Abstract
We report a case of large radicular cyst progression related to endodontic origin to emphasize proper intervention and follow-up for endodontic pathosis. A 25 yr old man presented with an endodontically treated molar with radiolucency. He denied any intervention because of a lack of discomfort. Five years later, the patient returned. The previous periapical lesion had drastically enlarged and involved two adjacent teeth. Cystic lesion removal and apicoectomy were performed on the tooth. Histopathological analysis revealed that the lesion was an inflammatory radicular cyst. The patient did not report any discomfort except for moderate swelling 3 days after the surgical procedure. Although the patient had been asymptomatic, close follow-ups are critical to determine if any periapical lesions persist after root canal treatment.
Previous epidemiological studies have shown that teeth with apical radiolucency are common.123 For example, after examination of 8,743 teeth in a French subpopulation, Boucher et al. reported that 22.7% were endodontically treated and among those treated teeth 24.4% had periapical radiolucency.3
Persistent periapical radiolucency after endodontic procedures may decrease, remain unchanged, or increase over time. Clinicians should consider factors including the quality of the current root canal treatment and the patient's symptoms before intervention. von Arx et al. analyzed 330 teeth referred to a specialist for apical surgery and reported that 59.1% of the referred cases went forward with apical surgery, 25.8% with extraction, 9.1% with no treatment, and 6.1% with nonsurgical retreatment.4 The decisions were made according to the probing depth, attached gingiva level, tooth mobility, pain, clinical signs, quality of canal filling, and periapical lesion size and location. In some situations, the patient may not want to receive intervention because of a lack of discomfort. Yu et al. reported that the incidence of painful exacerbation in persistent periapical lesions was 5.8% over 20 years.5
It remains unclear when clinicians should initiate interventions in asymptomatic root-filled teeth. In the present case, we present a drastic enlargement of a periapical lesion 5 years after the patient declined treatment for an endodontically treated tooth. We report this case to emphasize the importance of proper management and close follow-up of endodontically treated teeth with radiolucency.
In 2009, a 25 year old man was referred to the Department of Conservative Dentistry at Gangnam Severance Dental Hospital for evaluation and further treatment because of an apical pathosis on a lower left first molar. Nonsurgical endodontic treatment was performed on the tooth by the referring dentist because of apical radiolucency on the tooth 5 years previously (in 2005), and the patient was informed that the size of the apical radiolucency had increased. The patient could not recall the initial root canal treatment and did not experience any discomfort.
A panoramic radiograph obtained during the first visit to our institution showed a large, radiolucent area around a mesial root of tooth #36 (Figure 1a). Root canal fillings were found, and a metallic obstruction in one canal was noticed (Figures 1b and 1c). A clinical examination showed no remarkable findings, including tooth mobility, sensitivity to percussion, or swelling. We informed the patient of a large periapical radiolucency and that the possible treatment options were nonsurgical retreatment, surgical treatment, or extraction. In addition, because of the size of the lesion, computed tomography (CT) was suggested to evaluate the proximity of the lesion to the mandibular canal. However, because the patient was asymptomatic, he did not want to perform further radiographic examinations and active treatment. The patient was recommended to undergo a routine check-up before a final decision. However, the patient did not come for a follow-up without any notice.
Five years later, the patient came back because of cold sensitivity in the lower left molars. He felt moderate cold sensitivity during outdoor activity a week before this visit, and the sensitivity disappeared thereafter. He recalled his appointment scheduled in 2009 and decided to return for a check-up. A large cystic lesion involving the left lower premolar and molars was found in a panoramic radiograph (Figure 2a). Tooth #36 was negative for percussion and showed a normal range of mobility and periodontal probing. All adjacent teeth were asymptomatic and vital.
An oral surgeon at the Department of Oral Maxillofacial Surgery was consulted for surgical intervention. CT (Somatom Sensation 64, Siemens, Munich, Germany, 120 kVp, 90 mA) was performed to evaluate the size and location of the lesion. A large lesion was observed, in which the cortical bone was thinned and slightly expanded to the buccal and lingual sides (Figures 2b and 2c). Radiopaque particles were noticed inside the large radiolucent lumen, located approximately below the mesial root apex of tooth #36 (Figure 2d). The preliminary diagnosis of the lesion was a keratocystic odontogenic tumor (KCOT) in the left mandibular area. Possible differential diagnoses were calcifying odontogenic tumor, calcifying odontogenic cyst, apical periodontal cyst, and radicular cyst.
Surgical enucleation of the lesion under general anesthesia was planned, and basic tests required for surgical and general anesthetic procedures were performed. The patient was informed of possible numbness because of the proximity of the lesion to the inferior alveolar nerve, and he was also informed of the necessity of root canal treatment in the lower left first and second premolars and second molars if any signs of vitality loss were detected.
Under general anesthesia, cyst enucleation was performed with crevicular and vertical incisions between the lower left canine and the second molar. After the mucoperiosteal flap was elevated, the buccal cortical bone was detached by creating a window and maintained in sterile saline during the surgical procedure (Figure 3a). The lesion was enucleated after the mental foramen was protected. Beige-colored turbid thick fluid filled the inside of the lumen (Figure 3b). The cystic membrane was thin and torn easily from the bony cavity (Figure 3c). A 3 mm diameter calcific mass with hard and rough texture was found inside the lumen (Figure 3d). Small, yellowish, cheese-like particles were attached to the cystic membrane. An endodontic file was extruded from the mesiobuccal canal of the lower left first molar (Figure 3e). Apical root resection of both roots was performed under a microscope in the operating room. Apical leakage was noticed on both roots (Figures 3g and 3h), and the root canals were retroprepped and filled with ProRoot MTA (Dentsply Tulsa Dental Specialties, Tulsa, OK, USA) under a dental microscope (Figure 3f). The cystic lesion was sent to the Department of Oral Pathology at the College of Dentistry of Yonsei University for histopathological examination and diagnosed as an inflammatory radicular cyst (Figures 4a - 4c). The calcific mass was diagnosed as protein material with multifocal calcification, and it was suspected that canal filling material or intracanal medicament may have extruded into the apical lesion. After the surgical procedure, the patient did not have any obvious postoperative complications, with the exception of moderate swelling and slight pain for 3 - 4 days (Figure 3i). The patient returned for a one-month check-up and did not report any discomfort after the surgery. A 3 month check-up was scheduled.
When the patient was initially referred to our institution, apical surgery was the first option because of a file separation in one of the mesial canals. Based on the referring note, the apical lesion had enlarged before the patient visited our institution for the first time, demonstrating that the apical lesion on the tooth was deteriorating. Yu et al. reported that lesions existing for a longer period are less likely to heal.6 Furthermore, Santos et al. found that preoperative periapical lesions and the quality of canal fillings could affect postoperative periapical lesions.7 In this case, all canal fillings reached the proper length, but a separated metallic instrument was found in one buccal canal. These findings suggest that surgical endodontic retreatment would be required, if any intervention was needed.
To perform the apical tooth surgery, more information regarding the location of the mental foramen was important because the lesion was close to the mental foramen in the panoramic radiograph. Our recommendation to undergo CT imaging was rejected by the patient because he was not convinced that further treatment was necessary given the absence of discomfort, even though we informed him of the existence of apical pathosis on the tooth. Even though the patient was scheduled for a 3 month check-up to make a final decision, he did not show up, and the appointment was forgotten for the next 5 years.
Before the surgical procedure, the origin of the lesion was unclear. The initial diagnosis of the lesion was a KCOT, based on the rapid progression of the cystic lesion in the mandibular area.89 However, the histopathological findings revealed a nonkeratinized epithelial lining. Thus, we concluded that the previously incomplete endodontic treatment was the main cause of the radicular cyst.
Persistent endodontic lesions may progress by deteriorating or becoming enlarged. However, this is a rare case of an aggressive enlargement that required surgical intervention under general anesthesia. Even though the surgical intervention was successful in this case, it would have been beneficial to both the patient and operators if early detection and management had been provided. Therefore, this case report is a good example to emphasize the importance of regular check-ups for persistent endodontic lesions.
Figures and Tables
Figure 1
Initial radiograph findings when the patient first visited in 2009. (a) A panoramic radiograph revealed a periapical lesion on the mesial root of the left mandibular first molar (tooth #36); (b and c) Periapical radiographs showed radiolucency around the mesial root of tooth #36, and a metallic obstruction was noticed in one mesial canal.
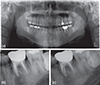
Figure 2
Radiographic findings in 2014. (a) A panoramic radiograph showed the progression of a cystic lesion around tooth #36, as compared to radiographs taken 5 years ago (Figure 1); (b and c) The computed tomography scan views demonstrated the thinning of the cortical plates on the buccal and lingual sides; (d) The coronal view showed a radiopaque material inside the lumen.

