Abstract
Disseminated tuberculosis occurs through lymphohematogenous dissemination of Mycobacterium tuberculosis bacilli. The exact incidence of disseminated tuberculosis is still unknown and its diagnosis presents a challenge since the symptoms are not specific of the disease. Brain tuberculoma is one of the complications of tuberculosis. The literary review of brain tuberculoma shows that it mainly occurs in the cerebrum and cerebellum, whereas involvement of the brainstem is rare. Recently, we have experienced a case of 46-year-old man with fever of 2 months duration who was diagnosed with disseminated tuberculosis with miliary central nervous system (CNS) tuberculomas; brain tuberculomas were found even in the brainstem and the spinal cord. Pulmonary, intestinal, renal, and choroidal involvements were also noted.
The approach to fever of unknown origin (FUO) is challenging. Through workup and penetrating assessments should be done on the patient to locate the fever focus. Several researches prove that infectious disease still is the most common cause of FUO (1-3). Among the infectious diseases, tuberculosis should always be considered as a possibility, especially in endemic areas. However, physicians often do not consider tuberculosis as a cause of FUO if symptoms are nonspecific and chest radiograph is normal.
Disseminated tuberculosis is defined as tuberculous infection involving the blood stream, bone marrow, liver, ≥ 2 noncontiguous sites, or miliary tuberculosis (4). It is due to lymphohematogenous dissemination of Mycobacterium tuberculosis bacilli.
Herein, we report a case of 46-year-old man with fever of 2 months duration who finally was diagnosed with disseminated tuberculosis with miliary CNS (central nervous system) tuberculoma; pulmonary, intestinal, renal, and choroidal involvements were also noted.
A 46-year-old, previously healthy man was referred to Korea University Guro Hospital in July 2007 with fever and fatigue of 2 months' duration; the cause of fever could not be detected despite 3 weeks' evaluation in the referral hospital. He had no past history of having suffered from tuberculosis or other infectious, metabolic diseases, and had no family history of tuberculosis or other diseases. He was a street vendor and his socioeconomic status was low. He had been drinking about 120 grams of alcohol daily for the past 25 years. He complained of fever, fatigue, and weight loss of 20 kilograms during the last 2 months.
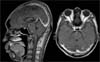
On admission, his vital signs were as follows: blood pressure, 90/60 mmHg; heart rate, 100 beat/min; respiratory rate, 20 beat/min; and body temperature, 39.4℃. On physical examination, hepatosplenomegaly was observed. Liver was firm and palpable, 3 finger-breadths below the costal margin. Laboratory tests were as follows: hemoglobin level, 10.1 g/dL; white blood cell count, 4,100/µL; platelet, 61,000/µL; asparate aminotransferase (AST), 170 IU/L; alanin aminotransferase (ALT), 104 IU/L; r-glutamyl transpeptidase (r-GTP), 125 IU/L; alkaline phosphatase (ALP), 621 IU/L; blood urea nitrogen, 28.3 mg/dL; creatinine, 1.5 mg/dL; and urine WBC, 30-60/HPF. The peripheral blood (PB) smear showed pancytopenia and microcytic normochromic anemia with anisopoikilocytosis. The antigen and antibody of human immunodeficiency virus (HIV) were not detected. Initial chest radiographic findings were unremarkable, but miliary lung nodules appeared on the 4th hospital day (Fig. 1). The computed tomography (CT) scan of abdomen showed hepatosplenomegaly. On the 4th hospital day, his personality changed and became aggressive, suffered mood swings, and complained of sleep disturbance. Magnetic resonance imaging (MRI) of the brain was taken, and it revealed numerous diffuse small nodular or ring enhanced lesions in the cerebrum, cerebellum, brainstem, and upper cervical spinal cord (Fig. 2). Bone scan showed flared appearance on the sternum, and colonoscopy revealed terminal ileitis. Acid-fast bacilli (AFB) were found in urine and cerebrospinal fluid (CSF) by Ziehl-Neelsen stain. The results of polymerase chain reaction for the detection of Mycobacterium tuberculosis (TB-PCR) were positive in urine, sputum, CSF, and ileocecal tissue. Mycobacterium tuberculosis was cultured from sputum and CSF. On ophthalmologic examination, choroidal tuberculomas were also found (Fig 3).
