Abstract
Objectives
Full thickness skin grafts (FTSG) offer several advantages; they are esthetically superb, have less postoperative shrinkage, and offer minimal postoperative pain and scar formation at the donor site. As a donor site of FTSG, the groin offers a relatively large area of skin with high elasticity. The aim of this study was to evaluate FTSG from the groin for reconstruction in oral and maxillofacial surgery.
Materials and Methods
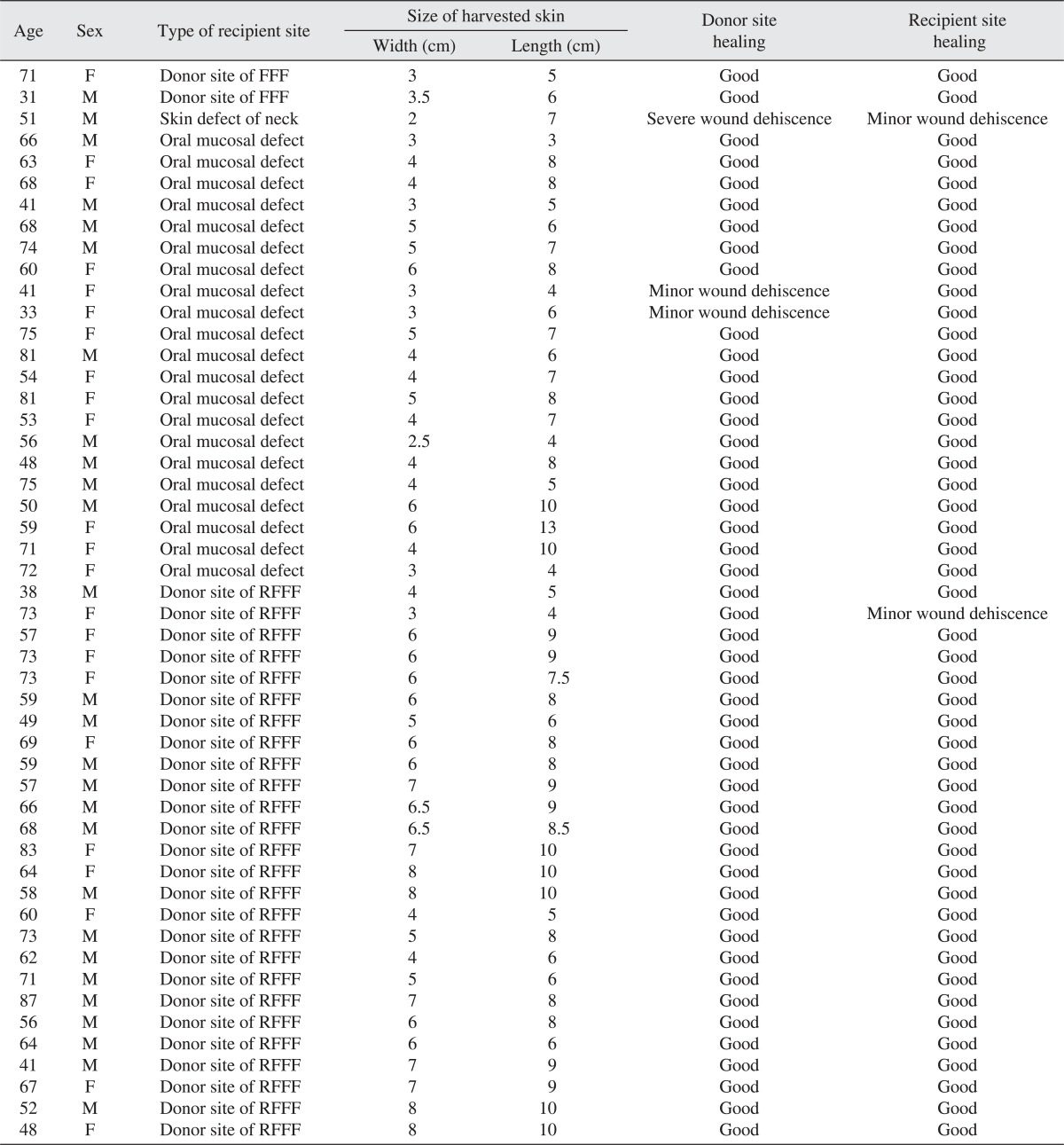
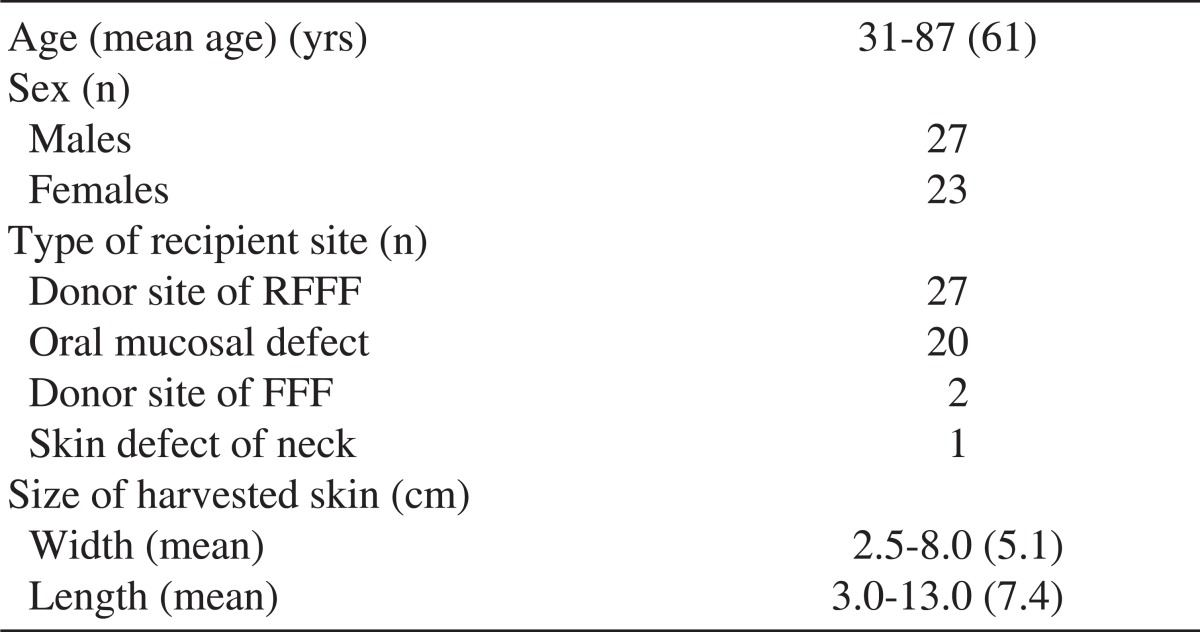
