of core needle biopsies.
Much effort has been made to determine the key factors in predicting the underestimation of IBC, such as analyzing clinicopathologic factors, sonography, and MRI. Many studies have reported that the underestimation of IBC was associated with preoperative clinical, radiologic or pathologic variables [12]. A higher underestimation rate was significantly related to symptoms, lesion palpability, thin biopsy devices, high BI-RADS scores, high nuclear grades, and comedo necrosis. Our study showed that upgraded rates of IBC were significantly higher in patients with symptoms, palpable masses, a lesion size of over 2 cm, and high BI-RAD scores. However, there were no significant difference with nuclear grade and comedo necrosis. These variables related to underestimation are insufficient to skip the ALND or SLNB in patients diagnosed with DCIS preoperatively because they lack objectivity. To supplement this problem, recent studies have focused on the clinical significance of the biological aggressiveness of DCIS.
18F-FDG PET/CT is an imaging tool, which can evaluate the glucose metabolism of tumors. It, therefore, is widely used for diagnosing tumors, assessing treatment responses, and patient follow-up in various kinds of tumors including breast cancer. Furthermore, metabolic parameters such as SUVmax, metabolically active tumor volume, and total lesion glycolysis indicating the glucose metabolism of tumors are known as independent prognostic factors [513]. Previous studies have revealed that the high level of SUVmax was significantly associated with large tumor size, lymph node involvement, high nuclear grade, lymphovascular invasion, negative hormone receptor status, and positive HER2 status in IBC patients. Thus, the SUVmax of 18F-FDG PET/CT has been a poor prognostic factor [1415].
Many studies have placed more emphasis on IBC rather than DCIS. Recently, Shigematsu et al. [16] conducted a study that showed 18F-FDG PET/CT played a major role in predicting the underestimation of IBC in cases of DCIS at needle biopsy. They showed that a high SUVmax was significantly related to symptomatic presentation, palpation, mass formation, high BI-RADS scores, and core needle biopsy. They concluded that SUVmax is a significant predictive factor of the underestimation of IBC. This finding is similar to our results and our study shows there were no significant differences with nuclear grade and comedo necrosis. When a proper cutoff value on 18F-FDG PET/CT was identified using an ROC curve, high SUVmax values had a strong influence on predicting underestimation of IBC including conventional clinical risk factors, such as symptomatic presentation, palpability and larger lesion size. Our optimal SUVmax cutoff value on ROC curve for predicting underestimation of IBC was 2.65. SUVmax of more than 2.65 was the only significant predictive value of underestimation of IBC, and clinical risk group with SUVmax had more influence on predicting underestimation of IBC than without SUVmax in multiple logistic regression analysis. Our SUVmax cutoff value was higher than in other studies. In our institution, VABB and excisional biopsies were performed more frequently to achieve correct diagnosis. VABB and excisional biopsies increase inflammatory reaction after procedure and cause increases in SUVmax values.
In general, 18F-FDG PET/CT scans had been analyzed visually and semiquantitatively. Visual and semiquantitative (SUVmax) assessments can differentiate malignant from benign lesions equally regarding other organs [1718]. We therefore added visual analysis as a qualitative method and axillary FDG uptake to increase the negative predictive value. Because breast physiological activities are variable according to the patient, we attempted to assess the visual analysis by comparing it with normal parenchymal activity. There were no underestimated cases below the moderate uptake cases. Qualitative assessments by visual analysis would also be a useful predictive factor in the underestimation of IBC.
Our study has some limitations. First, our current study was a retrospective review. Second, a relatively small sample size at a single institution was examined. Therefore, further investigation will be required to include a larger sample size at multiple institutions prospectively. Finally, there was the limitation of using 18F-FDG PET/CT on DCIS patients. Using 18F-FDG PET/CT on DCIS patients is currently still open to dispute. Therefore, further prospective studies are necessary to establish the proper indications among the clinicopathological risk factors.
In conclusion, 18F-FDG PET/CT can be a complementary diagnostic tool in predicting the underestimation of IBC in preoperative DCIS patients. Especially high SUVmax values with symptom presentation, palpability, and larger lesion size can help clinicians decide whether these patients should undergo ALND. SUVmax can vary depending on preoperative diagnostic methods, so further studies are necessary to establish the appropriate cutoff value of SUVmax on 18F-FDG PET/CT.
Figures and Tables
Fig. 1
Receiver operating characteristic curve of maximum standardized uptake valvue (SUVmax) for predicting underestimation of invasive breast cancer. Optimal cutoff of SUVmax was 2.65 (n = 102).

