Abstract
Background
In patients who need sustained endotracheal intubation and mechanical ventilation due to respiratory failure after traumatic cervical spinal cord injury, tracheostomy can be performed to reduce the duration of mechanical ventilation and respiratory complications. The purpose of this study was to determine criteria and timing of tracheostomy in patients with severe traumatic cervical spinal cord injury accompanied by motor weakness.
Methods
We reviewed 22 patients who underwent tracheostomy (study group) and 27 patients who did not (control group) from January 2005 to March 2016. We assessed the American Spinal Injury Association (ASIA) impairment scale score and investigated accompanying thoracic injury, paradoxical respiration, postoperative endotracheal intubation and other clinical parameters. The study group was also subdivided into the early tracheostomy group and late tracheostomy group depending on whether the tracheostomy was performed within or later than 7 days after surgery.
Results
Twenty-two patients in the study group had a mean ASIA impairment scale score of 14.1 points, which was lower than the control group's 23.4 points. Paradoxical respiration was observed in 77% of the patients in the study group compared to 18% in the control group. Postoperative intubation was maintained in 68% in the study group; 32% underwent endotracheal intubation due to respiratory failure within 4 days after surgery and had a tracheostomy. In the control group, postoperative intubation was maintained in 22%, and all of them were weaned off intubation within 4 days after surgery. The duration of intensive care unit hospitalization was 11.4 days for the early tracheostomy group, which was shorter than the late tracheostomy group's 19.7 days.
Conclusions
In patients with severe traumatic cervical spinal cord injury, tracheostomy may be needed when the motor grade of the ASIA scale is low, above the C4 segment is injured, or paradoxical respiration occurs after injuries. In addition, if endotracheal extubation is not feasible within 4 days after surgery, an early tracheostomy should be considered.
Traumatic cervical cord injuries can cause multiple organ dysfunction and complications:1) such injuries often cause neurologic disorders, paralysis, and dysfunction of respiratory muscles, which result in secondary complications. They remain as one of the most common causes of increased morbidity and mortality.234) Also, respiratory complications are one of the most common causes of death in multiple trauma patients.23)
Many patients with traumatic cervical cord injuries need sustained implementation of mechanical ventilation. 15) Among 21%–77% of these patients, tracheostomy, rather than endotracheal intubation, is needed to make breathing more comfortable and more efficient by reducing dead-space ventilation.5) In addition, the known advantages of tracheostomy include stable airway, possible oral nutrition, efficient management of tracheal secretions, and reduced respiratory complications.67891011) However, tracheostomy may lead to complications such as airway stenosis, hemorrhage, infection at the operation site, and dysphagia because it is an invasive procedure.
Early tracheostomy has a positive effect on the prognosis of the patient by reducing the duration of mechanical ventilation and length of stay in the intensive care unit (ICU) and improves patient tolerance to mechanical ventilation.68101213) The need for a tracheostomy is usually determined based on the level of neurological injury, age, and other accompanying injuries in patients with traumatic cervical spinal cord injuries; however, the criteria for early tracheostomy remain controversial.81011) The purpose of this study is to determine the proper criteria and timing for early tracheostomy in patients with severe traumatic cervical spinal cord injury accompanied by motor weakness.
This study was performed retrospectively on 49 patients with motor weakness whose muscle strength score of American Spinal Injury Association (ASIA) impairment scale was under 50 after surgery for cervical spinal injury. We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-2017-316). Written informed consents were obtained from all subjects. The patients underwent surgical treatment for traumatic cervical spinal injury at Chonnam National University Hospital from January 2005 to March 2016. Of those, 22 patients had tracheostomy: 10 within 7 days after surgery and the rest later than 7 days after surgery.
