Dear Editor
Pneumonia is a major cause of death worldwide, especially in aging and immunodeficient patients [1]. Common symptoms such as cough, fever, dyspnea, chest pain, and wheezes occur not only in pneumonia but also in many other illnesses. Early diagnosis of pneumonia is crucial, especially when symptoms are mild, to avoid overuse of antibiotics and prevent development of antibiotic resistance [2]. Therefore, rapid biomarkers are required to assist the initial evaluation and differentiation of low-grade pneumonia from upper respiratory infection (URI).
The delta neutrophil index (DNI), an automated hematology analyzer-based marker, was recently introduced. DNI is the fraction of immature granulocytes identified automatically by the ADVIA 2120i Hematology Analyzer (Siemens Healthcare Diagnostics Inc., Erlangen, Germany). DNI is associated with the diagnosis and prognosis of sepsis [34]. In this study, we evaluated the diagnostic power of DNI for the differentiation of low-grade community acquired pneumonia (CAP) from URI in patients with clinically ambiguous symptoms.
After obtaining approval from the institutional review board (IRB) of the Catholic Medical Center (IRB number: UC12SISI 0087), we recruited 127 patients (mean age±SD 58.3±24.2 yr, Table 1A) for the study, which was carried out from September 2013 through November 2013. The inclusion criterion for patients with low-grade CAP was low severity, according to the CURB-65 system (score 0 or 1) [5]. URI (known as the common cold) was defined as a typical acute infection involving the nose, paranasal sinuses, pharynx, larynx, and trachea without radiographic findings of pulmonary infiltrate. Patients without infection were used as the control group.
Total and differential leukocyte counts and DNI values were obtained with an ADVIA 2120i system. DNI was calculated with the following formula: DNI (%)=(neutrophil %+eosinophil % measured in the myeloperoxidase [MPO] channel with the cytochemical MPO reaction)-(polymorphonuclear neutrophil % measured in the nuclear lobularity channel). The level of C-reactive protein (CRP) was measured with a Hitachi 7600 Modular Chemistry Analyzer (Hitachi, Tokyo, Japan). Sputum and blood microbial cultures were performed before the start of antibiotic therapy. Among the 22 total isolates, the main CAP isolates were Staphylococcus aureus (n=9), Acinetobacter baumannii (n=4), Klebsiella pneumoniae (n=3), and Streptococcus pneumoniae (n=2). Bacteremia was found in two of 59 (3.4%) CAP patients and was not found in the URI and control groups. All of the patients recovered.
The results of biomarker determination in the three groups are presented as medians (first to third interquartile range) and were analyzed by Kruskal-Wallis test (Fig. 1). DNI was the highest in the low-grade CAP group, intermediate in the URI group, and the lowest in the control group (P<0.05). CRP, DNI, and lymphocyte and monocyte counts were significantly different between the low-grade CAP and the URI and control groups (P=0.001). Lymphocyte count was significantly different between the URI group and the control group (P=0.001). No significant differences in total leukocytes were observed among the groups.
An ROC analysis was performed to compare the diagnostic power for discriminating low-grade CAP from URI and controls (Table 1B). CRP, lymphocyte count, and DNI showed the highest areas under the curve (AUCs) among the tested biomarkers for the prediction of CAP. The optimal cutoffs for the prediction of CAP were DNI >1.7%, CRP >1.48 mg/L, neutrophils >5.23 ×109/L, and lymphocytes ≤1.57×109/L.
To investigate the diagnostic power of the combination of DNI, CRP, and lymphocyte count, we performed an ROC analysis with the following: sum of DNI %+CRP mg/L+(10 -lymphocytes [×109/L]). Compared with the individual biomarkers, the combination of DNI, CRP, and lymphocyte count had the highest AUC (0.974; see Table 1B). Furthermore, compared with the individual biomarkers, the combination of DNI and CRP had a higher AUC (0.949).
DNI is provided with complete blood count without additional cost and has the advantage of being rapid, thus providing results relatively quickly. DNI showed significantly better diagnostic power in the lower-grade CAP group than in the URI and control groups. Compared with DNI, total leukocytes and neutrophils showed less diagnostic power for differentiating CAP from URI. CRP showed the highest diagnostic power among individual biomarkers for differentiating low-grade CAP from URI. The combination of CRP and DNI increased the diagnostic power than individual biomarkers. Therefore, DNI may be useful for diagnosing CAP without additional cost, prescribing appropriate treatment in patients who need antibiotics, and preventing unnecessary use of antibiotics in patients with ambiguous clinical symptoms.
References
1. WHO. The top 10 causes of death. Updated on May 2014. http://www.who.int/mediacentre/factsheets/fs310/en/.
2. Wiemken TL, Peyrani P, Ramirez JA. Global changes in the epidemiology of community-acquired pneumonia. Semin Respir Crit Care Med. 2012; 33:213–219. PMID: 22718207.

3. Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, et al. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012; 37:242–246. PMID: 22258230.
4. Park BH, Kang YA, Park MS, Jung WJ, Lee SH, Lee SK, et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect Dis. 2011; 11:299. PMID: 22040292.

5. Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009; 64(S3):iii1–iii55. PMID: 19783532.

Fig. 1
Medians (and first to third interquartile ranges) of the delta neutrophil index (DNI, %), C-reactive protein (CRP), white blood cell (WBC) count, neutrophil count, lymphocyte count, and monocyte count in each group (A, pneumonia; B, upper respiratory infection; C, control).
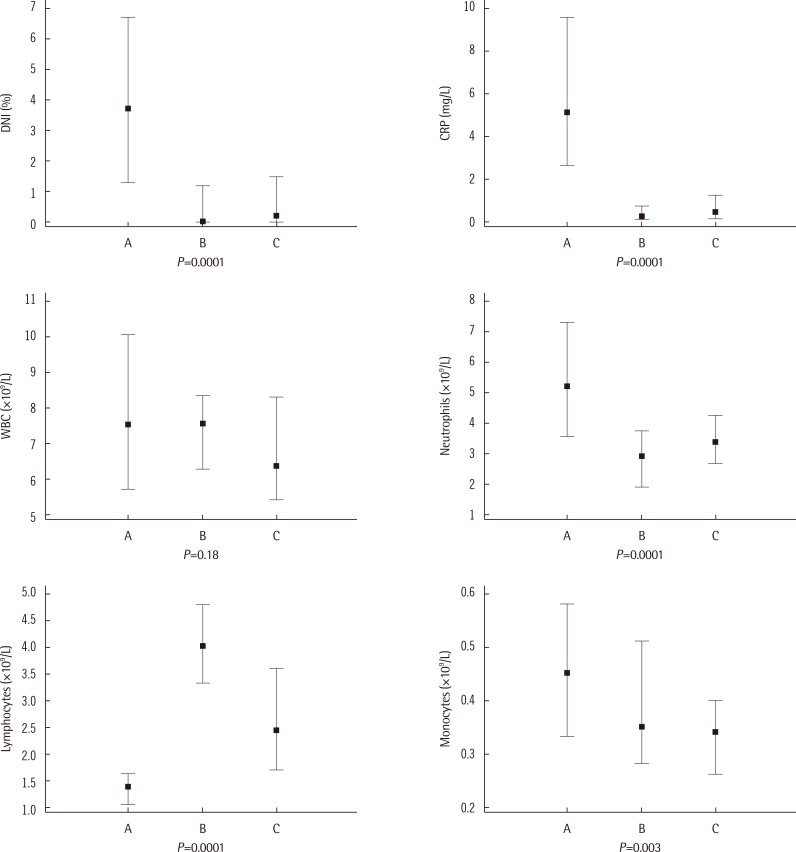
Table 1
(A) Clinical characteristics and (B) receiver operating characteristics analysis of biomarkers for the prediction of low-grade CAP
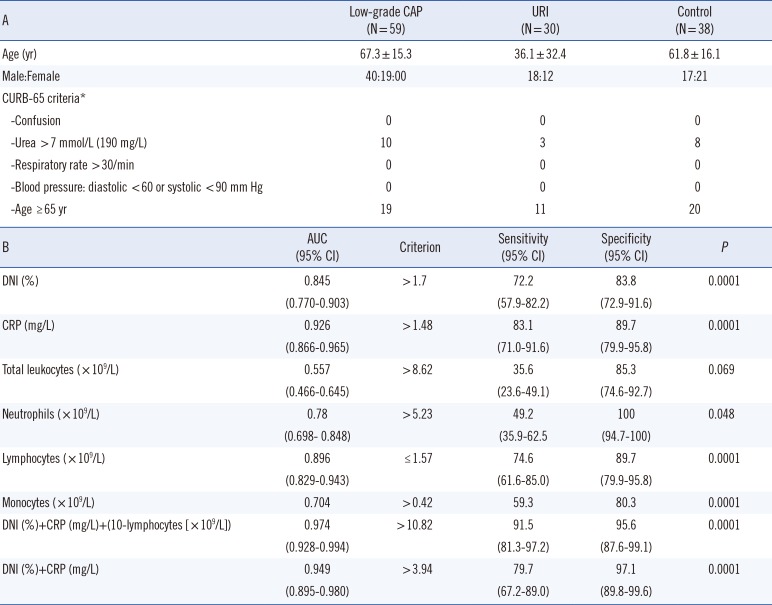
*CURB-65 score is the severity scoring system in pneumonia. The number of patients positive for each criterion is given in each group [5].
Abbreviations: AUC, area under the curve; CI, confidence interval; CAP, community-acquired pneumonia; CRP, C-reactive protein; DNI, delta neutrophil index; URI, upper respiratory infection.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download