Abstract
With successful extraction of growth factors and bone morphogenic proteins (BMPs) from mammalian teeth, many researchers have supported development of a bone substitute using tooth-derived substances. Some studies have also expanded the potential use of teeth as a carrier for growth factors and stem cells. A broad overview of the published findings with regard to tooth-derived regenerative tissue engineering technique is outlined. Considering more than 100 published papers, our team has developed the protocols and techniques for processing of bone graft material using extracted teeth. Based on current studies and studies that will be needed in the future, we can anticipate development of scaffolds, homogenous and xenogenous tooth bone grafts, and dental restorative materials using extracted teeth.
Tooth is a composite structure consisting of inorganic components including the calcium phosphate lineage and organic components such as collagen. Tooth minerals consist of five biological calcium phosphates: hydroxyapatite, tricalcium phosphate (TCP), octacalcium phosphate (OCP), amorphous calcium phosphate (ACP), and dicalcium phosphate dehydrate. Interacting reciprocally, these calcium phosphates are capable of remodeling the existing bone when grafted. The apatite existing within the bone tissue is known to be in the form of ceramics/high-polymer nano-composites.
Teeth and bones share many similarities. Teeth, cartilages, nerves, and maxillofacial bones all embryologically originated in the neural crest, sharing identical origin1-4. Clinicians support the intramembranous bone formation pathway when intraoral bone grafting is achieved5,6. The chemical compositions of teeth, especially dentin and bones, are very similar. Enamel consists of 96% inorganic substances and 4% water, whereas dentin has 65% inorganic substances, 35% organic substances, and water. Cementum is made up of 45-50% inorganic substances, 50-55% organic substances, and water. Finally, alveolar bone has 65% inorganic and 35% organic substances.
In organic parts, dentin and cementum include type I collagens and various growth factors such as bone morphogenic proteins (BMPs). Type I collagen occupies about 90% of the organic parts of tissues, with the rest non-collagenous proteins (NCP), biopolymers, lipid, citrate, lactate, etc. NCPs include phosphophoryn, sialoprotein, glycoprotein, proteoglycan, osteopontin (OPN), osteocalcin, dentin matrix protein-1, osterix, and Cbfa1 (Runx2). These proteins are known to trigger the bone resorption and generation processes7-15.
Based on the potentials of osteoconduction, osteoinduction, and osteogenesis through growth factors in tooth and similar histogenesis between tooth and bone, a novel bone graft material can be developed utilizing the inorganic and organic components of an extracted tooth. Indeed, autogenous tooth bone graft material (AutoBT; Korea Tooth Bank Co., Seoul, Korea) has been developed from an extracted tooth. A non-restorable tooth or a third molar tooth is assigned to be extracted from the patient. With fabrication and demineralization process, AutoBT material is made from the extracted tooth. This AutoBT is grafted back to the same patient when guided bone regeneration is necessary in dental surgeries. Currently, AutoBT is widely used in clinics in Korea and Japan.
This review paper provides overviews of the chemical compositions of dentin due to its similarities to those of alveolar bone and previous studies on demineralized dentin matrix (DDM), an initial tooth-derived tissue engineering application. Finally, we summarized recent applications of tooth as bone grafting material.
Dentin consists of 70% hydroxyapatite in its weight volume. Hydroxyapatite in dentin is structured with low-crystalline calcium phosphate16, making future bone remodeling possible. Bone tissues are also mainly composed of low-crystalline apatite. In contrast, hydroxyapatite in enamel is structured as high-crystalline calcium phosphate. High crystalline contents are not easily decomposed by osteoclasts, resulting in slow resorption and consequently poor osteoconductivity17.
Growth factors are signaling proteins that regulate cellular growth, proliferation, and differentiation18. Urist19 initially discovered BMPs and studied their roles in 1965. BMPs are known to exist in the bone matrix, osteosarcoma tissue, and dentin matrix, functioning to differentiate perivascular mesenchymal stem cells into cartilage and bone tissues20-23. Several studies have successfully isolated BMPs from dentin, enamel, and cementum of bovine, rats, guinea pigs, and rabbit teeth8,22-25. With extensive studies on BMPs, researchers have confirmed the osteoinductivity of BMPs extracted from animal teeth such as bovine, lapine, and murine teeth8-10,22,23,26-30.
Since only a limited amount of BMPs can be extracted from the teeth, however, the clinical utilization may be limited31-33. Therefore, various recombinant human BMPs (rhBMP) have been recently manufactured by gene recombination based on mammal cells or colon bacilli34-36.
Dentin and cementum contain various other growth factors besides BMPs such as insulin-like growth factor (IGF), platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), and transforming growth factor (TGF)-β37,38. Finkelman et al.39 reported the extraction of TGF-β, IGF-I, IGF-II from human dentin but at lower levels compared to those from human bone.
About 90% of dentinal organic components are known to be type I collagens. These triple-helix structured collagens are the most abundant protein in vertebrates. Collagen-derived materials have demonstrated biocompatibility and interference in bone formation at the implanted sites40-42.
