Abstract
Background
Recent advances in laboratory information systems have largely been focused on automation. However, the phlebotomy services have not been completely automated. To address this issue, we introduced an automated reception and turnaround time (TAT) management system, for the first time in Korea, whereby the patient's information is transmitted directly to the actual phlebotomy site and the TAT for each phlebotomy step can be monitored at a glance.
Methods
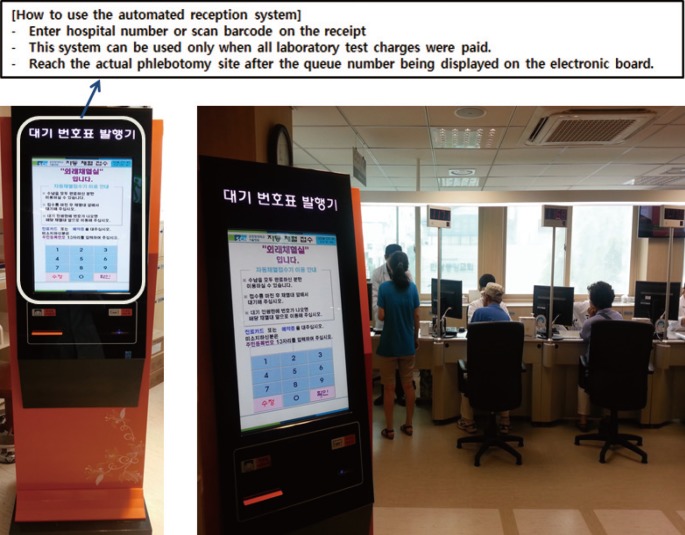
The GNT5 system (Energium Co., Ltd., Korea) was installed in June 2013. The automated reception and TAT management system has been in operation since February 2014. Integration of the automated reception machine with the GNT5 allowed for direct transmission of laboratory order information to the GNT5 without involving any manual reception step. We used the mean TAT from reception to actual phlebotomy as the parameter for evaluating the efficiency of our system.
Results
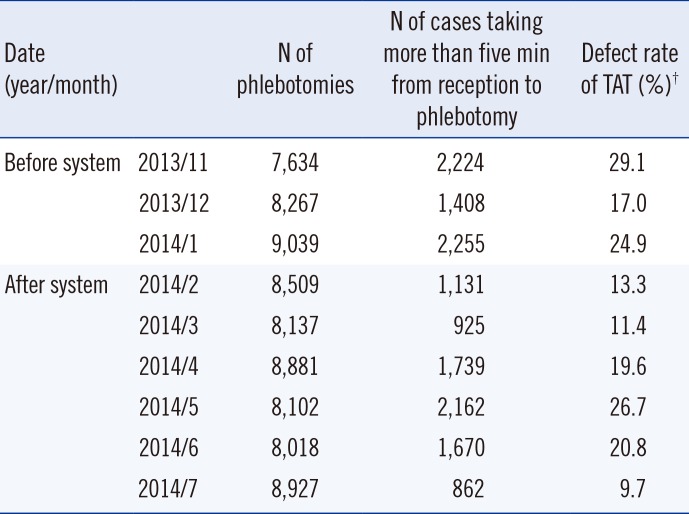
Mean TAT decreased from 5:45 min to 2:42 min after operationalization of the system. The mean number of patients in queue decreased from 2.9 to 1.0. Further, the number of cases taking more than five minutes from reception to phlebotomy, defined as the defect rate, decreased from 20.1% to 9.7%.
Since the 1990s, medical information systems have rapidly evolved around the order communication system (OCS), which consists of various components such as the hospital information system (HIS), electronic medical records (EMR), picture archiving communication system (PACS), and management information system (MIS). The laboratory information system (LIS) has also improved considerably, focusing on automation in response to the increased workload and the need to improve quality [1].
However, in the case of phlebotomy services, despite efforts at improving the workflow, the inconvenience to patients has not been completely mitigated. Until January 2014, patients in our hospital were required to obtain a queue number from a machine, followed by manual entry of the patient's identification number into the OCS in order of queue number and issuance of another queue number for the actual phlebotomy. These repetitive waiting steps increased the overall turnaround time (TAT) of the phlebotomy service and lead to patient dissatisfaction with the hospital service. Moreover, the automatic barcode labeling and test tube transfer system implemented in 2013 to improve work efficiency could not achieve its maximum performance because of the bottleneck at the manual reception steps.