In a retrospective study, 50 patients (27 males, 23 females) who received FTSG from the groin were evaluated for their operation records, clinical photography, and medical records.
Results
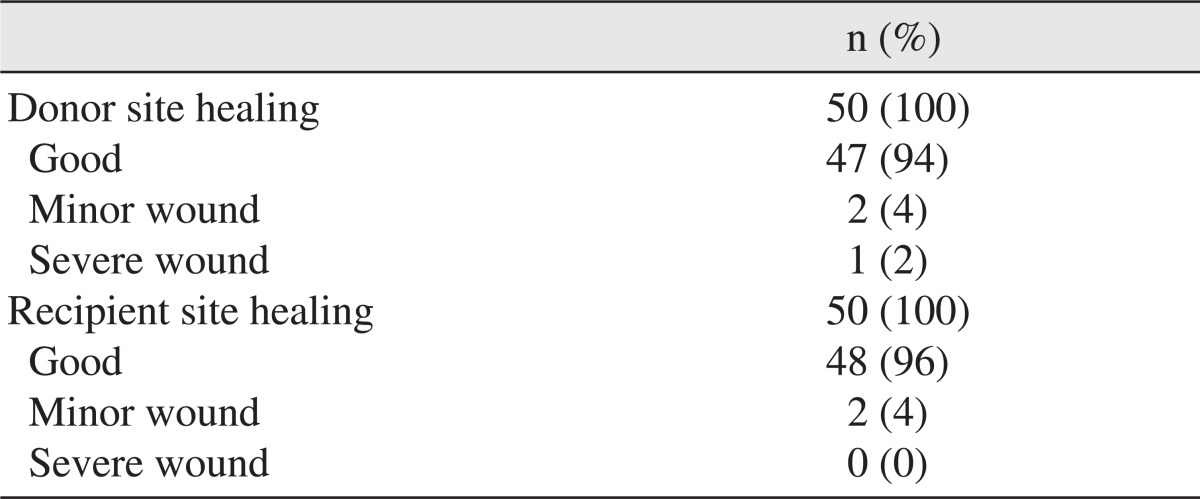
The width of skin from the groin was distributed from 2-8 cm (mean: 5.1 cm) at the donor site, while the long axis length was distributed from 3-13 cm (mean: 7.4 cm). A high number of patients, 47 patients (94%) out of 50, showed good healing at the donor site. Wound impairment was seen in 3 patients (6%), minor wound dehiscence in 2 patients, and severe wound dehiscence in 1 patient. In the recipient site, delayed healing was observed in 2 patients (4%).