Anti-tuberculosis medications were prescribed: isoniazid, rifampin, pyrazinamide, and ethambutol. Corticosteroid was also used for tuberculous meningitis with brain tuberculoma. Dexamethasone was given intravenously starting with the dose of 0.2 mg/kg and tapered over 17 days. Afterwards, it was switched to oral dexamethasone 4 mg for the first following week, changed to prednisolone 15 mg for the next week, followed by prednisolone 7.5 mg for 2 weeks and finally to prednisolone 5 mg for 45 days. Total duration of corticosteroid use was 13 weeks and total amount of corticosteroid was equal to 235.3 mg of dexamethasone. Throughout the treatment, fever subsided, and his personality became normal. Elevated liver enzyme and thrombocytopenia also normalized. He was discharged without further complication and remained asymptomatic during six months follow-up.
Literary review shows that infectious disease is the leading cause of FUO (1-3). Among them, tuberculosis is the most common infectious cause of FUO in endemic areas. Researches have shown that tuberculosis is responsible for 23% of all causes of FUO in Taiwan (1), and 24% in Turkey (2). In Korea, tuberculosis is responsible for 21.6% of causes of FUO in one research and 11.7% in the other research placing it as the most common infectious cause (5, 6).
Exact incidence of disseminated tuberculosis is not known. Since the symptoms are nonspecific, high index of suspicion is necessary to reach the diagnosis. Arnow and Flaherty reported that the most common forms of tuberculosis, which present as FUO, were disseminated disease without the miliary pattern on chest radiograph or extrapulmonary disease without clear localizing features (7). Likewise, Wang et al. also reported that the patients group whose diagnoses were delayed had the lowest rate of miliary pattern on chest radiograph (4). The initial lack of clues for diagnosis brings on little suspicion of each disease entity, and leads to delayed diagnosis or misdiagnosis. Initially in this case, the patient had no respiratory symptoms and his chest radiograph was clear. Moreover, he did not have previous tuberculosis history, which might make physicians to overlook the possibility of having tuberculosis. In the endemic areas of tuberculosis, it is important to screen for tuberculosis and take follow-up chest radiograph serially in approach to FUO patients.
In this case, pulmonary, renal, intestinal, and CNS involvements of tuberculosis were demonstrated by the results of TB-PCR and culture. Brain MRI showed brain tuberculoma which is an uncommon manifestation of tuberculosis. Brain tuberculomas are due to hematogenous spread of tubercle bacilli. Tuberculomas usually occur in the cerebral and cerebellar hemispheres because of their high vascular supply, and brainstem tuberculoma is rare (8, 9). In this case, however, brain tuberculomas were found even in the brainstem and spinal cord. This could signify the presence of a large infectious burden. The levels of ALP and r-GTP were elevated initially and decreased after anti-tuberculous treatment. Abdominal CT scan at the time of admission showed hepatosplenomegaly, reflecting hepatosplenic involvement. In addition, bone marrow involvement is also a possibility which could explain pancytopenia and findings observed in the bone scan. Pancytopenia was recovered after initiation of anti-tuberculous drugs. Choroidal involvement was also observed. The choroid is the commonly affected site and choroidal tuberculosis suggests direct hematogenous infecton (10).
Disseminated tuberculosis occurs because of inadequate host defense in containing tuberculous infection, especially due to impaired cell-mediated immunity (11). In this case, the patient was a malnourished chronic alcoholic, drinking 120 g of alcohol daily for the past 25 years. Heavy alcohol intake and malnutrition, which are known as conditions related to mycobacteriosis-associated FUO, might have contributed to the immunologic silence in this case (1). Both alcohol intake and malnutrition are important causes of impaired cell-mediated immunity; mitogen-blocking factor in alcoholics and leptin deficiency in malnourished patients are associated (12, 13).