The rest of dentinal organic components are NCP. NCPs that contribute to mineralization are osteocalcin, osteonectin, phosphophoryn, dentin sialoprotein (DSP), dentin-specific extracellular matrix protein, etc. Phosphophoryn in particular, bound to type I collagen, contributes to the mineralization process; it is of the largest amounts among NCPs. Previous studies discovered through the immune-histochemical study that OPN and DSP manifested 6-8 weeks after grafting the tooth graft material on alveolar bone defects in Wistar rats43. OPN is known to trigger osteogenesis through the early differentiation of the osteoblasts but also leads to bone resorption by allowing adherence of osteoclasts to the bone surface. DSP has a significant role in dentin calcification12,44.
Traditionally, roots were intentionally left for the prevention of alveolar bone resorption in removable prosthodontics or in cases of tooth extractions45,46. Intentional partial odontectomy has been safely practiced when roots of impacted third molar are situated close to the inferior alveolar nerve or ankylosed since only a crown portion is dissected, leaving the roots behind47. The root remnant of non-pathology involved tooth in alveolar bone does not induce any inflammatory response. Osteoclast cells appear in the pulp cavity, with the pulp replaced by bone, followed by root resorption. After all, the remaining roots completely fuse with the surrounding alveolar bone. Based on these clinical reports, alveolar bone and teeth can be inferred to have high level of affinity to each other48-50.
Homogenous demineralized dentin matrix (HDDM) is as an effective biocompatible bone graft material as autogenous demineralized dentin matrix (ADDM) since it induces heterotopic bone formation with no host immune rejection51,52. The demineralization process of HDDM does not denature osteopromotive properties. HDDM is a reservoir of biochemical factors that induce cellular proliferation as well as cell differentiation and chemotaxis53,54. In the histomorphometric analysis of HDDM in vitro, HDDM resorbs itself during the bone remodeling process53. Gomes et al.54 further evaluated the bone repair process after implantation of HDDM slices in surgical defects created in the parietal bones of rabbits with alloxan-induced diabetes. They reported that HDDM was biocompatible, stimulating bone tissue formation. In this study, HDDM is well accepted by the host and is totally incorporated into newly formed bone tissue.
Highly soluble, BMPs do not exert osteoinductive effects when used alone. Scaffolds are used to force BMPs to stay at the implant site55-57. Scaffold functions as carrier. An ideal scaffold should control-release growth factors or cells and can prevent degradation and inactivation18. Different materials are used for different purposes. Collagen and TCP are clinically used most widely58. For the delivery of BMPs and growth factors, collagen, calcium phosphates, and polyesters such as polycaprolactone have been used59-61.
DDM was introduced as an alternative material for scaffold in releasing BMPs62-64. Ike and Urist62 suggested that root dentin prepared from extracted teeth could be recycled for use as carrier of rhBMP-2. Although the quantity of endogenous BMP in dysfunctional teeth is very small or nil, active new bone formation was observed by many scientists when DDM was used as carrier62,64. According to the biochemical and histomorphometric analyses of bone and cartilage induced by human DDM and BMP-2, researchers concluded that human DDM of vital teeth origin induced bone and cartilage, and that BMP-2 strongly accelerated bone formation in the DDM carrier system65.
The demineralization process is required for freeing the various growth factors and proteins, since the release of the growth factors is sometimes blocked by the presence of hydroxyapatite crystals. Many authors observed that heterotrophic bone was induced when DDM was grafted in the lapine, porcine, and murine muscle tissues. As such, decalcification of dentin is believed to induce the release of BMP, thereby leading to osteoinduction52,66-70. Researchers use various decalcification methods. Decalcified dentin and bone using 0.6N HCl lead to the inducement of connective tissue cells and formation of endochondral bone in muscle and in skin connective tissues19,66,71-75. Ike and Urist62 partially demineralized the roots of the teeth using 0.6N HCL for 24 hours, and then cut them in 0.5 g blocks to produce partially demineralized matrix (PDM). PDM was then washed in cold water and lyophilized. An alternative approach was employed by Inoue et al.67; they grafted the demineralized dentin tissues using 0.6N HCL (pH1) and 3M (9N) in the rectal abdominis muscles of Wistar rats. Inoue et al.67 reported favorable chondrogenesis and osteogenesis, with the HCL-demineralized dentin showing relatively superior results. Different approaches in acid treatment protocols were used. DDM was treated using 2% HNO3. Several animal studies showed favorable results, with observed new bone formation68,76.
Some studies showed contrary results. According to Ike and Urist62, when human partially demineralized dentin granules were grafted in the intramuscular pockets, osteoinduction was not observed. Based on the quantitative analysis of proliferation and differentiation of the MG-63 cell, however, cellular adhesion and proliferation activity of the MG-63 cell on partially demineralized dentin matrix were noted77. With differently employed methods, one may conjecture that the osteoinductive properties of dentin may depend on different acid treatment protocols.
Bone substitutes have been actively used in clinics to reconstruct bony defects. There are four categories of bone graft materials: autograft, allograft, alloplast, and xenograft. With four types of graft materials available, the use of these materials depends on clinical applications, volume of deficiency, and evidence-based studies52,78,79. Above all, autografts are known to be the gold standard due to its osteoinductivity, osteoconductivity, and osteogenicity. Still, autogenous bone grafts harvested from extra-oral sites have some limitations, such as high morbidity, potential resorption, and high costs78,80. With advancements in tissue engineering, researchers have extensively studied compensating the drawbacks of autografts. Thus, many researchers paid attention to human tooth as one of the intraoral donor sites due to its chemical similarities to bone.
