Abstract
Primary retroperitoneal squamous cell carcinoma is very rare. A 66-year-old woman presented with right leg edema and pain that had developed one month prior. Pelvis magnetic resonance imaging showed the presence of a mass around the iliac vessels invading the iliacus muscle, right femoral head and obturator muscle. The patient underwent an exploratory laparotomy but the mass was not completely removed. The patient was treated with concurrent chemoradiation therapy with paclitaxel-carboplatin and Tomotherapy three weeks after surgery. After that, she conducted a further seven cycles of different chemotherapy. A abdomen CT scan after the last seven cycles showed a reduction in the size of the primary mass from 7.2 to 6.6 cm, consistent with a partial response to treatment. As a result, the role of adjuvant chemotherapy in these tumors is controversial. And it is considered that complete resection is more important.
Primary retroperitoneal tumors are defined as solid or cystic tumors, whether benign or malignant, that develop in the retroperitoneal space and arise from lymphatic, nervous, vascular, support muscle, connective, or fibroareolar tissue independent of the organs and large vessels in the space [1,2]. Primary retroperitoneal neoplasms account for only 0.1%-0.2% of all malignancies [3]. About 80%-86% of retroperitoneal tumors are malignant. And most primary retroperitoneal neoplasms are lymphomas, liposarcomas, leiomyosarcomas and malignant histiofibromas [3,4]. Whereas Epithelial cancer of the retroperitoneum is extremely rare, with only a few cases having been reported [5]. We present a case of a primary squamous cell carcinoma (SCC) of the pelvic retroperitoneum which to our knowledge has been rarely described.
A 66-year-old woman, gravida 4, para 2, visited our hospital with right leg edema and right inguinal pain that had developed one month prior. The patient had a past medical history of hypertension and the patient had taken medication three years prior. Duplex color Doppler ultrasound did not demonstrate the presence of a thrombus or a Baker's cyst. Gynecologic ultrasound was undertaken for the evaluation of a pelvic mass and 5.4 × 3.1 cm sized pelvic mass was discovered on the right side pelvic wall apart from the uterus and ovary. Pelvis magnetic resonance imaging (MRI) showed the presence of a 7.2 cm sized lobulating contoured, heterogeneous enhanced mass in the right pelvic cavity which suggested the presence of a retroperitoneal soft tissue tumor, such as a sarcoma or malignant nerve sheath tumor (Fig. 1). A Pap smear, chest X-ray, gastroscopy, and colonoscopy were normal. Tumor markers are normal except SCC antigen which was elevated to 10.47 ng/mL (N, 0-1.5 ng/mL).
The patient underwent an exploratory laparotomy. There was a 7×5 cm sized retroperitoneal hard mass fixed to the right pelvic wall compressing the external iliac artery and vein. The inner portion of the mass was necrotic and the mass was attached tightly to the iliac vessels. There was no lesion on the uterus, ovary and upper abdominal organs. It was impossible to remove the total mass completely for the risk of great vessel injury and a frozen biopsy suggested the presence of a squamous cell carcinoma (Fig. 2). Because the 18F-fluorodeoxyglucose positron emission tomography scanning (18F-FDG PET/CT) scan that was obtained 2 days after the operation revealed no uptake elsewhere and pelvic retroperitoneum was determined as the primary site (Fig. 3). The patient underwent concurrent chemoradiatiotherapy (CCRT) treatment with the use of paclitaxel-carboplatin and Tomotherapy three weeks after surgery. Paclitaxel (135 mg/m2 over 3 hours on day 1) and carboplatin (350 mg/m2 on day 1) were administered every three weeks.
Three months after completing CCRT, SCC antigen level decreased to 0.33 ng/mL (N, 0-1.5 ng/mL). An abdomen CT scan that was obtained 3 months after the CCRT revealed the total mass size was decreased (right pelvic wall mass, 7.2-6.6 cm) and the inner necrotic portion was increased and metastatic mass on iliac artery was decreased (2.6-1.1 cm). The patient is well tolerated and right leg edema is improved. After the CCRT, partial response was achieved. For that reason, she received further three cycles of chemotherapy with paclitaxel (175 mg/m2, day 1) and carboplatin (350 mg/m2, day 1). According to the CT, they were confirmed to be the remnant tumor mass around the right pelvic wall and iliac artery. In addition to these treatments, she underwent four cycles of combination chemotherapy with cisplatin (80 mg/m2, day 1) and 5-fluorouracil (1,000 mg/m2, from day 1 to 4). Three weeks after completion of the chemotheraphy, there is no change in the abdomen CT scan. And SCC was within the normal range. The patient refused the above management. Neither a primary lesion nor any signs of recurrence were demonstrated for four years after the operation. To date, the patient has been followed with no evidence of recurrence.
Retroperitoneal neoplasms are rare and comprise a diverse group tumors. To our knowledge, only a few similar cases have been reported (Table 1). Primary retroperitoneal tumors arise in the retroperitoneal space independently of any organ. Secondary retroperitoneal tumors occur by direct extension of any adjacent malignancy or by metastases of malignancies from any tumor in the body [9]. For retroperitoneal tumors, malignant tumors are more frequent than benign tumors and a lymphoma is the most common malignant tumor. Other possible retroperitoneal tumors are germ cell tumors, metastatic carcinomas and soft tissue sarcomas [5]. The most common type of vascular involvement of a retroperitoneal tumor is for the vein only, and both artery and vein involvement is the most infrequent type [10]. Primary retroperitoneal tumors also include tumors caused by embryonic rests of the urogenital ridge (wolffian or mullerian ducts, germ cells) and the primitive notochord and those arising from the neural crest, such as paragangliomas in the organ of Zuckerkandl or at other sites, and retroperitoneal extra-adrenal neuroblastomas [11,12].