Skin grafts are widely used in the field of oral and maxillofacial surgery, from repairing intraoral mucosal defects to coverage of the radial forearm free flap (RFFF) donor sites. Split thickness skin grafts (STSG) generally have higher survival rate, and they are easier to harvest compared to full thickness skin grafts (FTSG). Note, however, that the use of STSG has functional and esthetic complications including esthetically undesirable appearance, severe pain and discomfort in the early postoperative period, delayed wound healing and scar, and pigmentation formation. FTSG can ensure favorable appearance with less shrinkage compared to STSG and less postoperative pain and discomfort of the donor site; on the other hand, the survival rate is lower than STSG, with FTSG having a limitation in terms of skin size; hence the possible difficulty in repairing huge defects. As a donor site of FTSG, the groin offers the advantages of being able to harvest relatively larger amounts of skin compared to other parts of the body, with the scar marked by inguinal crease. Likewise, by using the method suggested by Taifour Suliman1, faster healing process could be expected. The authors studied retrospectively 50 cases of FTSG from the groin for reconstruction in the field of oral and maxillofacial surgery and achieved favorable outcome.
From November 2008 to February 2011, 50 patients (27 males, 23 females) who received FTSG from the groin participated in a retrospective study using their operation record, clinical photography, and medical record. Patients' mean age was 61 (youngest: 31 years old; oldest: 87 years old). Surgery was performed under general anesthesia, and we harvested fusiform skin using the inguinal crease of the groin as the long axis.(Fig. 1. A) For skin harvesting, we used the methods suggested by Taifour Suliman1 and made an incision with a 45° angle inside along a boundary of the constructed skin graft and harvested by slicing it. As such, we minimized bleeding and exposure of underlying fat tissues.(Fig. 1. B) After skin harvesting, we controlled hemorrhage using electrocautery; without undermining, the margin areas of the skin consisting of two lines of fusiform were neighbored and sutured layer by layer.(Fig. 1. C) Ten days after surgery, we performed stitch-out of the donor site. We studied the medical record of the donor site as well as the recipient site.
Table 1 and Table 2 show the distribution of the recipient sites of skin grafts. The width of skin was distributed from 2 cm to 8 cm (mean: 5.1 cm); the long axis length of the groin was distributed from 3 cm to 13 cm (mean: 7.4 cm). Among 50 patients, impaired healing of the donor site wound was observed on 3 patients (6%). Two patients (4%) were found to have minor wound dehiscence, with 1 patient (2%) observed to have severe wound impairment that exposed the downward fat tissues because of necrosis on some parts of the skin; they were all healed in 2 months. The remaining 47 patients (94%) exhibited favorable healing condition. As to the healing condition of the recipient site, delayed healing was noted on 2 patients (4%) (skin defect of neck: 1 patient; donor site of RFFF: 1 patient), but both were healed in 2 months.(Table 3)
In the field of oral and maxillofacial surgery, skin grafting is required in the following cases; covering the defect of the vascularized free flap donor site, repairing the exposed raw surface after intraoral mass excision, and covering the defect after the mass excision of the head and neck area or trauma. Whether to use FTSG or STSG is decided based on the size of the skin, available donor site, vascularity of the recipient site, and esthetic considerations. For the coverage of the RFFF donor site, STSG from the thigh is generally used; satisfactory results have been reported regarding the function of the forearm, healing period, and esthetic aspects. The donor site defect of RFFF is preferentially covered by STSG because it can easily be harvested in rectangular form using a dermatome. Moreover, STSG is preferentially used in cases of oral mucosal defects where the mobility of the underlying soft tissue would decrease the survival rate of FTSG. Note, however, that the donor site of STSG has a long healing period and the disadvantages of postoperative pain, scar formation, and esthetic problems2. Likewise, STSG requires much more effort in terms of postoperative care of the donor site3. FTSG offers the advantages of superb esthetics4, less postoperative shrinkage, and minimal postoperative pain and scar formation through primary closure compared to STSG5,6. Nonetheless, the size of FTSG is relatively limited, and there is a possibility of graft failure due to the thickness of the graft7.