The patient's age, sex, degree of injury, level of injury, presence of accompanied thoracic injuries, presence of paradoxical respiration, period before tracheostomy, continuation of intubation after surgery for cervical spinal cord injury, length of ICU stay, and amount of tracheal secretion were investigated. The severity of injury was measured based on the muscle strength score of the ASIA impairment scale, and the level of injury was determined as the highest level of the segment injured, which was detected by simple radiography and computed tomography. Paradoxical respiration was considered present when the doctor in charge or a specialist doctor observed contraction of abdominal muscles during respiration from injury to surgery. The amount of respiratory secretion was assessed based on the number of times the nurse in charge of ICU performed aspiration per hour: 0 point was given for less than once per hour; 1 point, for once; 2 points, for twice; and 3 points, for three times per hour.
Descriptive statistics (arithmetic mean, standard deviation, and range) were calculated using SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). The independent t-test was used to determine the significance of intergroup differences. A p-value < 0.05 was considered significant and the statistical analysis was performed by an independent statistician.
The characteristics of the two groups are summarized in Table 1. Of the total 49 patients who underwent surgery for traumatic cervical spinal cord injury with motor weakness, 22 patients (19 males and 3 females) with a mean age of 55.4 years (range, 26 to 70 years) underwent tracheostomy. In them, the mean ASIA impairment scale score for muscle strength was 14.1 points at the time of injury, which was statistically significantly lower than the average of 23.4 points of 27 patients in the non-tracheostomy group (25 males and 2 females) with a mean age of 52.3 years (range, 17 to 81 years) (p = 0.034).
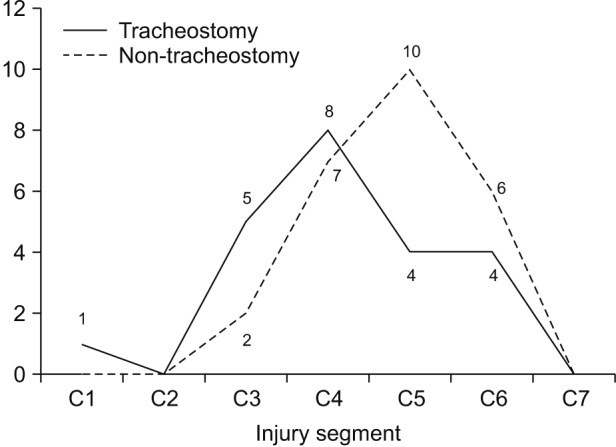
The tracheostomy group had damage to the higher segments (Fig. 1). The average level of injury in the tracheostomy group was at C4.18 (range, C1 to C6), whereas the average level in the control group was at C4.96 (range, C3 to C7), showing a statistically significant difference between groups (p = 0.011). There was no statistically significant difference between the two groups in the incidence of associated thoracic injury: 18% (four patients) in the tracheotomy group vs. 14% (four patients) in the non-tracheotomy group. A statistically significant difference was observed in the presence of paradoxical respiration between the two groups (p < 0.001): 77% (17 patients) in the tracheotomy group vs. 18% (five patients) in the non-tracheotomy group. The score for the assessment of the amount of tracheal secretion was 2.32 points in the tracheostomy group and 0.67 point in the non-tracheotomy group, showing a statistically significant difference between groups (p < 0.001).
In the tracheostomy group, tracheostomy was performed at a mean of 7.5 days (range, 1 to 29 days) after surgery. Of the 22 patients in the tracheostomy group, intubation was maintained after surgery in 68% (14 patients) and 32% (eight patients) showed respiratory failure accompanied by increased tracheal secretion and respiratory muscle fatigue, so intubation was performed within 4 days after surgery. All of them underwent tracheostomy for sustained mechanical ventilation. In the non-tracheostomy group, intubation was maintained in 22% (five patients) of 27 patients after surgery and removed within 4 days after surgery in all patients (Fig. 2).
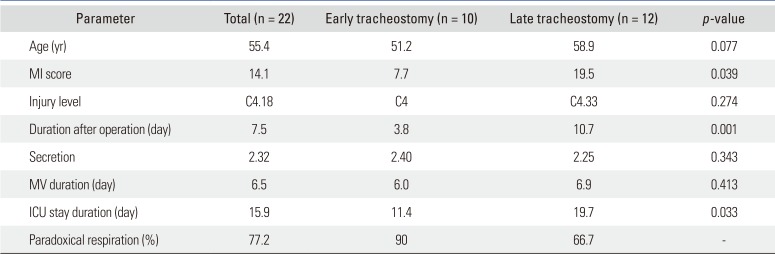
The characteristics of the two groups are summarized in Table 2. Ten patients (eight males and two females; average age, 51.2 years [range, 33 to 73 years]) who underwent tracheostomy within 7 days after surgery (early tracheostomy group) had a mean ASIA impairment scale score of 7.7 points at the time of injury, which was statistically significantly lower than the mean 19.5 points of 12 patients in the late tracheostomy group who underwent tracheostomy later than 7 days after surgery (11 males and one female; average age, 58.9 years [range, 26 to 70 years]) (p = 0.039). The duration of postoperative sustained mechanical ventilation was shorter in the early tracheostomy group (6 days), but the difference was not statistically significant (p = 0.41). The duration of postoperative ICU hospitalization was 11.4 days in the early tracheostomy group, which was shorter than that of the late tracheostomy group (19.7 days), showing statistically significant difference (p = 0.033).
Among patients who had surgery for traumatic cervical cord injury accompanied by motor weakness, the lower motor weakness score of the ASIA impairment scale, higher injury level, and paradoxical respiration were associated with the greater need for tracheostomy. Furthermore, respiratory failure and increased tracheal secretion persisting for more than 4 days after surgery necessitated continuous mechanical ventilation and in this case, early tracheostomy could reduce the duration of ICU stay.
The patients who have acute spinal cord injury have an increased risk of respiratory failure, followed by respiratory disease, such as pneumonia, and mortality due to complications. In many cases, prolonged mechanical ventilation is needed after endotracheal intubation to prevent respiratory complications and to treat respiratory failure after spinal cord injury. Furthermore, tracheostomy may also be needed to prevent complications due to prolonged endotracheal intubation in many cases.14)