Extensive studies in vitro have been conducted on ADDM with its biocompatibility, osteoinductivity, and osteo conductivity81-84. In animal studies, ADDM induced bone formation according to the histology analysis81-83. For instance, Gomes et al.54 performed a histological evaluation of the osteoinductive property of ADDM on calvarial bone defects in rabbit. According to the study, ADDM was verified to have chemotactic properties for osteoprogenitor cells and osteoblasts, promoting the acceleration of bone repair process at the bony defect. Slices of ADDM induced direct bone formation, and they were incorporated by the newly formed bone tissue and remodeled82.
The mechanisms involved in the osteogenesis of ADDM include endochondral and intramembranous bone formation52,85-87. Likewise, the osteogenesis of ADDM is influenced by the size and form of graft materials87. The ideal sizes of graft material granules are different from author to author, ranging from 75 µm to 500 µm73,88,89. Some authors reduced the inter-particulate distances by adding β-TCP due to difficulties in homogenizing the sizes40. Since ADDM contains native growth factors supporting mesenchymal cell attachment and further absorbs several proteins derived from body fluid, however, some authors state that homogenizing the ADDM granule size is not critical65,90.
The clinical effectiveness of ADDM was tested in pocket preservation. Wistar rat's incisors were frozen soon after extraction, and then milled with hydroxypropyl cellulose added. Consequently, early healing and bone formation in the extraction socket were observed when grafted with milled tooth. This study used the extracted tooth as a whole without decalcification, including both enamel and dental pulp. Therefore, the results indicate that osteoinductive healing may come from growth factors in dentin or dental pulp91. Another study was conducted on the human third molar socket wherein the greater homogeneity of bone radiopacity with enhanced healing process was observed53,81,84. Periods of radiographic observation focusing on the changes in radiopacity and in the peripheral boundary between graft material and bone and clinical observations confirmed that the graft was biocompatible and clinically easy to use92. Another application of ADDM is on implant dentistry. In fact, ADDMs have been actively tested in implant osseointegration and bone remodeling capacity; thus enhancing implant primary stability86.
Based on decades of research and scientific facts on tooth, Jeong et al.80 and Kim et al.93 suggested that AutoBT is an excellent alternative to autogenous bone graft. After all, AutoBT was developed and has been in clinical use since 2008 in Korea. With the patient's consent, the extracted teeth are sent to Korea Tooth Bank in 75% ethyl alcohol storage container.(Fig. 1. A) After dissection of the anatomical crown, sample root portions are ground into powder form, with each particle measuring 400-800 µm in diameter.(Fig. 1) The remaining soft tissues and contaminants of the particulate AutoBT are removed with distilled water. Once subjected to dehydration, defatting, lyophilization, and ethylene oxide sterilization processes, AutoBT is packed. A block form of AutoBT is fabricated in the same manner as particulate bone graft excluding the grinding steps.(Fig. 1. C)
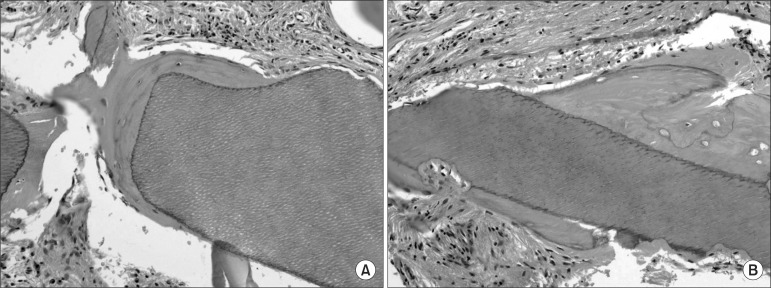
The basic components and surface structure of AutoBT have been analyzed using X-ray diffraction analyzer, scanning electron microcopy, and histomorphometric evaluation16,78. AutoBT consists of low-crystalline hydroxya-patite and other calcium phosphate minerals such as TCP, ACP, and OCP, which are components similar to those of human bone16. With the analysis of AutoBT's basic components, diverse clinical applications of using AutoBT have been identified, supporting the osteoinductive and osteoconductive capabilities of AutoBT with favorable clinical results79,94-103. In clinical studies, AutoBT has been grafted in sinus bone graft (Fig. 2. A-2. C), guided bone regeneration, ridge augmentation, ridge splitting, and socket preservation94-103.(Fig. 3. A-3. E) Later, researchers histologically noticed that AutoBT underwent gradual resorption, and that it was replaced by new bone16,78.(Fig. 4. A-4. B) AutoBT can also be mixed with other types of bone graft materials when repairing large defects104. Furthermore, the block form of AutoBT is an excellent choice as material when reconstructing large bony defects with or without the combination of AutoBT powder types102. The block form of AutoBT is fabricated with the same procedures as the powder type except crushing the teeth. Thus, the AutoBT block form still includes the remaining root structure of the extracted tooth.
With support from the previous studies on AutoBT, it was confirmed that AutoBT is a safe and effective bone graft material. AutoBT was further suggested to have potential to be developed into allogenic and xenogenic tooth bone graft materials, ideal scaffold for stem cells and bone growth factors, and endodontic and tooth restorative material.
Indeed, DDM has shown potential applications in bone substitute and scaffold. As discussed in this review, ADDM, with absence of antigenicity, enhances bone-remodeling capabilities. Among a variety of available bone graft materials, choosing the appropriate one is challenging. While choosing the graft material should be dictated by the extent of defects and the procedural purposes, tooth-derived bone graft may be considered as an option given its autogenous origin and favorable clinical and histological outcomes when teeth extraction is necessary. Further studies are needed in evaluating clinical efficacies and comparing other commercially available bone graft materials.
References
1. Yoshida T, Vivatbutsiri P, Morriss-Kay G, Saga Y, Iseki S. Cell lineage in mammalian craniofacial mesenchyme. Mech Dev. 2008; 125:797–808. PMID: 18617001.