To address these issues, we installed an automated reception machine and developed a TAT management system through which patient information and requested laboratory tests were transmitted directly to the actual phlebotomy site in a single step, and the TAT of each phlebotomy step could be monitored at a glance. This system has been functional since February 2014, remarkably decreased the overall TAT, and improved the workflow and efficiency at the phlebotomy room.
Our hospital is a 750-bedded tertiary care university hospital, with 95,711 outpatients (an average of 400 patients per day) availing the outpatient phlebotomy services in 2013. The GNT5 system ver. 2.2 (Energium Co., Ltd., Siheung, Korea) comprising of a Barcode Applicator (BA), Test Tube Transfer (TTA), and Medic Work Table (MWT) has been in operation in the phlebotomy room since June 2013 (Fig. 1). Installation of an automated reception machine and development of a TAT management program was achieved by July 2013 and fully operationalized in February 2014 (Fig. 2). By integrating the GNT5 and automated reception machine using a computerized order transmission program, laboratory order information received by the automated reception machine at the time of the patient's visit at the phlebotomy room is transmitted directly to the GNT5 system. As a result, the phlebotomist automatically received the barcode-labeled test tubes for corresponding patients and could verify the patient's information in the LIS program in a single step. A TAT management system for phlebotomy was concomitantly under development.
During this developmental phase, a preparatory committee that comprised of members from the laboratory medicine, outpatient, hospital administration, and data processing departments worked for addressing the following issues.
For tests requiring serial samples such as glucose tolerance tests, all relevant information is transmitted to the phlebotomy site at the reception; therefore, patients do not have to repeatedly pass through the reception step but can directly reach the actual phlebotomy site for the second phlebotomy.
We organized laboratory orders for tests that require special attention (e.g., a patient consent form, administration of specific medicine, requirement for fasting, requirement for special test tubes, shielding of tubes from direct light) such that the corresponding caution messages were printed on the queue number ticket issued from the automated reception machine. This mechanism allowed for cross-verification of the precautions mentioned on the queue number ticket with that in the LIS program by the phlebotomist, thus minimizing the room for error.
Physicians are obligated to specify the desired date of phlebotomy when they order laboratory tests at the outpatient department (OPD). It was noted that phlebotomy could be performed within one week before or after the desired date. If the patient's visit to the phlebotomy room does not fall within the applicable period, a message such as 'Please contact the hospital staff' appeared on the screen of the automated reception machine, allowing the phlebotomist to consult with the corresponding OPD on whether or not to perform the phlebotomy at that time. Moreover, in the case of patients whose phlebotomy should be performed on a specified date, physicians can use the 'Lock' function to specify that the phlebotomy can be performed only on the desired date.
Before installing these systems, unpaid laboratory test charges were not conveyed to patients unless the patient was manually registered by a staff member, requiring an extra visit to the hospital administration. To alleviate this problem, the new system presents any information about unpaid charges via the message 'Please visit the hospital administration for payment' on the automated reception machine.
Different tests require different numbers and types of test tubes. At the time of reception, the system automatically allocates the test tubes according to the test and automatically transmits this information to the GNT5 system.
At reception, the laboratory order transmission system automatically checks for unperformed or missed laboratory tests within the 15-month period preceding the day of visit and processes them en bloc unless there is a special comment from the physician. The 15-month period was arbitrarily determined with consideration of the server processing capacity of our HIS.
We developed a TAT monitoring program that allowed for monitoring of each step of the phlebotomy process starting from the allocation of queue number ticket to the actual phlebotomy (Fig. 3). The program allowed for real-time monitoring of the time elapsed between reception and the actual phlebotomy, queue time, number of tubes used, and name of the phlebotomist. Moreover, this program could be monitored at the central laboratory located on a different floor and it could facilitate rapid mobilization of extra manpower in case of need.
The Mann-Whitney test was used to compare the mean TAT from issuing of queue number ticket to actual phlebotomy before and after installing of the automated reception and TAT management system. The Chi-square test was used to compare the defect rate of TAT before and after installing of the automated reception and TAT management system.