Patients with traumatic cervical spinal cord injury are susceptible to respiratory complications due to neurological injury of respiratory muscles of the diaphragm, thoracic spine, and abdomen, which results in reduction of vital capacity and reserve volumes.15) It is known that acute cervical spinal cord injury can affect descending reticulospinal respiratory pathways that control the diaphragm, intercostal muscles, accessory respiratory muscles, and abdominal muscles causing muscular dysfunction. Ultimately, it leads to reduced vital capacity and static oral pressure, weakened cough, and disorder of removal of foreign body, and it can increase rates of atelectasis and respiratory infection. It is known that endotracheal intubation and mechanical ventilation can not only reduce respiratory failure and complications following surgery for acute cervical spinal cord injury but also prevent spinal cord injury due to secondary hypoxia.16)
Although there is no clear evidence that tracheostomy reduces ventilator-associated pneumonia, it is reported that it can reduce the duration of mechanical ventilation and ICU hospital stay.101517) In this study, we also confirmed that tracheostomy could reduce the duration of ICU hospital stay. Additional benefits of the procedure include easier patient management for nurses, disposal of secretion, patient comfort, feasibility of deglutition movement, and early vocalization. However, misplaced needles and cannulae, fracture of cricoid cartilage, injury of the posterior wall of the trachea, hemorrhage, pneumothorax, emphysema, wound infection, and mediastinitis are inherent risks of the invasive procedure, which can lead to death in severe cases.181920) It has been reported that the mortality rate of tracheostomy ranges from 1.1% to 8.9% in adults; major causes of death include post-procedure hemorrhage and airway obstruction and infection due to wrong trachea incision tube insertion.21) Therefore, tracheostomy should be determined on the basis of assessment of benefits and risks of the procedure.
In the past, tracheotomy was performed as late as possible to prevent traumatic organ injury in patients requiring continuous mechanical ventilation. Recently, however, persistent tracheal intubation has been known to cause various complications, and advantages of tracheostomy are being highlighted. Therefore, early tracheostomy is being recognized as a good treatment option, and some studies have reported that early tracheostomy reduces ICU mortality and hospital mortality.222324252627) However, there is still controversy regarding the proper timing of tracheostomy in patients with traumatic spinal cord injuries. So, we set out this study to determine the criteria and timing for early tracheostomy in patients with severe traumatic cervical spinal cord injury with motor weakness.
In previous studies, an injury to the segment above the fourth cervical vertebra and low strength scores of the ASIA impairment scale were associated with the need for tracheostomy.81011) Based on our findings in this study, we suggest that tracheostomy should also be performed in case of paradoxical respiration or persisting increased secretion. In addition, if tracheal extubation is not feasible within 4 days after surgery, early tracheostomy should be considered because continuous mechanical ventilation will be needed.
Despite the concern over the risk of infection at the previous surgical site after tracheostomy in patients with anterior cervical spine fusion or fixation, there is very little research on this. In the current study, there was no statistically significant increase in cervical spine infections after anterior cervical spine fusion, and none of the patients with tracheostomy had surgical site infection. According to Northrup et al.,14) the correlation between tracheostomy and infection after anterior cervical spine surgery seems to be low.
There are some limitations in this study. First, only a small number of patients were studied because only patients with symptomatic traumatic cervical spinal cord injury in a single institution were included. Second, paradoxical respiration and the amount of secretion may be different depending on observers because they are subjective criteria, rather than objectively, quantifiable criteria.
In patients with traumatic cervical spinal cord injuries, tracheostomy is highly likely to be needed when the motor grade of the ASIA impairment scale score is low, the injury level is higher than C4, or paradoxical respiration and increased secretion are observed. Furthermore, if intubation was required for more than 4 days after operation, early tracheostomy should be considered.
References
1. Mansel JK, Norman JR. Respiratory complications and management of spinal cord injuries. Chest. 1990; 97(6):1446–1452. PMID: 2189697.

