TO THE EDITOR: Polycythemia vera (PV) is a chronic myeloproliferative disorder with panmyelosis that is unrelated to a secondary cause. Although the discovery of JAK2 V617F mutation in the pathogenetic mechanism of PV has made the diagnosis clearer and easier, until recently, diagnosis of PV involved excluding secondary causes of erythrocytosis in clinical practice. Among the secondary causes, smoking history, elevated erythropoietin (EPO) level, and hypoxemia measured by arterial blood gas analysis are well known and recognized as minor criteria for the diagnosis of PV. With the upfront evaluation of JAK2 mutation status in patients with erythropoiesis, clinicians are apt to be neglectful about the evaluation of these secondary causes. However, based on our case, evaluation of other causes is clinically significant.
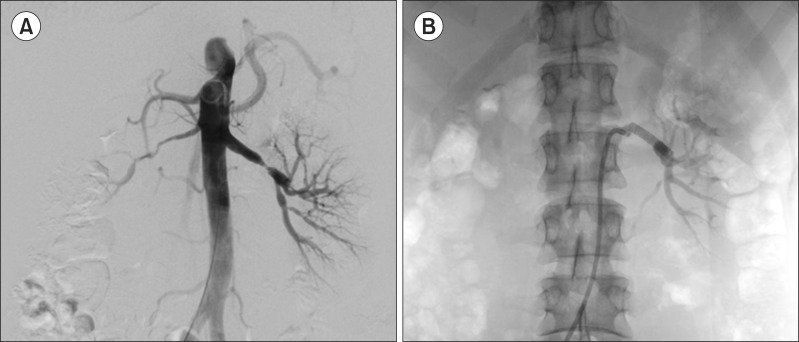
A 30-year-old woman presented with headache, hypertension, and abnormal laboratory findings on routine health examination. Her initial blood pressure was 190/140 mmHg, and pulse rate was 84 beats/min. The laboratory testing yielded a white blood cell count of 22.5×109/L hemoglobin at 22.5 g/dL, hematocrit level at 66.9%, and platelet count of 400.0×109/L. Physical examination revealed mild splenomegaly. She did not have hypoxemia and had never smoked. Sequentially performed bone marrow aspiration and biopsy revealed panmyelosis consistent with PV, and molecular testing revealed the presence of JAK2 V617F mutation. However, the consequently identified EPO level was elevated to 470 mIU/mL, and hypertension, which was initially considered to be caused by polycythemia, persisted after phlebotomy. For the exploration of secondary hypertension with an elevated EPO level, we performed CT angiography covering the adrenal glands and renal arteries and found irregular severe stenosis of the right renal artery and multifocal irregular stenosis of the left renal artery. Moreover, her right kidney was severely atrophied (Fig. 1). Anti-nuclear antibody (ANA), anti-neutrophil cytoplasmic antibody (ANCA), C3, C4, and lipid profile were all within normal range. We continued with intermittent phlebotomy for the management of PV and decided to perform angioplasty of the narrowed renal artery (Fig. 2). Additionally, we prescribed the anti-platelet agent clopidogrel because the patient had aspirin hypersensitivity. Two months after the angioplasty with stent insertion in the left renal artery, her blood pressure stabilized with clonidine alone, and her hemoglobin level decreased spontaneously to 13.7 g/dL. Therefore, she did not need additional phlebotomy or any cytotoxic medication such as hydroxyurea.
To date, only a few cases of PV combined with renal artery stenosis (RAS) have been reported, and we do not know whether these two disease entities have a causal relationship. Although RAS is known to impair renal perfusion and subsequently increases EPO secretion and leads to secondary erythrocytosis, it is not obvious whether the elevated EPO level caused by RAS could induce an acquired mutation. In 1965, Luke et al. [1] reported the first case of RAS combined with PV and severe hypertension in a 54-year-old man. However, JAK2 V617F mutation analysis was not available at that time. Therefore, it is possible that the erythrocytosis was secondary to the RAS. Later, a few similar cases, which were confirmed as having PV or essential thrombocythemia (ET) by bone marrow biopsy or mutation analysis, were reported; no pathogenetic mechanism of coexisting PV and RAS was mentioned [2, 3, 4].
PV is known to be associated with thrombotic risks. Theoretically, the increase in red blood cell mass is known to displace platelets toward the vessel wall and facilitate shear-induced platelet activation. Moreover, in patients with PV or ET, biochemical changes in the cell membrane and intracellular contents of red blood cell can increase red blood cell aggregation and thrombogenesis [5]. On the other hand, damage to the vascular structure itself or atherosclerosis has not been recognized as a major complication of PV because vascular effects by PV are mostly limited to the endothelium, which is insufficient for vascular stenosis, especially in large vessels. However, a few studies revealed that hyperproliferation of erythrocytes, leukocytes, or platelets could damage vascular endothelial cells, and this damage could cause fibromuscular intimal proliferation of the artery without thrombotic occlusion [6].
RAS is caused chiefly by atherosclerosis or fibromuscular dysplasia (FMD). Atherosclerosis commonly occurs at the origin or the proximal portion of the artery in older patients with typical cardiovascular risk factors. In contrast, FMD occurs in the middle or distal arterial segments in younger patients without cardiovascular risk factors. FMD is a non-atherosclerotic, non-inflammatory vascular disease that most commonly affects the renal artery. Although a variety of genetic, mechanical, and hormonal factors have been proposed, the principal pathogenetic mechanism of FMD remains uncertain [7]. As mentioned above, we do not know the exact underlying mechanism that was predominant in our case because we did not perform a pathologic evaluation of the patient's renal artery. Although we presume FMD to be the main mechanism because of the patient's young age and the location of renal arterial stenosis, both mechanisms can be explained in connection with the secondary effect of PV or ET. A review of related literature revealed conflicting reports. First, Hua et al. [4] who reported a PV patient with multiple intracranial and extracranial steno-occlusive diseases, insisted that the large vessel steno-occlusion is due to hyperplasia of smooth muscle cells and luminal thrombosis rather than atherosclerosis or inflammation. Furthermore, they presented a few similar cases of sickle cell anemia or ET for reference with the explanation that progressive intimal and medial wall proliferation can be caused by endothelial irritation and edema due to repeated microvascular thrombosis [4]. However, Gavriilaki et al. [8] insisted that PV may lead to atherosclerosis and subsequent atherosclerotic RAS based on their case report and supported that theory by thrombotic restenosis, which occurred following a period of high hematocrit levels after stenting. Notably, Cucuianu et al. [9] performed arterial Doppler ultrasonography in 37 patients with PV (29) and ET (8); they found significant arterial stenosis in 23 patients (62.1%) including 10 patients with peripheral arterial stenosis. The possible relevance was explained by hyperactivation of JAK2 activating STAT5 (a promoter of angiogenesis) and accelerating hyperplasia of vascular endothelia leading to atherosclerotic plaque. Another previous study showed that a high-sensitivity C-reactive protein level significantly correlated with the JAK2 V617F allele burden, and explained that accelerated atherosclerosis could be caused by PV or ET through chronic inflammatory mechanism [10]. Because identifying the relationship between PV and RAS has therapeutic implications, further prospective, large-scale studies are warranted.
In summary, our case and a few previous reports demonstrate that there is a possible mutual relationship between PV and RAS. Therefore, elevated EPO levels and hypertension in patients with JAK2 mutation positive PV should not be overlooked in clinical practice. Moreover, evaluation of vascular stenosis and treatment planning based on the result should be considered in patients with PV or ET.
References
1. Luke RG, Kennedy AC, Stirling WB, Mcdonald GA. Renal artery stenosis, hypertension, and polycythaemia. Br Med J. 1965; 1:164–166. PMID: 14222595.