The schematic representation of the entire process from reception to blood sampling after installation of the automated reception and TAT management system is presented in Fig. 4. The rate of incomplete reception was 30.6% in the initial phase after system operationalization (February 2014), but decreased with time (8.2% in March, 11.2% in April, 11.5% in May, 11.0% in June and 13.2% in July).
The mean TAT from issuing of queue number ticket to actual phlebotomy was used as a parameter for evaluating the efficiency of the automated reception and TAT management system. Prior to system installation, the range of mean TAT was 4:14-5:45 (min:sec). After implementation of the system in February 2014, the mean TAT decreased to 2:42 in July 2014 (P=0.000) (Table 1). Further, the mean number of patients in the queue decreased from 2.9 in November 2013 to 1.0 in July 2014, irrespective of the number of test tubes needed for phlebotomy (P=0.000) (Table 1).
A TAT goal of <5 min from reception to phlebotomy was set on the basis of time required from reception to phlebotomy before operationalization of the system (from November 2013 to January 2014, 3:12-4:28 min:sec) and defined the proportion of cases taking more than five minutes as the defect rate. The defect rate decreased from 29.1% in November 2013 (before installing the system) to 9.7% in July 2014 (P<0.001) (Table 2).
Quality can be defined as the ability of a product or service to satisfy the needs and expectations of a customer [2]. In the case of a hospital's outpatient phlebotomy room, waiting time is one of the most important factors affecting patient satisfaction with the service. Therefore, reducing the waiting time through more efficient workflow could improve the quality of the phlebotomy service.
Since 2013, we have operated the GNT system in our hospital's outpatient phlebotomy room to improve the efficiency of workflow. The GNT system is a phlebotomy assistance system that helps prevent medical accidents, reduces waiting time, and improves the convenience for both patients and phlebotomists. The system automatically provides phlebotomists with essential items required for a phlebotomy (the appropriately labeled specimen tube, a specimen label, a patient identification label) based on the phlebotomy information recorded in the hospital information system (i.e., HIS, LIS, OCS) [3]. However, despite the automated barcode application and tube transfer functions of this system, the manual reception step was a bottleneck that limited the efficiency of the phlebotomy services. Moreover, the risk of human error at the point of pre-phlebotomy reception performed by a phlebotomist unaided by automation was exacerbated by increase in outpatient attendance alongside a decrease in the number of laboratory personnel and the human error that resulted from physical and mental fatigue [4567].
To address this issue, we introduced an automated reception machine and developed a laboratory order transmission program connected to LIS and OCS with full consideration of the circumstances in our hospital. These included the desired phlebotomy date, processing of unpaid charges, and time period for noting unperformed or missed tests.
TAT is the most frequently used indicator of efficiency of the laboratory test ordering process [8]. We used a TAT management program developed to monitor the efficiency of our phlebotomy service. This program can monitor each step of the phlebotomy process from reception to actual phlebotomy; therefore, if a problem arises in the phlebotomy room, we can analyze and address the matter by examining each step of the process. Moreover, our program can be monitored remotely. This functionality can help improve system efficiency by allowing for real time identification and troubleshooting of problems. This functionality is of particular value in health care settings where the central laboratory is located separately from the phlebotomy room.
After installing the automated reception and TAT management system in February 2014, both the TAT for each phlebotomy step and the number of patients in the queue were significantly reduced. Moreover, there was a significant decrease in the defect rate, a parameter that we defined as the number of cases where the time between reception and phlebotomy exceeded five minutes, after implementing the system.
Laboratory services are an integral and essential part of clinical service delivery. The department of laboratory medicine must be centrally involved in the planning and implementation process, for these systems to bring about improvements in system efficiency. Moreover, successful implementation requires the building of new relationships and improved level of hospital-wide collaboration. Formal channels of communication between multidisciplinary groups are crucial for real time problem solving [891011]. We found that a consensus among the OPD, hospital administration, and data processing department was essential during the developmental process, because the heterogeneity in outpatient practices presents a unique set of challenges for harmonization of the system across various specialties and departments. For example, in the outpatient setting, days or even weeks may elapse between placement of an order and collection of the specimen [121314].