2. National Spinal Cord Injury Statistical Center, University of Alabama at Birmingham. 10 Annual report for the spinal cord injury model system. Birmingham, AL: National Spinal Cord Injury Statistical Center;2011.
3. Nakajima A, Honda S, Yoshimura S, Ono Y, Kawamura J, Moriai N. The disease pattern and causes of death of spinal cord injured patients in Japan. Paraplegia. 1989; 27(3):163–171. PMID: 2762003.

4. Neumann CR, Brasil AV, Albers F. Risk factors for mortality in traumatic cervical spinal cord injury: Brazilian data. J Trauma. 2009; 67(1):67–70. PMID: 19590310.

5. Ball PA. Critical care of spinal cord injury. Spine (Phila Pa 1976). 2001; 26(24 Suppl):S27–S30. PMID: 11805605.

6. Berney S, Stockton K, Berlowitz D, Denehy L. Can early extubation and intensive physiotherapy decrease length of stay of acute quadriplegic patients in intensive care? A retrospective case control study. Physiother Res Int. 2002; 7(1):14–22. PMID: 11992981.

7. Brook AD, Sherman G, Malen J, Kollef MH. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care. 2000; 9(5):352–359. PMID: 10976359.

8. Branco BC, Plurad D, Green DJ, et al. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma. 2011; 70(1):111–115. PMID: 20526209.

9. Fishburn MJ, Marino RJ, Ditunno JF Jr. Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil. 1990; 71(3):197–200. PMID: 2317137.
10. Goettler CE, Fugo JR, Bard MR, et al. Predicting the need for early tracheostomy: a multifactorial analysis of 992 intubated trauma patients. J Trauma. 2006; 60(5):991–996. PMID: 16688060.

11. Harrop JS, Sharan AD, Scheid EH Jr, Vaccaro AR, Przybylski GJ. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg. 2004; 100(1 Suppl Spine):20–23. PMID: 14748569.

12. Kluger Y, Paul DB, Lucke J, et al. Early tracheostomy in trauma patients. Eur J Emerg Med. 1996; 3(2):95–101. PMID: 9028753.

13. Palmieri TL, Jackson W, Greenhalgh DG. Benefits of early tracheostomy in severely burned children. Crit Care Med. 2002; 30(4):922–924. PMID: 11940771.

