Abstract
A 9-year-old girl visited our hospital, complaining of a rapid-growing and rigid swelling on the left posterior mandibular area. Panoramic radiograph showed a moderately defined multilocular honeycomb appearance involving the left mandibular body. CT scan revealed an expansile, multilocular osteolytic lesion and multiple fluid levels within cystic spaces. Bone scan demonstrated increased radiotracer uptake and angiography showed a highly vascularized lesion. The lesion was suspected as aneurysmal bone cyst (ABC) and preoperative embolization was performed, which minimize the extent of operation and the surgical complication. The lesion was treated by surgical curettage and lateral decortication with repositioning. No additional treatment such as a surgical reconstruction or bone graft was needed. Early diagnosis of ABC is very important and appropriate treatment should be performed considering several factors such as age, surgical complication, and possibility of recurrence.
Aneurysmal bone cyst (ABC) is a relatively rare, benign osteolytic lesion.1,2 This lesion is predominantly found within the long bones,2,3 and only 2% occur in the jaws.4 Jaffe and Lichtenstein5 recognized this cystic lesion for the first time and distinguished it from other cystic lesions and giant cell tumors in 1942. The World Health Organization defined ABCs as expansive osteolytic lesions consisting of blood-filled spaces and channels divided by connective tissue septa that can contain osteoid tissue and osteoclast-like giant cells.6,7 Primary ABC is more common than secondary ABC that arises from pre-existing benign or malignant bone lesions.8
This report presents a case of ABC occurring at the posterior mandible managed by preoperative embolization and surgical curettage after lateral decortication with repositioning in 9-year-old girl.
A 9-year-old girl visited our hospital, complaining of a rapid-growing and rigid swelling of the left posterior mandibular area. The patient detected the swelling 3 days before the visitation. The clinical examination revealed swelling with fever on the left cheek area. The skin over the lesion appeared normal. The swelling had bony hard consistency and there was tenderness on palpation. The involved gingiva blanched on pressure but showed no pulsations or evidence of bleeding from the gingival sulcus. The overall appearance of the lesion gave a clinical impression of benign tumor of the mandible.
Panoramic radiograph was acquired with Orthopantomograph OP-100 (Instrumentarium Imaging, Tuusula, Finland) and revealed moderately defined multilocular radiolucencies with honeycomb appearance involving the left mandibular body area (Fig. 1A). It showed an external root resorption of the involved right deciduous second molar and the permanent first molar. The developing permanent second premolar was rotated and mesially displaced, and the permanent second molar was also displaced distally. Cortical expansion was evident inferiorly.
The patient's parent asked to remove her deciduous molar of the involved area, complaining of the tooth mobility. The surgeon did not suspect the intra-osseous vascular lesion and tried to extract the deciduous teeth without knowing the risk of bleeding. Consequently, blood oozed from the extraction socket continuously and vaseline gauze was packed for hemostasis.
For the further evaluation, contrast enhanced CT and bone scans were performed several days later. Contrast enhanced CT (Lightspeed Ultra, GE Healthcare, Milwaukee, WI, USA) showed an expansile, multilocular osteolytic lesion and multiple fluid levels within the cystic spaces at the right posterior mandibular area (Fig. 1B). A three-phase bone scan was performed after the intravenous injection of 20mCi 99mTc-HDP. The blood-pool and delayed images showed increased radiotracer accumulation in the left mandibular body area (Fig. 1C). The patient wanted to delay the surgery 5 month later.
Five month later, the lesion was re-evaluated. Panoramic radiograph revealed that lesion grew largely and the internal septa showed multilocular soap bubble appearance (Fig. 2A) and contrast enhanced CT showed the similar features compared with the previous CT images but enlarged lesion (Fig. 2B). Femoral artery angiography showed high vascularization of the lesion and the left facial artery as a feeding vessel (Fig. 2C).
Selective embolization using polyvinyl alcohol was performed before the surgery considering her tender age. The day after embolization, the lesion was managed using curettage with lateral decortication and repositioning to the original position with screw fixation under general anesthesia (Fig. 3). Thereby, the continuity of the mandible was maintained that provided stability of the mandibular arch. The bony surgical specimen stained by hematoxylin and eosin confirmed the diagnosis of ABC showing the typical histological pattern (Fig. 4). Post-operative period was uneventful, and no sign of recurrence has been observed for 5.7 years (Fig. 5).
The radiographic and CT features of ABCs are not pathognomonic, and there has been no consensus in the literature in this regard.9 This, in part, might be because of the various histologic types of ABCs; the solid type being more defined and less destructive; the vascular type being less defined and more destructive.10 ABCs vary in the radiographic features manifesting as unicystic, multilocular, or moth eaten, causing expansion, perforation, or extensive destruction of the cortical bone.10-12 Extreme expansion of outer cortical plate is more dramatic in ABCs than in most other lesions.13 Periosteal reaction and pathological fracture of the jaw associated with ABCs were also reported.9-11 The diagnosis of ABC can be challenging due to the untypical radiographic and clinical appearance and misdiagnosis as osteomyelitis was reported.1 In the present case, the lesion showed multilocular honeycomb radiolucency and then changed into soap bubble appearance after five months. Early diagnosis of ABC is important to prevent unexpected bleeding and delay of the treatment. Rapid growth of the swelling with multilocular radiolucency of children should be considered as ABCs.
In ABC, the predominant bone scan pattern is moderate to intense tracer accumulation at the periphery of the lesion with little activity at its center (doughnut sign), a finding that is evident in about 64% of cases.14,15 In the present case, the doughnut sign was observed at the blood-pool phase while the intense, central homogeneous uptake was evident at the delayed phase. The central uptake might be related to the extraction of the deciduous teeth.
Differential diagnosis of the present case included multilocular lesions such as central giant cell granulomas, ameloblastoma, and cherubism. ABCs may expand to a greater degree, and they are more common in the posterior parts of mandible compared with giant cell granulomas. Ameloblastoma usually occurs in the older age group and cherubism is a multifocal bilateral disease.
Regarding the treatment, various methods have been described, including surgery, embolization, cryotherapy, and a wait and see strategy.16,17 To date, surgical curettage or partial resection are the primary choices of the treatment.13 Massive bleeding may occur during operation and multiple bony septa may cause incomplete curettage.10 ABCs have a high recurrence rate and they are usually recurring within the first year after the initial treatment.18 Therefore, surgical resection has been considered as a choice for complete removal of aggressive ABCs.19 In this case, preoperative embolization helped to control bleeding and to minimize the surgical extent. The decortications with repositioning maintained the continuity of mandible, and the inferior alveolar nerve was preserved during curettage. The postoperative result was good aesthetically and functionally. The operative site was healed with normal bony structure, and no additional treatment such as a surgical reconstruction or bone graft was necessary, which was beneficial for young child.
In conclusion, this report presented a case of ABC on the mandibular posterior area treated by conservative surgical curettage with preoperative embolization minimizing the extent of surgery and the surgical complications. Early diagnosis of ABC is very important and it should be treated appropriately considering multiple factors such as age, surgical complication, and possibility of recurrence.
Figures and Tables
Fig. 1
A. Cropped panoramic radiograph reveals multilocular honeycomb appearance with expansion of cortical bone on the left mandibular body area. B. Coronal contrast enhanced CT scan shows an expansile, multilocular osteolytic lesion with multiple internal septation and multiple fluid levels within cystic spaces at the left mandible. C. The blood-pool (left) and delayed phase (right) reveal an increased radiotracer uptake in the left mandibular body area.
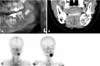
Fig. 2
A. Cropped panoramic radiograph shows that the lesion grows largely and the internal septa show multilocular soap bubble appearance five months later. B. Coronal contrast enhanced CT image shows the similar features compared with the previous CT images but enlarged lesion. C. Pre-embolization angiogram demonstrates a highly vascularized lesion (left). Post-angiogram shows occlusion of the feeder vessel (right).

