Abstract
Actinomyces normally colonizes the mouth, colon, and vagina. Although disruption of mucosa may lead to infection at virtually any site, central nervous system actinomycosis is rare. A 45-year-old man presented with seizure and magnetic resonance imaging showed brain abscess. He was diagnosed with actinomycotic and streptococcal infection of brain by histologic and microbiologic examination. After stereotactic aspiration and biopsy, he was treated successfully by prolonged antibiotic therapy using intravenous penicillin-G and oral amoxicillin.
Figures and Tables
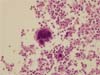
Figure 1
Initial magnetic resonance imaging. (A) 2.2×1.8cm sized mass lesion, iso-signal intensity on T1 weighted image and (B) peripheral low signal intensity on T2 weighted image with peripheral enhancement on right frontal lobe with internal non-enhancing necrotic portion is observed.

References
2. Puzzilli F, Salvati M, Bristot R, Bastianello S, Ruggeri A, Lunardi P. Actinomycosis of the central nervous system: surgical treatment of three cases. J Neurosurg Sci. 1998. 42:165–171.
3. Mandell GL, Bennett JE, Dolin R. Mandell, Douglas and Bennett's principles and practice of infectious diseases. 2005. 6th ed. New York: Churchill Livingstone;2924–2931.
4. Sudhakar SS, Ross JJ. Short-term treatment of actinomycosis: two cases and a review. Clin Infect Dis. 2004. 38:444–447.

5. Song EH, Kwon HH, Jang EY, Kim MN, Lee SO, Kim YS, Woo JH. A case of brain abscess caused by Actinomyces meyeri and Haemophilus aphrophilus. Korean J Med. 2008. 74:Suppl 1. 144–148.
6. Maltby GL. Intracranial actinomycosis; report of an unusual case. J Neurosurg. 1951. 8:674–678.
7. Bolton CF, Ashenhurst EM. Actinomycosis of the Brain; Case Report and Review of the Literature. Can Med Assoc J. 1964. 90:922–928.
9. Chatwani A, Amin-Hanjani S. Incidence of actinomycosis associated with intrauterine devices. J Reprod Med. 1994. 39:585–587.
10. Schaal KP, Lee HJ. Actinomycete infections in humans--a review. Gene. 1992. 115:201–211.
11. Roberts JA, Paratz J, Paratz E, Krueger WA, Lipman J. Continuous infusion of beta-lactam antibiotics in severe infections: a review of its role. Int J Antimicrob Agents. 2007. 30:11–18.

12. Roberts JA, Webb S, Paterson D, Ho KM, Lipman J. A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med. 2009. 37:2071–2078.

13. Chaudhry SI, Greenspan JS. Actinomycosis in HIV infection: a review of a rare complication. Int J STD AIDS. 2000. 11:349–355.

14. Adeyemi OA, Gottardi-Littell N, Muro K, Kane K, Flaherty JP. Multiple brain abscesses due to Actinomyces species. Clin Neurol Neurosurg. 2008. 110:847–849.

15. de Louvois J, Gortavai P, Hurley R. Bacteriology of abscesses of the central nervous system: a multicentre prospective study. Br Med J. 1977. 2:981–984.

16. Lewin W, Morgan AD. Actinomycosis of the brain. J Neurol Neurosurg Psychiatry. 1947. 10:163–170.

17. Dailey AT, LeRoux PD, Grady MS. Resolution of an actinomycotic abscess with nonsurgical treatment: case report. Neurosurgery. 1993. 32:134–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download