14. Northrup BE, Vaccaro AR, Rosen JE, Balderston RA, Cotler JM. Occurrence of infection in anterior cervical fusion for spinal cord injury after tracheostomy. Spine (Phila Pa 1976). 1995; 20(22):2449–2453. PMID: 8578397.

15. Milanchi S, Magner D, Wilson MT, Mirocha J, Margulies DR. Percutaneous tracheostomy in neurosurgical patients with intracranial pressure monitoring is safe. J Trauma. 2008; 65(1):73–79. PMID: 18580518.

16. Berlly M, Shem K. Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med. 2007; 30(4):309–318. PMID: 17853652.

17. Arabi YM, Alhashemi JA, Tamim HM, et al. The impact of time to tracheostomy on mechanical ventilation duration, length of stay, and mortality in intensive care unit patients. J Crit Care. 2009; 24(3):435–440. PMID: 19327302.

18. Epstein SK. Late complications of tracheostomy. Respir Care. 2005; 50(4):542–549. PMID: 15807919.
19. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med. 1981; 70(1):65–76. PMID: 7457492.

20. De Leyn P, Bedert L, Delcroix M, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007; 32(3):412–421. PMID: 17588767.

21. Stemmer EA, Oliver C, Carey JP, Connolly JE. Fatal complications of tracheotomy. Am J Surg. 1976; 131(3):288–290. PMID: 769582.

22. Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984; 94(3):367–377. PMID: 6700353.

23. Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg. 2000; 123(4):495–500. PMID: 11020193.

24. Esteller More E, Ibanez-Nolla J, Garcia-Hernandez F, et al. Post-mortem study of laryngotracheal lesions produced by prolonged intubation and/or tracheotomy. Acta Otorrinolaringol Esp. 1997; 48(7):545–550. PMID: 9489156.
25. Esteller-More E, Ibanez J, Matino E, Adema JM, Nolla M, Quer IM. Prognostic factors in laryngotracheal injury following intubation and/or tracheotomy in ICU patients. Eur Arch Otorhinolaryngol. 2005; 262(11):880–883. PMID: 16258758.

26. Cosortium for Spinal Cord Medicine. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005; 28(3):259–293. PMID: 16048145.
27. Cox CE, Carson SS, Holmes GM, Howard A, Carey TS. Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993-2002. Crit Care Med. 2004; 32(11):2219–2226. PMID: 15640633.

Fig. 2
(A) Duration until postoperative intubation in tracheostomy patients: intubation was required in all patients until postoperative day (POD) 4. (B) Duration until extubation in non-tracheostomy patients: extubation was performed within POD 4. OP: operative.
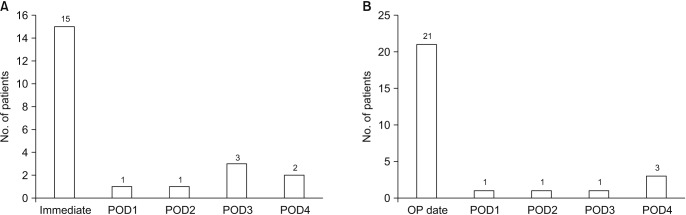
Table 1
Characteristics of Patients with and without Tracheostomy
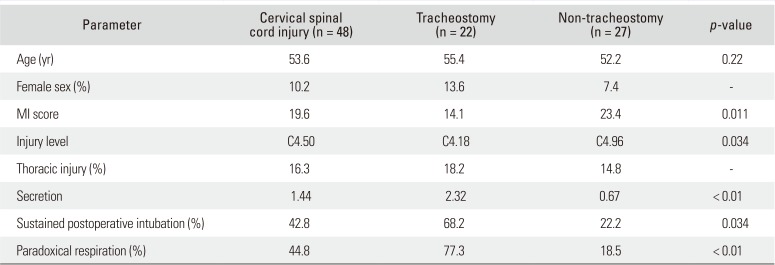
Table 2
Characteristics of Patients with Early and Late Tracheostomy




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download