2. Morrison SJ, White PM, Zock C, Anderson DJ. Prospective identification, isolation by flow cytometry, and in vivo self-renewal of multipotent mammalian neural crest stem cells. Cell. 1999; 96:737–749. PMID: 10089888.

3. Stevens A, Zuliani T, Olejnik C, LeRoy H, Obriot H, Kerr-Conte J, et al. Human dental pulp stem cells differentiate into neural crest-derived melanocytes and have label-retaining and sphere-forming abilities. Stem Cells Dev. 2008; 17:1175–1184. PMID: 18393638.

4. Arthur A, Rychkov G, Shi S, Koblar SA, Gronthos S. Adult human dental pulp stem cells differentiate toward functionally active neurons under appropriate environmental cues. Stem Cells. 2008; 26:1787–1795. PMID: 18499892.

5. Reddi AH. Bone matrix in the solid state: geometric influence on differentiation of fibroblasts. Adv Biol Med Phys. 1974; 15:1–18. PMID: 4600893.

6. Huggins C, Wiseman S, Reddi AH. Transformation of fibroblasts by allogeneic and xenogeneic transplants of demineralized tooth and bone. J Exp Med. 1970; 132:1250–1258. PMID: 4929179.

8. Kawai T, Urist MR. Bovine tooth-derived bone morphogenetic protein. J Dent Res. 1989; 68:1069–1074. PMID: 2808865.

9. Bessho K, Tagawa T, Murata M. Purification of rabbit bone morphogenetic protein derived from bone, dentin, and wound tissue after tooth extraction. J Oral Maxillofac Surg. 1990; 48:162–169. PMID: 2299457.

10. Bessho K, Tagawa T, Murata M. Comparison of bone matrix-derived bone morphogenetic proteins from various animals. J Oral Maxillofac Surg. 1992; 50:496–501. PMID: 1573485.

11. Feng JQ, Luan X, Wallace J, Jing D, Ohshima T, Kulkarni AB, et al. Genomic organization, chromosomal mapping, and promoter analysis of the mouse dentin sialophosphoprotein (Dspp) gene, which codes for both dentin sialoprotein and dentin phosphoprotein. J Biol Chem. 1998; 273:9457–9464. PMID: 9545272.

12. Ritchie HH, Ritchie DG, Wang LH. Six decades of dentinogenesis research. Historical and prospective views on phosphophoryn and dentin sialoprotein. Eur J Oral Sci. 1998; 106(Suppl 1):211–220. PMID: 9541228.
13. Hoeppner LH, Secreto F, Jensen ED, Li X, Kahler RA, Westendorf JJ. Runx2 and bone morphogenic protein 2 regulate the expression of an alternative Lef1 transcript during osteoblast maturation. J Cell Physiol. 2009; 221:480–489. PMID: 19650108.

14. Handschin AE, Egermann M, Trentz O, Wanner GA, Kock HJ, Zünd G, et al. Cbfa-1 (Runx-2) and osteocalcin expression by human osteoblasts in heparin osteoporosis in vitro. Clin Appl Thromb Hemost. 2006; 12:465–472. PMID: 17000892.

15. Ye L, MacDougall M, Zhang S, Xie Y, Zhang J, Li Z, et al. Deletion of dentin matrix protein-1 leads to a partial failure of maturation of predentin into dentin, hypomineralization, and expanded cavities of pulp and root canal during postnatal tooth development. J Biol Chem. 2004; 279:19141–19148. PMID: 14966118.

16. Kim YK, Kim SG, Oh JS, Jin SC, Son JS, Kim SY, et al. Analysis of the inorganic component of autogenous tooth bone graft material. J Nanosci Nanotechnol. 2011; 11:7442–7445. PMID: 22103215.

17. Kim GW, Yeo IS, Kim SG, Um IW, Kim YK. Analysis of crystalline structure of autogenous tooth bone graft material: X-Ray diffraction analysis. J Korean Assoc Oral Maxillofac Surg. 2011; 37:225–228.

18. Karfeld-Sulzer LS, Weber FE. Biomaterial development for oral and maxillofacial bone regeneration. J Korean Assoc Oral Maxillofac Surg. 2012; 38:264–270.

20. Hanamura H, Higuchi Y, Nakagawa M, Iwata H, Nogami H, Urist MR. Solubilized bone morphogenetic protein (BMP) from mouse osteosarcoma and rat demineralized bone matrix. Clin Orthop Relat Res. 1980; (148):281–290. PMID: 6929747.

21. Sampath TK, Reddi AH. Homology of bone-inductive proteins from human, monkey, bovine, and rat extracellular matrix. Proc Natl Acad Sci U S A. 1983; 80:6591–6595. PMID: 6579546.

22. Butler WT, Mikulski A, Urist MR, Bridges G, Uyeno S. Noncollagenous proteins of a rat dentin matrix possessing bone morphogenetic activity. J Dent Res. 1977; 56:228–232. PMID: 265954.

23. Conover MA, Urist MR. Dentin matrix morphogenetic protein. The chemistry and biology of mineralized connective tissues: Proceedings of the First International Conference on the Chemistry and Biology of Mineralized Connective Tissues. 1981. 3-7 May 1981; Northwestern University Dental School, Chicago, IL, USA. New York: Elsevier-North Holland Inc;p. 597–606.
24. PH Chung. Method for extracting tooth protein from extracted tooth. Korea Intellectual Property Rights Information Service. Patent. Application No. 10-2002-0008789.
25. PH Chung. Tooth protein extracted from extracted tooth and method for using the same. Korea intellectual property rights information service. Patent. Application No. 10-2004-0 051812.
26. Chiba M. Experimental studies of bone morphogenetic protein derived from bovine tooth. Jpn J Oral Maxillofac Surg. 1988; 34:1557–1566.