Fig. 3
The buccal cortex is decorticated (left) and the inferior alveolar nerve is preserved during curettage (right).

References
1. Breuer C, Paul H, Zimmermann A, Braunstein S, Schaper J, Mayatepek E, et al. Mandibular aneurysmal bone cyst in a child misdiagnosed as acute osteomyelitis: a case report and a review of the literature. Eur J Pediatr. 2010. 169:1037–1040.

2. Cottalorda J, Kohler R, Sales de Gauzy J, Chotel F, Mazda K, Lefort G, et al. Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop B. 2004. 13:389–394.

3. Sun ZJ, Sun HL, Yang RL, Zwahlen RA, Zhao YF. Aneurysmal bone cysts of the jaws. Int J Surg Pathol. 2009. 17:311–322.
4. Motamedi MH, Yazdi E. Aneurysmal bone cyst of the jaws: analysis of 11 cases. J Oral Maxillofac Surg. 1994. 52:471–475.
5. Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942. 44:1004–1025.
6. Rosenberg AE, Nielsen GP, Fletcher JA. Fletcher CD, Unni KK, Mertens F, editors. Aneurysmal bone cyst. WHO classification of tumors: pathology and genetics of tumors of soft tissue and bone. 2005. 3rd ed. Lyon: IARC Press;338–339.
7. Jundt G. Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Aneurysmal bone cyst. WHO classification of tumors: pathology and genetics of head and neck tumors. 2005. 3rd ed. Lyon: IARC Press;326.
8. Wang K, Allen L, Fung E, Chan CC, Chan JC, Griffith JF. Bone scintigraphy in common tumors with osteolytic components. Clin Nucl Med. 2005. 30:655–671.

9. Kalantar Motamedi MH. Aneurysmal bone cysts of the jaws: clinicopathological features, radiographic evaluation and treatment analysis of 17 cases. J Craniomaxillofac Surg. 1998. 26:56–62.
10. Motamedi MH, Navi F, Eshkevari PS, Jafari SM, Shams MG, Taheri M, et al. Variable presentations of aneurysmal bone cysts of the jaws: 51 cases treated during a 30-year period. J Oral Maxillofac Surg. 2008. 66:2098–2103.

11. Sun ZJ, Zhao YF, Yang RL, Zwahlen RA. Aneurysmal bone cysts of the jaws: analysis of 17 cases. J Oral Maxillofac Surg. 2010. 68:2122–2128.

12. Motamedi MH. Destructive aneurysmal bone cyst of the mandibular condyle: report of a case and review of the literature. J Oral Maxillofac Surg. 2002. 60:1357–1361.

13. White SC, Pharoah MJ. Oral radiology; principles and interpretation. 2009. 6th ed. St. Louis: Mosby-Year Book Inc;445–446.
15. Seven B, Varoglu E, Alper F, Keles M, Koplay M. Aneurysmal bone cyst of the second metatarsal: three-phase bone scan findings and radiological assessment. Hell J Nucl Med. 2008. 11:189–190.
16. Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg. 2007. 127:105–114.

17. Khambete N, Risbud M, Mehta N. Interventional radiography in management of high-flow arteriovenous malformation of maxilla: report of a case. Imaging Sci Dent. 2011. 41:123–128.

18. Struthers PJ, Shear M. Aneurysmal bone cyst of the jaws. (I). Clinicopathological features. Int J Oral Surg. 1984. 13:85–91.
19. Cottalorda J, Bourelle S. Current treatments of primary aneurismal bone cysts. J Pediatr Orthop B. 2006. 15:155–167.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download