Late diagnosis of primary retroperitoneal tumors is common because the retroperitoneum space is adaptable and the tumors remain asymptomatic for some time [11]. MRI, in this case is very useful. The main advantage of MRI is that the tumor can be studied in all planes of the space. And theses image provides a preoperative interpretation of the anatomy, structure and vascularization of the tumor.
The importance of the complete resection is directly related to the possibility of survival [13]. But the rate of complete radical resection has been reported as only 44.5% in some studies, although reconstruction of the iliac vessels might be required [14]. Due to the rarity and poor prognosis of primary retroperitoneal tumors, there is no well-established treatment. One-year survival rates of retroperitoneal sarcomas and lymphomas are approximately 80% and 67%, respectively, whereas one-year survival rates of undifferentiated tumors and carcinomas are less than 33% [15]. In previous reports similar to our case, chemotherapy with cisplatin and 5-fluorouracil, irrinotecan and cisplatin, paclitaxel and carboplatin or gemcitabine were not effective [8]. In our case, the patient underwent the similar chemotheraphy. However, tumor mass still remains.
We have presented a case of a primary SCC arising from the retroperitoneum that was treated with surgery and adjuvant CCRT with paclitaxel-carboplatin and chemotheraphy. It is difficult to establish the standard treatment of retroperitoneal squamous cell carcinoma for the poor prognosis. In our experience, the role of adjuvant chemotherapy in these tumors is controversial. Complete surgical resection, if possible, is associated with the best prognosis for primary retroperitoneal SCC.
Figures and Tables
Fig. 1
Magnetic resonance imaging showed the presence of a heterogeneous mass with an ill-defined margin that measured 7.2 cm. Focal calcification that infiltrated the iliacus muscle, femoral head and obturator muscle was observed.
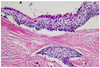
Fig. 2
Microscopic findings of the tumor are shown. A squamous cell carcinoma with intercellular bridges and island infiltrating fibrous tissue is seen (H&E, ×200).
References
1. Martínez-Piñeiro JA, Pérez-Castro Ellendt E, Hernández Armero A, Cisneros Ledo J, Avellana Fontanella JA. Primary retroperitoneal tumors. Apropos of 11 cases. Arch Esp Urol. 1983. 36:97–108.
2. González Cajigal R, Martín Duce A, Moreno González-Bueno C. Primary retroperitoneal tumors. Rev Esp Enferm Apar Dig. 1988. 73:580–584.
3. Armstrong JR, Cohn I Jr. Primary malignant retroperitoneal tumors. Am J Surg. 1965. 110:937–943.
4. Pack GT, Tabah EJ. Primary retroperitoneal tumors: a study of 120 cases. Int Abstr Surg. 1954. 99:209–231.
5. Pal DK, Chakraborty S, Das S. Retroperitoneal tumours: a ten years retrospective study. J Indian Med Assoc. 2005. 103:18–20.
6. Shimura H, Mihara A, Miyahara H. Statastics of 43 cases of retroperitoneal tumors and the prognosis. J Clin Surg. 1964. 26:429–435.
7. Liu X, Saiki N, Kohno A, Fujioka M, Hirabayashi K, Komori T, et al. Retroperitoneal squamous cell carcinoma: metastasis from uterine endometrial carcinoma? Radiat Med. 2000. 18:267–271.
8. Khalil AM, Shabb NS, Hourani MH, Shamseddine AI, El-Hajj MI, Seoud AF. Primary squamous cell carcinoma of the pelvic retroperitoneum presenting as an adnexal mass: a case report. J Obstet Gynaecol. 2005. 25:92–93.
9. Duncan RE, Evans AT. Diagnosis of primary retroperitoneal tumors. J Urol. 1977. 117:19–23.
10. Schwarzbach MH, Hormann Y, Hinz U, Leowardi C, Böckler D, Mechtersheimer G, et al. Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement. J Vasc Surg. 2006. 44:46–55.
11. Tambo M, Fujimoto K, Miyake M, Hoshiyama F, Matsushita C, Hirao Y. Clinicopathological review of 46 primary retroperitoneal tumors. Int J Urol. 2007. 14:785–788.
12. An JY, Heo JS, Noh JH, Sohn TS, Nam SJ, Choi SH, et al. Primary malignant retroperitoneal tumors: analysis of a single institutional experience. Eur J Surg Oncol. 2007. 33:376–382.
13. Boneschi M, Erba M, Cusmai F, Eusebio D, Miani S, Bortolani EM. Primary retroperitoneal tumors. Treatment modality and prognostic factors. Minerva Chir. 1999. 54:763–768.
14. Chen F, Yang Y, Shi Z, Fu W, Jiang J. Resection of pelvic retroperitoneal neoplasm and reconstruction of iliac blood vessels: report of 22 cases. Zhonghua Wai Ke Za Zhi. 2000. 38:858–860.
15. Pinson CW, ReMine SG, Fletcher WS, Braasch JW. Long-term results with primary retroperitoneal tumors. Arch Surg. 1989. 124:1168–1173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download