27. Urist MR, Mizutani H, Conover MA, Lietze A, Finerman GA. Dentin, bone, and osteosarcoma tissue bone morphogenetic proteins. Prog Clin Biol Res. 1982; 101:61–81. PMID: 6760205.
28. Bessho K, Tagawa T, Murata M. Analysis of bone morphogenetic protein (BMP) derived from human and bovine bone matrix. Clin Orthop Relat Res. 1991; (268):226–234. PMID: 2060214.
29. Bessho K, Tanaka N, Matsumoto J, Tagawa T, Murata M. Human dentin-matrix-derived bone morphogenetic protein. J Dent Res. 1991; 70:171–175. PMID: 1999554.

30. Ito K, Arakawa T, Murata M, Tazaki J, Takuma T, Arisue M. Analysis of bone morphogenetic protein in human dental pulp tissues. Arch Bioceramics Res. 2008; 8:166–169.
31. Chae YP, Lee JH, Kim SK, Yeo HH. A histologic study on the repair of rat calvarial critical size defect with bovine bone morphogenetic protein (b-BMP). J Korean Assoc Oral Maxillofac Surg. 1997; 23:290–303.
32. Kim BR, Lee JH, Kim JW. Comparison of bone inducing process of porcine bone matrix-derived bmp combined with the following, freeze-dried allogeneic bone, surface demineralized allogeneic bone, and demineralized allogeneic bone powder in rats. J Korean Assoc Oral Maxillofac Surg. 1998; 24:380–395.
33. Oh DW, Lee SH, Shin HI. Histologic evaluation of the ectopic bone formation induced by partially purified BMP-fibrous glass membrane complex. J Korean Assoc Oral Maxillofac Surg. 1996; 22:86–100.
34. Park JC, Yu SB, Chung YI, Tae GY, Kim JJ, Park YD, et al. Bone regeneration with MMP sensitive hyaluronic acid-based hydrogel, rhBMP-2 and nanoparticles in rat calvarial critical size defect(CSD) model. J Korean Assoc Oral Maxillofac Surg. 2009; 35:137–145.
35. Kim SJ, Kim MR, Oh JS, Han I, Shin SW. Effects of polycaprolactone-tricalcium phosphate, recombinant human bone morphogenetic protein-2 and dog mesenchymal stem cells on bone formation: pilot study in dogs. Yonsei Med J. 2009; 50:825–831. PMID: 20046425.

36. Lee JH, Kim CS, Choi KH, Jung UW, Yun JH, Choi SH, et al. The induction of bone formation in rat calvarial defects and subcutaneous tissues by recombinant human BMP-2, produced in Escherichia coli. Biomaterials. 2010; 31:3512–3519. PMID: 20149447.

37. Schmidt-Schultz TH, Schultz M. Intact growth factors are conserved in the extracellular matrix of ancient human bone and teeth: a storehouse for the study of human evolution in health and disease. Biol Chem. 2005; 386:767–776. PMID: 16201872.

38. Gao J, Symons AL, Bartold PM. Expression of transforming growth factor-beta 1 (TGF-beta1) in the developing periodontium of rats. J Dent Res. 1998; 77:1708–1716. PMID: 9759668.
39. Finkelman RD, Mohan S, Jennings JC, Taylor AK, Jepsen S, Baylink DJ. Quantitation of growth factors IGF-I, SGF/IGF-II, and TGF-beta in human dentin. J Bone Miner Res. 1990; 5:717–723. PMID: 2396498.
40. Rocha LB, Goissis G, Rossi MA. Biocompatibility of anionic collagen matrix as scaffold for bone healing. Biomaterials. 2002; 23:449–456. PMID: 11761165.

41. Rosa FP, Lia RC, de Souza KO, Goissis G, Marcantonio E Jr. Tissue response to polyanionic collagen: elastin matrices implanted in rat calvaria. Biomaterials. 2003; 24:207–212. PMID: 12419620.

42. Maki F, Murata M, Kitajo H, Sato D, Taira H, Arisue M. Bone healing in large mandibular defects without periosteum in adult rabbits: a new application of collagenous sponge for bone regeneration. J Hard Tissue Biol. 2000; 9:56–62.
43. Nampo T, Watahiki J, Enomoto A, Taguchi T, Ono M, Nakano H, et al. A new method for alveolar bone repair using extracted teeth for the graft material. J Periodontol. 2010; 81:1264–1272. PMID: 20476887.

44. Linde A. Dentin matrix proteins: composition and possible functions in calcification. Anat Rec. 1989; 224:154–166. PMID: 2672882.

45. Gongloff RK. Vital root retention. A 5-year experience. Int J Oral Maxillofac Surg. 1986; 15:33–38. PMID: 3083004.
46. Fareed K, Khayat R, Salins P. Vital root retention: a clinical procedure. J Prosthet Dent. 1989; 62:430–434. PMID: 2585312.

47. Freedman GL. Intentional partial odontectomy: report of case. J Oral Maxillofac Surg. 1992; 50:419–421. PMID: 1545302.
48. Tsukamoto-Tanaka H, Ikegame M, Takagi R, Harada H, Ohshima H. Histochemical and immunocytochemical study of hard tissue formation in dental pulp during the healing process in rat molars after tooth replantation. Cell Tissue Res. 2006; 325:219–229. PMID: 16596394.

49. Takamori Y, Suzuki H, Nakakura-Ohshima K, Cai J, Cho SW, Jung HS, et al. Capacity of dental pulp differentiation in mouse molars as demonstrated by allogenic tooth transplantation. J Histochem Cytochem. 2008; 56:1075–1086. PMID: 18765839.

