Abstract
Purpose
This study was to find the computed tomographic features of fibrous dysplasia of the maxillofacial region.
Materials and Methods
All eight cases included in the study reported either to Government Dental College and Hospital or Nair Hospital Dental College, Mumbai between 2003 and 2009. The patients were prescribed computed tomogram in addition to conventional radiographs of maxillofacial region which were studied for characteristic features of fibrous dysplasia. The diagnosis of fibrous dysplasia was confirmed by histopathological report.
Results
All cases showed the ill-defined margins of lesions except in the region where the lesions were extending to cortex of the involved bone. Internal structure of all cases showed ground glass appearance. Four cases of maxillary lesion showed the displacement of maxillary sinus maintaining the shape of maxillary sinus. Two cases showed complete obliteration of maxillary sinus. Displacement of inferior alveolar canal did not follow any typical pattern in any of the cases but was displaced in different directions.
Fibrous dysplasia is an uncommon but important lesion affecting the maxillofacial region because it can cause severe deformity and asymmetry of face and jaw bones. Fibrous dysplasia is a genetically-based sporadic disease of the bone; with mutations in the gene (GNAS I).1 Fibrous dysplasia results from a localized change in normal bone metabolism that results in the replacement of all the components of cancellous bone by fibrous tissue containing varying amounts of abnormal appearing bone.2
Fibrous dysplasia is mainly divided into two forms, monostotic (single bone involvement) and polyostotic (multiple bone involvement) forms. Polyostotic form is further divided into Jaffe's type and McCune Albright syndrome. In Jaffe-Litchenstein type, variable number of bones plus pigmented lesion of skin 'café au lait' spots are seen. McCune-Albright syndrome is a severe form involving nearly all the bones with pigmented lesions, and endocrine disorder.3 Another type identified by Daves and Yardley is craniofacial fibrous dysplasia which involves two or more facial and cranial bones.4 Eversole et al reported that the monostotic type occurred in 74% polyostotic type in 13% and craniofacial type in 13%.5
Fibrous dysplasia can be investigated by conventional radiography, computed tomography (CT), scintigraphy, and histopathology. Fibrous dysplasia shows various radiographic findings according to the degree of maturation which determines the degree of opacification. Various appearances described on conventional radiographs are radiolucency, ground-glass, smoky, cloudy, peau d'orange, finger print, or diffuse sclerosis,2,6-8 however CT features has not widely reported. Therefore, this study was undertaken to document and report the various CT appearances of fibrous dysplasia.
Eight cases of fibrous dysplasia which reported either to Government Dental College and Hospital or Nair Hospital Dental College, Mumbai from 2003-2009 were included in the study. The diagnosis of fibrous dysplasia was confirmed on the basis of radiologic and histological findings.
A thorough history of the cases was taken followed by radiographic examinations including initial conventional radiography and followed by CT. The lesions were studied clinically with respect to the sex and age of the patient, the related complaint of the patients, and the jaw involvement with regards to maxilla, mandible (single or both), and sides (left or right or both).
The soft tissue and bone windows of the CT images were examined for the lesions. The CT images were studied to evaluate the correlation between the clinical findings and the extent of involvement of the various facial bones. The anatomical extension of the lesions was also assessed. The lesions were studied on the axial, coronal, and sagittal CT images, and the extent, borders, internal structure of the lesions, and its effect on the adjacent structures were noted.
Out of 8 patients in our study male (4) and female (4) were equal in number. All the cases were unilaterally affected and right side (6) was more commonly affected than left side (2). The age ranged from 12 to 27 years, with average age 18.3 years (Table 1).
All the reported cases were either of monostotic form or craniofacial form (involving cranial bones and facial bones). The involved bones were maxilla, mandible, sphenoid, temporal, zygomatic, and frontal bone (Table 2). Only 3 cases showed involvement of cranial bones along with facial bones (Figs. 1A and B). Maxilla (4 cases) was most commonly involved followed by the mandible (2 cases). In two cases, both maxilla and mandible were involved. The anatomical extensions of the lesions are shown in Table 3.
Two cases of the lesions involving the mandible showed ill-defined margin (Fig. 2) whereas other lesions were extending and merging into the cortex of the involved bone (Table 4).
The internal structure of the involved bone showed increased density of bone. Internal structure was found to be more homogenous in the maxilla than in the mandible. All 8 cases showed the characteristic ground glass appearance (Fig. 3, Table 4).
Regarding the effect on surrounding structures (Table 2), all cases showed bucco-lingual expansion causing cortical thinning of the involved bone. The lesions caused a displacement of adjacent structures such as inferior alveolar canal, maxillary sinus, and floor of orbit.
In 6 cases of maxillary involvement, the lesions displaced the maxillary sinus, however the shape of sinus was maintained (Fig. 4). Maxillary sinus in two cases and sphenoid sinus in one case showed complete obliteration (Figs. 5A and B). The floor of orbit was raised in only two cases where the maxilla was involved. All 4 cases involving mandible showed a displacement of the inferior alveolar canal in all directions (Figs. 6A and B).
Loss of lamina dura was noted in all cases around the teeth in the affected bone. Only 3 cases showed a displacement of the tooth and two cases were associated with impacted teeth, however none showed any evidence of root resorption.
Fibrous dysplasia is encountered in younger age group with no specific sex predilection.5-7 The craniofacial type of fibrous dysplasia is found to be as common as fibrous dysplasia of the jaw and was more commonly seen in younger age. The unilateral nature of fibrous dysplasia was noted in all cases. The most commonly involved cranial bones were maxilla and frontal bones (Fig. 1). When the maxilla was affected, other adjacent bones separated by sutures such as zygomatic, sphenoid, frontal, and nasal bones might also get affected.9 This study showed that the right side was more commonly involved than the left, which was similar to the findings of previous studies.10
Eversole et al5 suggested that the ill-defined margin of the lesion helped to differentiate it from other fibro-osseous lesions. In this study, the margins were ill-defined except in the region where they extended to the cortex of bone. Ground glass appearance was the most common radiographic appearance of internal structure of fibrous dysplasia in the present study, which was substantiated the diagnosis of fibrous dysplasia.10 Fibrous dysplasia shows bucco-lingual expansion causing thinning of the cortical plate. The expansion of the external surface of the affected bone assumed a grosser but still recognizable anatomical shape.6 The lesion displaced the inferior alveolar canal in all four directions (buccal, lingual, superior, and inferior). The displacement was in contrast with the finding of Petrikowski11 who suggested that the upward displacement of inferior dental canal was a unique characteristic of fibrous dysplasia. However, the displacement of the canal in various directions might be explained by the location of epicenter in relation to the canal. For example if the epicenter was superior to the inferior alveolar canal, it would displace the canal inferiorly.
The lesion involving maxilla showed expansion on the external surface and on internal surface into maxillary sinus. The expansion of maxilla reduced the size of maxillary sinus cavity although the shape seemed unaltered. This unique finding could help in differentiating fibrous dysplasia from other tumors such as ossifying fibroma.6 Fibrous dysplasia might also completely obliterate maxillary sinus and displace the floor of orbit.
Lamina dura was lost in all teeth which were involved in the lesion; this might be corroborated by the fact that the loss of lamina dura was unique to fibrous dysplasia and could be used as an ancillary diagnostic feature for fibrous dysplasia.11 The impacted teeth which were noted in two cases may be caused by increased density of bone in the path of eruption. Although the lesion displaced the teeth without resorption, the displacement was found to be minimal. The minimal displacement of teeth such as inclination and rotation was noted but no bucco-lingual displacement similar to a study by Akintoye et al.12
The features of fibrous dysplasia such as the margins, internal structure, and effect on surrounding structure were well characterized on CT images. The margins of lesion, ground glass appearance, and displacement of maxillary sinus were characteristic and consistent with the findings of fibrous dysplasia. Although no single radiographic feature is pathognomic of fibrous dysplasia, all the features together could be considered to be diagnostic of fibrous dysplasia.
Figures and Tables
Fig. 1
CT images of fibrous dysplasia. A. Coronal section shows craniofacial type of fibrous dysplasia with involvement 1. frontal, temporal, 2. zygomatic, 3. maxilla, and 4. mandible. B. Another coronal section shows maxillofacial type with involvement of 1. maxilla and 2. zygomatic bone.