The groin offers relatively larger size of skin due to surplus skin with high elasticity. After skin harvesting, the defect could primarily be closed, and the scar could be hidden by the natural crease8. Kim et al.6 performed FTSG from the groin for coverage of RFFF in 40 patients and reported no postoperative pain or limitation of movement on the groin and 2 cases of tendon exposure on the forearm. The authors implemented FTSG but chose the groin as donor site, which has extra skin; thus gaining relatively big graft and using it on the RFFF donor site or oral mucosal defect. Moreover, they minimized the thickness of the graft using Suliman's method to increase the survival rate of graft. Taifour Suliman1 introduced a simple method of harvesting skin by making an incision with a 45° angle and detaching the skin by slicing it to gain relatively thin skin, which would reduce fat exposure with no bleeding.
At least 47 patients (94%) out of 50 exhibited good healing process of the donor site.(Fig. 1. D) Wound impairment was noted on 3 patients (6%), minor wound dehiscence, on 2 patients, and severe wound dehiscence, on 1 patient. Minor wound dehiscence (2 cases) seemed to have no correlation with the size of the graft since the latter was relatively small (width of 3.0 cm, length of 4.0 cm; width of 3.0 cm, length of 6.0 cm each). On the other hand, because the patients were young (one is a 33-year-old woman, the other a 41-year-old woman), we think there was a lot of tension between two margins of skin. One case of severe wound dehiscence (51-year-old man) was observed on the graft measuring 2.0×7.0 cm, with partial necrosis of the skin margin and exposed underneath fat tissue noted. In this case, the width of harvested skin was relatively small. Thus, we think the size of skin was not the cause of wound dehiscence. On the other hand, the patient has many other wound dehiscences on his body such as neck wound (recipient site of skin graft), chest wound formed due to the raising of pectoralis major myocutaneous flap, and intraoral wound that developed due to tumor resection and reconstruction. As such, we concluded that, even though he has no systemic disease, he has a systemic problem with the wound healing process.
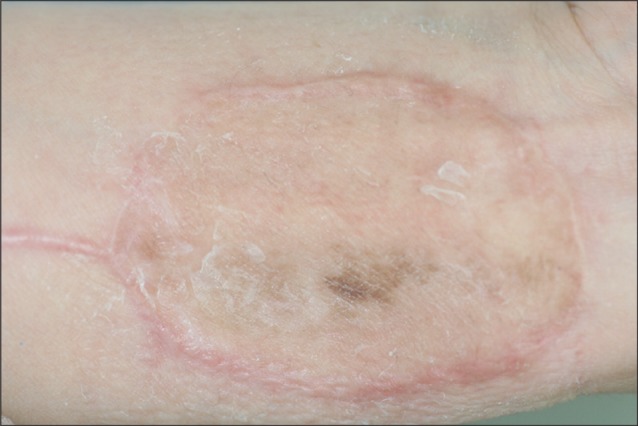
A total of 48 patients (96%) succeeded in grafting, with good healing process of the recipient site (Figs. 2, 3), with 2 patients (4%) exhibiting graft failure and impaired wound healing. One patient showed partial exposure of the tendon on the RFFF defect site, whereas the other manifested grafting failure on skin defect of neck; the latter was the same patient who showed severe wound impairment of the groin. For this patient, the general condition probably influenced wound healing.