50. Hasegawa T, Suzuki H, Yoshie H, Ohshima H. Influence of extended operation time and of occlusal force on determination of pulpal healing pattern in replanted mouse molars. Cell Tissue Res. 2007; 329:259–272. PMID: 17497176.

51. Bang G, Urist MR. Bone induction in excavation chambers in matrix of decalcified dentin. Arch Surg. 1967; 94:781–789. PMID: 4226076.

52. Yeomans JD, Urist MR. Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues. Arch Oral Biol. 1967; 12:999–1008. PMID: 4226721.

53. Carvalho VA, Tosello Dde O, Salgado MA, Gomes MF. Histomorphometric analysis of homogenous demineralized dentin matrix as osteopromotive material in rabbit mandibles. Int J Oral Maxillofac Implants. 2004; 19:679–686. PMID: 15508983.
54. Gomes MF, Banzi EC, Destro MF, Lavinicki V, Goulart MD. Homogenous demineralized dentin matrix for application in cranioplasty of rabbits with alloxan-induced diabetes: histomorphometric analysis. Int J Oral Maxillofac Implants. 2007; 22:939–947. PMID: 18271375.
55. Bessho K, Tagawa T, Murata M. Purification of bone morphogenetic protein derived from bovine bone matrix. Biochem Biophys Res Commun. 1989; 165:595–601. PMID: 2597148.

56. Nilsson OS, Urist MR, Dawson EG, Schmalzried TP, Finerman GA. Bone repair induced by bone morphogenetic protein in ulnar defects in dogs. J Bone Joint Surg Br. 1986; 68:635–642. PMID: 3733844.

57. Sato K, Urist MR. Induced regeneration of calvaria by bone morphogenetic protein (BMP) in dogs. Clin Orthop Relat Res. 1985; (197):301–311. PMID: 4017344.

58. Urist MR. Experimental delivery systems for bone morphogenetic protein. In : Wise DL, Altobelli DE, Schwartz ER, Gresser JD, Trantolo DJ, Yaszemski M, editors. Handbook of biomaterials and applications. Section 3: Orthopaedic biomaterials applications. Boston: Marcel Dekker;1995. p. 1093–1133.
59. Herford AS, Boyne PJ. Reconstruction of mandibular continuity defects with bone morphogenetic protein-2 (rhBMP-2). J Oral Maxillofac Surg. 2008; 66:616–624. PMID: 18355584.

60. Jung RE, Weber FE, Thoma DS, Ehrbar M, Cochran DL, Hämmerle CH. Bone morphogenetic protein-2 enhances bone formation when delivered by a synthetic matrix containing hydroxyapatite/tricalciumphosphate. Clin Oral Implants Res. 2008; 19:188–195. PMID: 18067602.

61. Boerckel JD, Kolambkar YM, Dupont KM, Uhrig BA, Phelps EA, Stevens HY, et al. Effects of protein dose and delivery system on BMP-mediated bone regeneration. Biomaterials. 2011; 32:5241–5251. PMID: 21507479.

62. Ike M, Urist MR. Recycled dentin root matrix for a carrier of recombinant human bone morphogenetic protein. J Oral Implantol. 1998; 24:124–132. PMID: 9893518.

63. Yagihashi K, Miyazawa K, Togari K, Goto S. Demineralized dentin matrix acts as a scaffold for repair of articular cartilage defects. Calcif Tissue Int. 2009; 84:210–220. PMID: 19183824.

64. Murata M. Bone engineering using human demineralized dentin matrix and recombinant human BMP-2. Hard Tissue Biol. 2005; 14:80–81.

65. Murata M, Akazawa T, Hino J, Tazaki J, Ito K, Arisue M. Biochemical and histo-morphometrical analyses of bone and cartilage induced by human decalcified dentin matrix and BMP-2. Oral Biol Res. 2011; 35:9–14.
66. Urist MR. Bone histogenesis and morphogenesis in implants of demineralized enamel and dentin. J Oral Surg. 1971; 29:88–102. PMID: 4927173.
67. Inoue T, Deporter DA, Melcher AH. Induction of cartilage and bone by dentin demineralized in citric acid. J Periodontal Res. 1986; 21:243–255. PMID: 2941557.

68. Murata M, Kawai T, Kawakami T, Akazawa T, Tazaki J, Ito K, et al. Human acid-insoluble dentin with BMP-2 accelerates boneinduction in subcutaneous and intramuscular tissues. J Ceram Soc Jpn. 2010; 118:438–441.
69. Bang G. Induction of heterotopic bone formation by demineralized dentin in guinea pigs: antigenicity of the dentin matrix. J Oral Pathol. 1972; 1:172–185. PMID: 4125138.

70. Bang G. Induction of heterotopic bone formation by demineralized dentin: an experimental model in guinea pigs. Scand J Dent Res. 1973; 81:240–250. PMID: 4269633.

71. Urist MR, Dowell TA, Hay PH, Strates BS. Inductive substrates for bone formation. Clin Orthop Relat Res. 1968; 59:59–96. PMID: 4969827.

72. Huggins CB, Urist MR. Dentin matrix transformation: rapid induction of alkaline phosphatase and cartilage. Science. 1970; 167:896–898. PMID: 5410857.

73. Reddi AH, Huggins C. Biochemical sequences in the transformation of normal fibroblasts in adolescent rats. Proc Natl Acad Sci U S A. 1972; 69:1601–1605. PMID: 4504376.

74. Reddi AH, Anderson WA. Collagenous bone matrix-induced endochondral ossification hemopoiesis. J Cell Biol. 1976; 69:557–572. PMID: 1270511.