Fig. 2
Axial CT image shows ill-defined margin (white arrow) except in region where lesion is extending to the cortex (black double arrow).
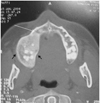
Fig. 3
Coronal CT image shows lesion involving maxilla with increased density of maxilla giving ground glass appearance (black arrow).

Fig. 4
Coronal CT image shows maxillary sinus occupied with lesion. Note: the size is reduced but the shape of maxillary sinus is maintained (black arrow).

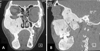
Fig. 5
CT images. A. Coronal section shows obliteration of 1. maxillary sinus. B. Oblique section shows complete obliteration of 1. maxillary and 2. sphenoid sinus.
References
1. Bastepe M. The GNAS Locus: quintessential complex gene encoding Gsalpha, XLalphas, and other imprinted transcripts. Curr Genomics. 2007. 8:398–414.
2. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 2004. 5th ed. St. Louis: Mosby-Year Book Inc;485–491.
3. Waldron CA. Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Bone pathology. Oral and maxillofacial pathology. 1995. Philadelphia: WB Saunders;461–465.
5. Eversole LR, Sabes WR, Rovin S. Fibrous dysplasia: a nosologic problem in the diagnosis of fibro-osseous lesions of the jaws. J Oral Pathol. 1972. 1:189–220.

6. MacDonald-Jankowski DS, Yeung R, Li TK, Lee KM. Computed tomography of fibrous dysplasia. Dentomaxillofac Radiol. 2004. 33:114–118.

7. Ricalde P, Horswell BB. Craniofacial fibrous dysplasia of the fronto-orbital region: a case series and literature review. J Oral Maxillofac Surg. 2001. 59:157–167.

8. Jacobsson S, Hallén O, Hollender L, Hansson CG, Lindström J. Fibro-osseous lesion of the mandible mimicking chronic osteomyelitis. Oral Surg Oral Med Oral Pathol. 1975. 40:433–444.

9. Posnick JC. Fibrous dysplasia of the craniomaxillofacial region: current clinical perspectives. Br J Oral Maxillofac Surg. 1998. 36:264–273.

10. MacDonald-Jankowski D. Fibrous dysplasia in the jaws of a Hong-Kong population: radiographic presentation and systematic review. Dentomaxillofac Radiol. 1999. 28:195–202.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download