Figure 3
Clinical photos and a panoramic radiograph taken during the surgical procedure. (a) A bony window was prepared to save the cortical plate; (b) Pus-like turbid exudate from the lumen; (c) The cystic membrane was removed and sent for a biopsy; (d) A small, calcific material with a diameter of 3 mm was removed from the lumen; (e) An extruded endodontic file was observed in the mesial root; (f) Both roots were retrofilled with MTA. (g) The resected mesial root showed a metallic file in the mesiobuccal canal and leaked isthmus; (h) The resected distal root showed a filled canal with leakage; (i) Immediate postoperative panoramic radiograph.

Acknowlegements
This study was supported by the Yonsei University College of Dentistry Fund (6-2015-0105).
References
1. Allard U, Palmqvist S. A radiographic survey of periapical conditions in elderly people in a Swedish county population. Endod Dent Traumatol. 1986; 2:103–108.

2. Eriksen HM, Bjertness E. Prevalence of apical periodontitis and results of endodontic treatment in middle-aged adults in Norway. Endod Dent Traumatol. 1991; 7:1–4.

3. Boucher Y, Matossian L, Rilliard F, Machtou P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int Endod J. 2002; 35:229–238.

4. von Arx T, Roux E, Bürgin W. Treatment decisions in 330 cases referred for apical surgery. J Endod. 2014; 40:187–191.

5. Yu VS, Messer HH, Yee R, Shen L. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endod. 2012; 38:41–46.

6. Yu VS, Messer HH, Shen L, Yee R, Hsu CY. Lesion progression in post-treatment persistent endodontic lesions. J Endod. 2012; 38:1316–1321.

7. Santos SM, Soares JA, Costa GM, Brito-Júnior M, Moreira AN, de Magalhães CS. Radiographic parameters of quality of root canal fillings and periapical status: a retrospective cohort study. J Endod. 2010; 36:1932–1937.

8. Madras J, Lapointe H. Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc. 2008; 74:165–165h.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download