75. Urist MR, DeLange RJ, Finerman GA. Bone cell differentiation and growth factors. Science. 1983; 220:680–686. PMID: 6403986.

76. Tazaki J, Murata M, Yusa T, Akazawa T, Ito K, Hino J, et al. Autograft of human tooth and demineralized dentin matricesfor bone augmentation. J Ceram Soc Jpn. 2010; 118:442–445.
77. Lee HJ. Quantitative analysis of proliferation and differentiation of MG-63 cell line on the bone grafting material using human tooth [PhD thesis]. 2011. Seoul: School of Dentistry, Seoul National University.
78. Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, et al. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:496–503. PMID: 20060336.

79. Kim YK. Clinical application and classification of bone graft material according to component. J Korean Dent Assoc. 2010; 48:263–274.
80. Jeong HR, Hwang JH, Lee JK. Effectiveness of autogenous tooth bone used as a graft material for regeneration of bone in miniature pig. J Korean Assoc Oral Maxillofac Surg. 2011; 37:375–379.

81. Catanzaro-Guimarães SA, Catanzaro Guimarães BP, Garcia RB, Alle N. Osteogenic potential of autogenic demineralized dentin implanted in bony defects in dogs. Int J Oral Maxillofac Surg. 1986; 15:160–169. PMID: 3083019.

82. Gomes MF, dos Anjos MJ, Nogueira TO, Guimarães SA. Histologic evaluation of the osteoinductive property of autogenous demineralized dentin matrix on surgical bone defects in rabbit skulls using human amniotic membrane for guided bone regeneration. Int J Oral Maxillofac Implants. 2001; 16:563–571. PMID: 11516004.
83. Gomes MF, dos Anjos MJ, Nogueira Tde O, Catanzaro Guimarães SA. Autogenous demineralized dentin matrix for tissue engineering applications: radiographic and histomorphometric studies. Int J Oral Maxillofac Implants. 2002; 17:488–497. PMID: 12182291.
84. Gomes MF, Abreu PP, Morosolli AR, Araújo MM, Goulart Md. Densitometric analysis of the autogenous demineralized dentin matrix on the dental socket wound healing process in humans. Braz Oral Res. 2006; 20:324–330. PMID: 17242793.

85. Murata M, Sato D, Hino J, Akazawa T, Tazaki J, Ito K, et al. Acid-insoluble human dentin as carrier material for recombinant human BMP-2. J Biomed Mater Res A. 2012; 100:571–577. PMID: 22213638.

86. Ryu SY, Park SI, Kim SH. Effects of demineralized dentin matrix on osseointegration of implants in dogs. J Korean Assoc Oral Maxillofac Surg. 1996; 22:15–27.
87. Shapoff CA, Bowers GM, Levy B, Mellonig JT, Yukna RA. The effect of particle size on the osteogenic activity of composite grafts of allogeneic freeze-dried bone and autogenous marrow. J Periodontol. 1980; 51:625–630. PMID: 7007609.

88. Bhaskar SN, Cutright DE, Knapp MJ, Beasley JD, Perez B, Driskell TD. Tissue reaction to intrabony ceramic implants. Oral Surg Oral Med Oral Pathol. 1971; 31:282–289. PMID: 5277379.

89. Hosny M, Sharawy M. Osteoinduction in young and old rats using demineralized bone powder allografts. J Oral Maxillofac Surg. 1985; 43:925–931. PMID: 3906057.

90. Murata M, Akazawa T, Mitsugi M, Um IW, Kim KW, Kim YK, Pignatello R. Human dentin as novel biomaterial for bone regeneration. Biomaterials-physics and chemistry. 2011. p. 127–140.
91. Miyata Y, Ozawa S, Kojima N, Kondo Y, Matuskawa R, Tanaka Y. An experimental study of bone grafting using rat milled tooth. Int J Oral Maxillofac Implants. 2011; 26:1210–1216. PMID: 22167425.
92. Kim SG, Yeo HH, Kim YK. Grafting of large defects of the jaws with a particulate dentin-plaster of paris combination. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:22–25. PMID: 10442940.
93. Kim JY, Kim KW, Um IW, Kim YK, Lee JK. Bone healing capacity of demineralized dentin matrix materials in a mini-pig cranium defect. J Korean Dent Sci. 2012; 5:21–28.

94. Kim YK, Lee JY. The evaluation of postoperative safety of autogenous teeth bone graft. J Korean Acad Implant Dent. 2009; 28:29–35.
95. Kim YK, Kim SG, Kim KW, Um IW. Extraction socket preservation and reconstruction using autogenous tooth bone graft: case report. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:264–269.
96. Kim YK, Yi YJ. Horizontal ridge augmentation using ridge expansion and autogenous tooth bone graft: a case report. J Dent Rehabil Appl Sci. 2011; 27:109–115.
97. Kim YK, Lee HJ, Kim KW, Kim SG, Um IW. Guide bone regeneration using autogenous teeth: case reports. J Korean Assoc Oral Maxillofac Surg. 2011; 37:142–147.

98. Kim YK, Kim SG, Um IW. Vertical and horizontal ridge augmentation using autogenous tooth bone graft materials: case report. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:166–170.
99. Lee JH, Kim SG, Moon SY, Oh JS, Kim YK. Clinical effectiveness of bone grafting material using autogenous tooth: preliminary report. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:144–148.
100. Jeong KI, Kim SG, Kim YK, Oh JS, Jeong MA, Park JJ. Clinical study of graft materials using autogenous teeth in maxillary sinus augmentation. Implant Dent. 2011; 20:471–475. PMID: 22067601.