This is the first application of the automated reception and TAT management system to phlebotomy services in Korea. We expect that our system will provide a platform to streamline workflow in other hospital phlebotomy rooms. Additional details such as management of redundant orders requested from different OPDs should be discussed in the future to further improve the efficiency of the system and to enhance the satisfaction of physicians and patients.
References
1. Streitberg GS, Angel L, Sikaris KA, Bwititi PT. Automation in clinical biochemistry: core, peripheral, STAT, and specialist laboratories in Australia. J Lab Autom. 2012; 17:387–394. PMID: 22661200.
2. Hawkins RC. Laboratory turnaround time. Clin Biochem Rev. 2007; 28:179–194. PMID: 18392122.
3. GNT system introduction. Update on Jan 2014. http://www.gobizkorea.com/catalog/product_view.jsp?blogId=1308180833&listStyle=A&objId=1093197.
4. Da Rin G. Pre-analytical workstations: a tool for reducing laboratory errors. Clin Chim Acta. 2009; 404:68–74. PMID: 19302988.
5. Wallin O, Söderberg J, Van Guelpen B, Stenlund H, Grankvist K, Brulin C. Preanalytical venous blood sampling practices demand improvement--a survey of test-request management, test-tube labelling and information search procedures. Clin Chim Acta. 2008; 391:91–97. PMID: 18342012.
6. Hawker CD. Laboratory automation: total and subtotal. Clin Lab Med. 2007; 27:749–770. viPMID: 17950896.
7. Lippi G, Guidi GC. Risk management in the preanalytical phase of laboratory testing. Clin Chem Lab Med. 2007; 45:720–727. PMID: 17579523.
8. Georgiou A, Westbrook JI. Computerised order entry systems and pathology services--a synthesis of the evidence. Clin Biochem Rev. 2006; 27:79–87. PMID: 17077878.
9. Georgiou A, Westbrook J, Braithwaite J, Iedema R. Multiple perspectives on the impact of electronic ordering on hospital organisational and communication processes. HIM J. 2006; 34:130–135. PMID: 18216417.
10. Stablein D, Welebob E, Johnson E, Metzger J, Burgess R, Classen DC. Understanding hospital readiness for computerized physician order entry. Jt Comm J Qual Saf. 2003; 29:336–344. PMID: 12856555.
11. Davidson EJ, Chismar WG. Planning and managing computerized order entry: a case study of IT-enabled organizational transformation. Top Health Inf Manage. 1999; 19:47–61. PMID: 10387655.
12. Baron JM, Dighe AS. Computerized provider order entry in the clinical laboratory. J Pathol Inform. 2011; 2:35. PMID: 21886891.
13. Pantanowitz L, Henricks WH, Beckwith BA. Medical laboratory informatics. Clin Lab Med. 2007; 27:823–843. viiPMID: 17950900.
14. Valenstein P, Meier F. Outpatient order accuracy. A College of American Pathologists Q-Probes study of requisition order entry accuracy in 660 institutions. Arch Pathol Lab Med. 1999; 123:1145–1150. PMID: 10583917.
Fig. 1
Components of the GNT5 phlebotomy assistance system.
Abbreviations: BA, barcode applicator; TTT, test tube transfer; MWT, medic work table.
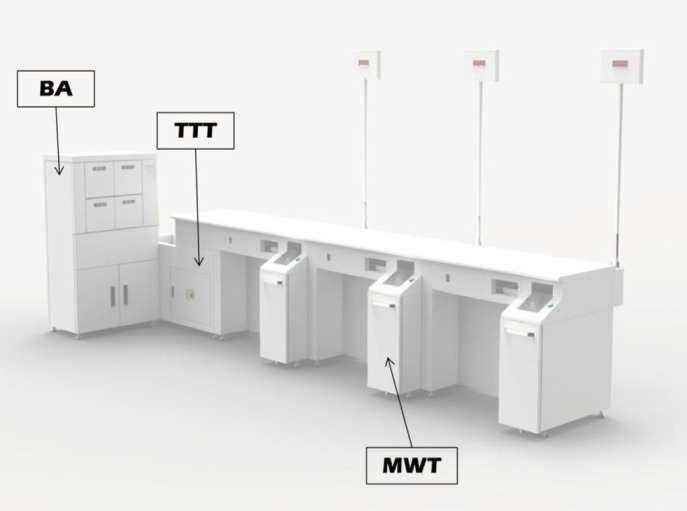
Fig. 3
A screenshot of the turnaround time (TAT) management program showing the user interface for real-time monitoring of each step of the phlebotomy process.