2. Biggs B, Anderton JL. Reno-vascular disease in polycythaemia rubra vera. Postgrad Med J. 1983; 59:382–383. PMID: 6634546.

3. Hur JW, Lee YY, Lee WS, Jun JB. Erythromelalgia as a presenting manifestation in a patient with essential thrombocythemia complicating renovascular hypertension due to unilateral renal artery stenosis. Rheumatol Int. 2005; 26:83–85. PMID: 15750823.

4. Hua le H, Dodd RL, Schwartz NE. Concurrent stenoocclusive disease of intracranial and extracranial arteries in a patient with polycythemia vera. Case Rep Med. 2012; 2012:151767. PMID: 22690222.
5. Finazzi G, De Stefano V, Barbui T. Are MPNs vascular diseases? Curr Hematol Malig Rep. 2013; 8:307–316. PMID: 24037420.

6. Bellucci S, Michiels JJ. The role of JAK2 V617F mutation, spontaneous erythropoiesis and megakaryocytopoiesis, hypersensitive platelets, activated leukocytes, and endothelial cells in the etiology of thrombotic manifestations in polycythemia vera and essential thrombocythemia. Semin Thromb Hemost. 2006; 32:381–398. PMID: 16810614.

8. Gavriilaki E, Sampanis N, Kavlakoudis C, Papaioannou G, Vasileiou S. An exceptional case of renal artery restenosis in a patient with polycythaemia vera. Blood Coagul Fibrinolysis. 2014; 25:904–906. PMID: 24991947.

9. Cucuianu A, Stoia M, Farcas A, et al. Arterial stenosis and atherothrombotic events in polycythemia vera and essential thrombocythemia. Rom J Intern Med. 2006; 44:397–406. PMID: 18386616.
10. Hasselbalch HC. Perspectives on chronic inflammation in essential thrombocythemia, polycythemia vera, and myelofibrosis: is chronic inflammation a trigger and driver of clonal evolution and development of accelerated atherosclerosis and second cancer? Blood. 2012; 119:3219–3225. PMID: 22318201.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download