101. Jeong KI, Kim SG, Oh JS, Lim SC. Maxillary sinus augmentation using autogenous teeth: preliminary report. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:256–263.
102. Park SM, Um IW, Kim YK, Kim KW. Clinical application of auto-tooth bone graft material. J Korean Assoc Oral Maxillofac Surg. 2012; 38:2–8.

103. Lee JY, Kim YK, Kim SG, Lim SC. Histomorphometric study of sinus bone graft using various graft material. J Dent Rehabil Appl Sci. 2011; 27:141–147.
104. Lee JY, Kim YK. Retrospective cohort study of autogenous tooth bone graft. Oral Biol Res. 2012; 36:39–43.
Fig. 1
A. Extracted teeth are ready to be fabricated into autogenous tooth bone graft (AutoBT) in either powder form or block form. B. AutoBT powder. C. AutoBT block form.
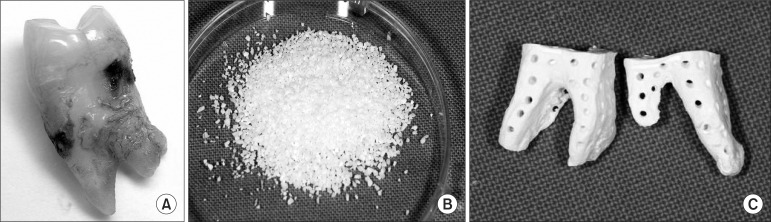
Fig. 2
A case of sinus bone graft and delayed implant placement in the left maxillary first molar in a 32-year-old female patient. AutoBT powder was used as bone graft material. A. Pre-surgery computed tomography. B. Four months' post-operative computed tomography. C. Panoramic x-ray soon after implant placement.
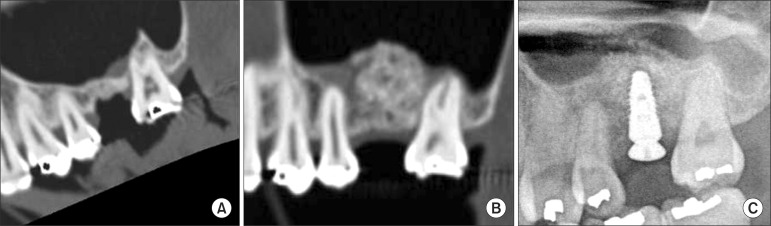
Fig. 3
A case of autogenous tooth bone graft (AutoBT) block socket graft followed by implant placement in a 41-year-old female patient. A. Pre-surgery panoramic x-ray showed bony defect with close proximity to the inferior alveolar nerve after extraction of the left mandibular second molar. B. The AutoBT block form fabricated from the extracted tooth was grafted at the extraction socket. C. Well-formed new bones were observed after raising a flap 5 months after the socket graft. D. Short wide implant was placed at the site. E. Periapical radiograph 6 months after the final prosthesis.
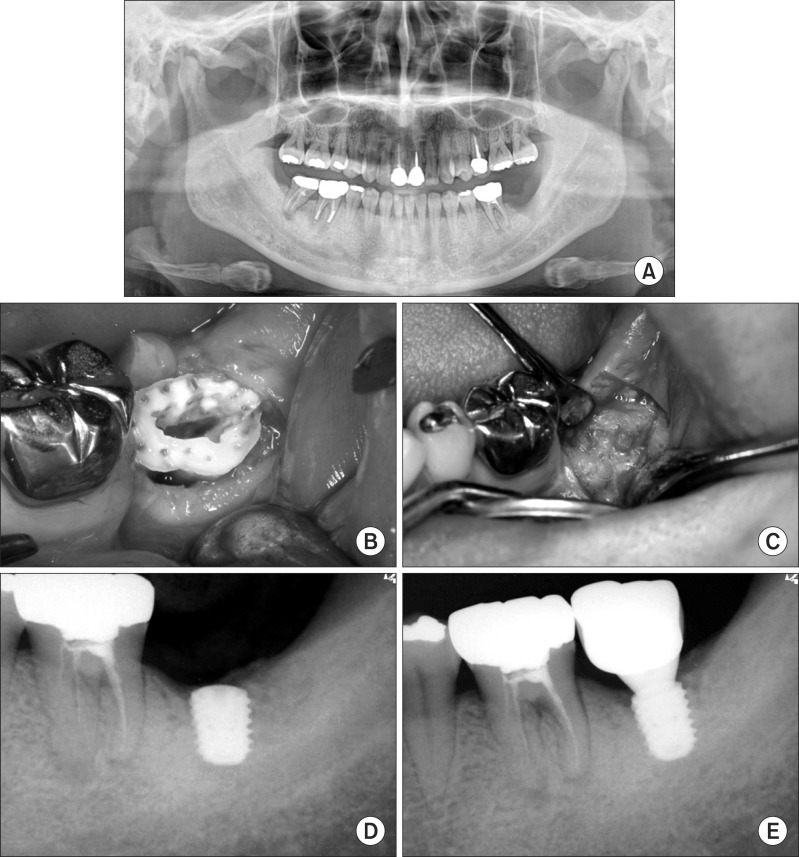
Fig. 4
A. High-magnification image of new bone formation around the tooth elements. Marginal scalloping of the implant chip suggested that remodeling was occurring in the new bone-implant chip interface.(H&E staining, ×100) B. Newly formed bone and tooth materials showing remodeling were identified around the implant chip and at the periphery of the implant chip, respectively.(H&E staining, ×100)
Images from the article of Kim et al.78 (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:496-503).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download