For wound closure, we pulled both sides of the wound edges without undermining the tissue underneath and performed primary closure. The reason for not carrying out undermining - which reduces tension of tissue - is that, since groin has surplus skin, wound margins can be easily brought together without undermining. In addition, the textbook meaning of undermining suggests the implementation of wound closure by doing dissection on the skin and fat layer in the plane of the upper muscle under no tension. Undermining involves dissecting the skin and fat layer to reduce tension during wound closure. In the groin, however, undermining may damage the superficial epigastric vessels and superficial circumflex iliac vessels lying above the inguinal ligament. Moreover, this takes much time and has the weakness of causing profuse bleeding because of the thick fat layer, which may cause excessive bleeding during undermining. In the clinic, we attempted wound closure after undermining the fat layer right underneath the skin but encountered skin necrosis due to the lack of blood supply on the skin margins. Therefore, we performed wound closure without undermining for the 50 cases. Inguinal crease had harvested mean width of 5.1 cm and actually yielded good results in the biggest width of 8.0 cm. The harvested skin was measured to have mean width of 5.1 cm and maximum width of 8.0 cm.
Taifour Suliman's method of skin harvesting is controversial. In this method, deep dermis is not entirely included in the graft, possibly leaving a dermal layer on the donor site; this in turn can lead to the formation of epidermal inclusion cyst. Still, Taifour Suliman1 insisted that the layer left after skin harvest is part of superficial fascia, not deep dermis; hence the extremely low possibility of inclusion cyst formation, Taifour Suliman also mentioned that none of the above occurred in the reported cases. In our 50 cases, the occurrence of epidermal inclusion cyst was not observed.
There are limitations with FTSG as well. Since the groin is hair-bearing tissue, undesirable hair growth may occur on the recipient sites. Furthermore, skin from the groin has a tendency of dark pigmentation8. The inner surface of the upper arm may be considered an alternative donor site with esthetically good skin, but harvesting a large size of skin is difficult. The lower abdomen is another alternative; although large skin harvest is possible, however, it does not match the skin of the head and neck region. To do away with the need for an additional donor site for grafting, primary closure may be considered in small radial defects9. In medium-sized radial defects, Ular flap10, Z-plasty11, or modified Z-plasty of combined Ular flap and Z-plasty12 were introduced. Note, however, that local flap requires wide dissection underneath the local flap. In larger radial defects, grafting full thickness skin from the proximal side of the defect area was introduced by using the concept of autonomous reparative unit, which allows accurate and efficient design of the graft13. Split thickness skin of the radial flap may also be harvested prior to radial flap raising14. Split thickness skin was harvested in mesh form from 66 patients, with its size stretched or grafted with non-mesh form. Because of the uneven surface of the forearm, they posed a difficulty to site dermatome; hence the failed harvesting skin graft from one old man.
We think FTSG from the groin for soft tissue defect repair in reconstruction surgery is a good method considering the relatively big graft obtained, lower morbidity of the donor site, and higher graft survival rate. Nonetheless, we think the size of the skin graft should not be big when applied to younger patients since wound dehiscences could develop. After surgery, all patients had no problem walking, but they were not able to wear triangle briefs since such may lead to wound impairment. We believe our results using FTSG from the groin for reconstructive surgery demonstrate that this is a favorable technique for both donor and recipient sites.
References
1. Taifour Suliman M. A simple method to facilitate full-thickness skin graft harvest. Burns. 2009; 35:87–88. PMID: 18703286.

2. Avery CM. Review of the radial free flap: is it still evolving, or is it facing extinction? Part one: soft-tissue radial flap. Br J Oral Maxillofac Surg. 2010; 48:245–252. PMID: 19837491.

3. Sidebottom AJ, Stevens L, Moore M, Magennis P, Devine JC, Brown JS, et al. Repair of the radial free flap donor site with full or partial thickness skin grafts. A prospective randomised controlled trial. Int J Oral Maxillofac Surg. 2000; 29:194–197. PMID: 10970081.

4. Lutz BS, Wei FC, Chang SC, Yang KH, Chen IH. Donor site morbidity after suprafascial elevation of the radial forearm flap: a prospective study in 95 consecutive cases. Plast Reconstr Surg. 1999; 103:132–137. PMID: 9915173.