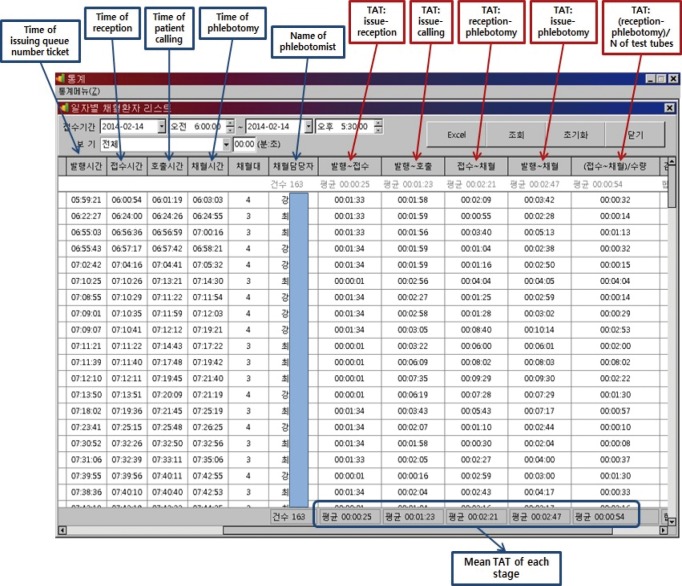
Fig. 4
Workflow at the outpatient phlebotomy room after installation of automated reception and turnaround time (TAT) management system.
Abbreviation: OPD, outpatient department.
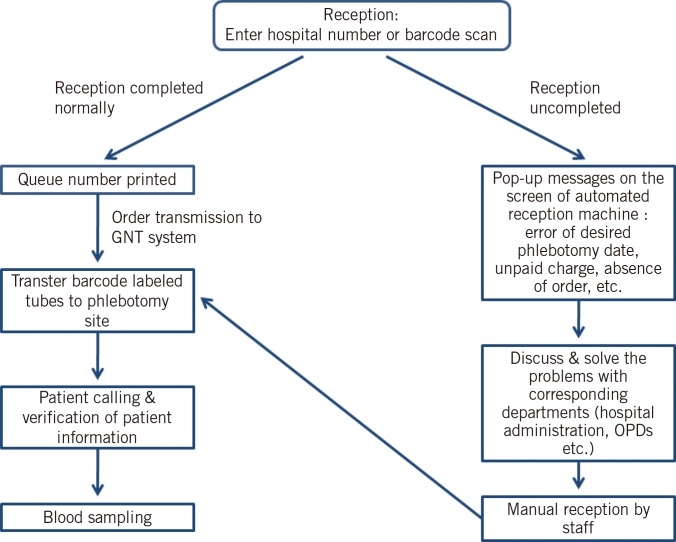
Table 1
Indices of work efficiency at the outpatient phlebotomy room before and after installation of the automated reception and TAT management system
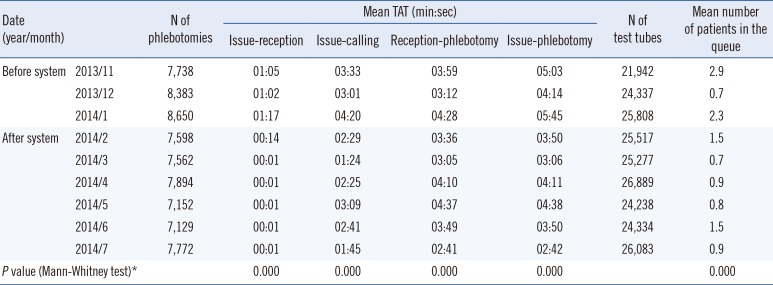
Table 2
Defect rate of TAT*




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download