References
1. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a Nationwide Survey and Breast Cancer Registry Database. J Breast Cancer. 2016; 19:1–7.

2. Siziopikou KP. Ductal carcinoma in situ of the breast: current concepts and future directions. Arch Pathol Lab Med. 2013; 137:462–466.

3. Park AY, Gweon HM, Son EJ, Yoo M, Kim JA, Youk JH. Ductal carcinoma in situ diagnosed at US-guided 14-gauge core-needle biopsy for breast mass: preoperative predictors of invasive breast cancer. Eur J Radiol. 2014; 83:654–659.

4. Brennan ME, Turner RM, Ciatto S, Marinovich ML, French JR, Macaskill P, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011; 260:119–128.

5. Ueda S, Tsuda H, Asakawa H, Shigekawa T, Fukatsu K, Kondo N, et al. Clinicopathological and prognostic relevance of uptake level using 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in primary breast cancer. Jpn J Clin Oncol. 2008; 38:250–258.

6. Kadoya T, Aogi K, Kiyoto S, Masumoto N, Sugawara Y, Okada M. Role of maximum standardized uptake value in fluorodeoxyglucose positron emission tomography/computed tomography predicts malignancy grade and prognosis of operable breast cancer: a multi-institute study. Breast Cancer Res Treat. 2013; 141:269–275.

7. Chin-Lenn L, Mack LA, Temple W, Cherniak W, Quinn RR, Ravani P, et al. Predictors of treatment with mastectomy, use of sentinel lymph node biopsy and upstaging to invasive cancer in patients diagnosed with breast ductal carcinoma in situ (DCIS) on core biopsy. Ann Surg Oncol. 2014; 21:66–73.

8. Sato Y, Kinoshita T, Suzuki J, Jimbo K, Asaga S, Hojo T, et al. Preoperatively diagnosed ductal carcinoma in situ: risk prediction of invasion and effects on axillary management. Breast Cancer. 2016; 23:761–770.

9. Park AY, Gweon HM, Son EJ, Yoo M, Kim JA, Youk JH. Ductal carcinoma in situ diagnosed at US-guided 14-gauge core-needle biopsy for breast mass: preoperative predictors of invasive breast cancer. Eur J Radiol. 2014; 83:654–659.

10. Park SH, Kim MJ, Kim SJ, Kim EK. Ductal carcinoma in situ diagnosed using an ultrasound-guided 14-gauge core needle biopsy of breast masses: can underestimation be predicted preoperatively? Ultrasonography. 2014; 33:128–135.

11. Shin SH, Kim BC, Song YJ, Yoon HC, Cho JS, Park MH, et al. Risk factor of invasive breast cancer in patients with preoperative diagnosis of ductal carcinoma in situ. J Korean Surg Soc. 2011; 80:90–95.

12. Nori J, Meattini I, Giannotti E, Abdulcadir D, Mariscotti G, Calabrese M, et al. Role of preoperative breast MRI in ductal carcinoma in situ for prediction of the presence and assessment of the extent of occult invasive component. Breast J. 2014; 20:243–248.
13. Berriolo-Riedinger A, Touzery C, Riedinger JM, Toubeau M, Coudert B, Arnould L, et al. [18F]FDG-PET predicts complete pathological response of breast cancer to neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2007; 34:1915–1924.

14. Ohara M, Shigematsu H, Tsutani Y, Emi A, Masumoto N, Ozaki S, et al. Role of FDG-PET/CT in evaluating surgical outcomes of operable breast cancer: usefulness for malignant grade of triple-negative breast cancer. Breast. 2013; 22:958–963.
15. Morris PG, Ulaner GA, Eaton A, Fazio M, Jhaveri K, Patil S, et al. Standardized uptake value by positron emission tomography/computed tomography as a prognostic variable in metastatic breast cancer. Cancer. 2012; 118:5454–5462.

16. Shigematsu H, Kadoya T, Masumoto N, Matsuura K, Emi A, Kajitani K, et al. Role of FDG-PET/CT in prediction of underestimation of invasive breast cancer in cases of ductal carcinoma in situ diagnosed at needle biopsy. Clin Breast Cancer. 2014; 14:358–364.
17. Hashimoto Y, Tsujikawa T, Kondo C, Maki M, Momose M, Nagai A, et al. Accuracy of PET for diagnosis of solid pulmonary lesions with 18F-FDG uptake below the standardized uptake value of 2.5. J Nucl Med. 2006; 47:426–431.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download