5. Avery CM, Iqbal M, Orr R, Hayter JP. Repair of radial free flap donor site by full-thickness skin graft from inner arm. Br J Oral Maxillofac Surg. 2005; 43:161–165. PMID: 15749218.

6. Kim TB, Moe KS, Eisele DW, Orloff LA, Wang SJ. Full-thickness skin graft from the groin for coverage of the radial forearm free flap donor site. Am J Otolaryngol. 2007; 28:325–329. PMID: 17826534.

9. Shiba K, Iida Y, Numata T. Ipsilateral full-thickness forearm skin graft for covering the radial forearm flap donor site. Laryngoscope. 2003; 113:1043–1046. PMID: 12782819.

10. Juretic M, Car M, Zambelli M. The radial forearm free flap: our experience in solving donor site problems. J Craniomaxillofac Surg. 1992; 20:184–186. PMID: 1629369.

11. Hui KC, Zhang F, Lineaweaver WC. Z-plasty closure of the donor defect of the radial forearm free flap. J Reconstr Microsurg. 1999; 15:19–21. PMID: 10025526.

12. Bashir MA, Fung V, Kernohan MD, Ragbir M, Ahmed OA. "Z-plasty" modification of ulnar-based fasciocutaneous flap for closure of the radial forearm flap donor defect. Ann Plast Surg. 2010; 64:22–23. PMID: 20023451.

13. Squadrelli-Saraceno M, Compan A, Bimbi G, Gatto L, Riccio S, Colombo S. Autonomous reparative unit (ARU): a new concept of repairing free flap donor site with local full-thickness skin graft. Acta Otorhinolaryngol Ital. 2010; 30:40–46. PMID: 20559472.
14. Ghanem TA, Wax MK. A novel split-thickness skin graft donor site: the radial skin paddle. Otolaryngol Head Neck Surg. 2009; 141:390–394. PMID: 19716019.
Fig. 1
A. Construction for skin harvesting on groin, using inguinal crease as the long axis. B. Harvesting thin skin without exposing the underlying fat tissue. C. Neighboring and layer-by-layer suturing of wound margins without undermining. D. Healing status of the donor site 1 month after the surgery.
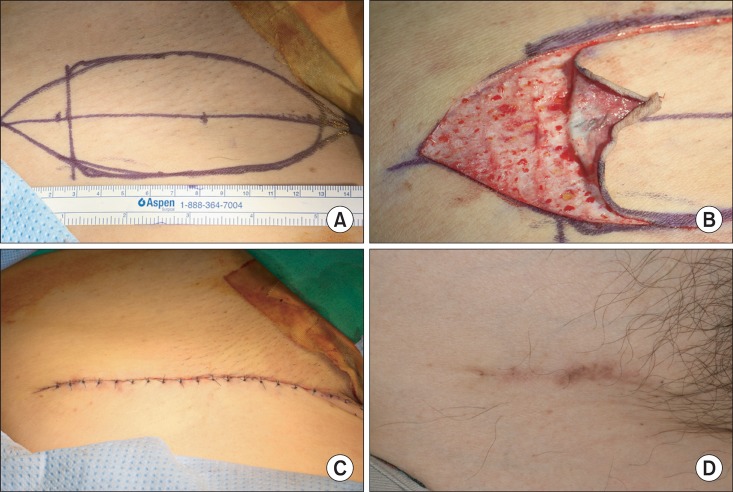
Fig. 2
A. Healing status of the recipient site (oral mucosal defect) 10 days after the surgery. B. Healing status of the recipient site (oral mucosal defect) 2 months after the surgery.
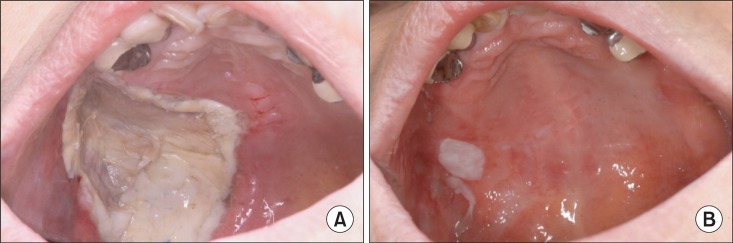
Fig. 3
Healing status of the recipient site (donor site of radial forearm free flap) 4 months after the surgery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download