Corticosteroid is commonly used in the treatment of tuberculous meningitis along with anti-tuberculous drugs. Corticosteroids help reduce swelling and congestion of the meninges, and thus decrease pressure inside the brain and the attendant risk of death or disabling residual neurological deficit among survivors (14). The adjunctive treatment with dexamethasone improved survival in patients over 14 years of age with tuberculous meningitis in the literature (15). Standard therapeutic guideline on corticosteroid for tuberculous meningitis does not exist, but in one literature, dexamethasone (for adults 12 to 16 mg/day for three weeks, tapered over the next three weeks) or prednisolone (for adults 60 mg/day for three weeks and tapered over the next three weeks) is recommended (14). In the other research, patients with a score on the Glasgow Coma Scale of 14 or less, such as our patient, received intravenous dexamethasone treatment for four weeks (0.4 mg/kg/day for the first week and decreasing by 0.1 mg/kg/day for each following week) and followed by oral treatment for four weeks, starting at a total dose of 4 mg/day and decreasing by 1mg each week (15). In this case, we used dexamethasone intravenously starting at 0.2 mg/kg and tapered over 17 days. Afterwards, oral therapy was maintained for about 10 weeks. As described above, total duration of corticosteroid use was 13 weeks and the total amount of corticosteroid was equal to 235.3 mg of dexamethasone.
The mortality from disseminated tuberculosis is most often due to delayed diagnosis and treatment. Timing of anti-tuberculosis treatment is known as one of the independent prognostic factors of disseminated tuberculosis (4). In the setting of relative immunologic silence, high index of suspicion and prompt treatment are important. Therefore, physicians could carefully consider starting anti-tuberculous medication as a clinical trial to the patients with FUO without localized infection sign, especially in endemic areas of tuberculosis.
Figures and Tables
References
1. Chin C, Lee SS, Chen YS, Wann SR, Lin HH, Lin WR, Huang CK, Kao CH, Yen MY, Liu YC. Mycobacteriosis in patients with fever of unknown origin. J Microbiol Immunol Infect. 2003. 36:248–253.
2. Tabak F, Mert A, Celik AD, Ozaras R, Altiparmak MR, Ozturk R, Aktuglu Y. Fever of unknown origin in Turkey. Infection. 2003. 31:417–420.
3. Colpan A, Onguru P, Erbay A, Akinci E, Cevik MA, Eren SS, Bodur H. Fever of unknown origin: analysis of 71 consecutive cases. Am J Med Sci. 2007. 334:92–96.

4. Wang JY, Hsueh PR, Wang SK, Jan IS, Lee LN, Liaw YS, Yang PC, Luh KT. Disseminated tuberculosis: a 10-year experience in a medical center. Medicine (Baltimore). 2007. 86:39–46.
5. Kim YK, Kim MS, Lee KS, Huh AJ, Yeom JS, Hong SK, Chang KH, Song YG, Kim JM. A comparison of causes of fever of unknown origin between the 1980s and the 1990s. Korean J Med. 2001. 61:546–552.
6. Kee SY, Jo YM, Kim JY, Choi WS, Jeong HW, Jung SJ, Kim SB, Hyun JJ, Hwang BY, Cheong HJ, Kim WJ. Etiology of Adult Patients with Fever of Unknown Origin (FUO) Observed in A University Hospital in Korea from 1998-2003. Infect Chemother. 2005. 37:127–132.
8. Guzel A, Tatli M, Aluclu U, Yalcin K. Intracranial multiple tuberculomas: 2 unusual cases. Surg Neurol. 2005. 64:Suppl 2. S109–S112.

9. Idris MN, Sokrab TE, Arbab MA, Ahmed AE, El Rasoul H, Ali S, Elzubair MA, Mirgani SM. Tuberculoma of the brain: a series of 16 cases treated with anti-tuberculosis drugs. Int J Tuberc Lung Dis. 2007. 11:91–95.
10. Varma D, Anand S, Reddy AR, Das A, Watson JP, Currie DC, Sutcliffe I, Backhouse OC. Tuberculosis: an under-diagnosed aetiological agent in uveitis with an effective treatment. Eye. 2006. 20:1068–1073.

11. Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med. 2000. 161:1376–1395.
12. Rodrguez L, Graniel J, Ortiz R. Effect of leptin on activation and cytokine synthesis in peripheral blood lymphocytes of malnourished infected children. Clin Exp Immunol. 2007. 148:478–485.

13. Pavia CS, La Mothe M, Kavanagh M. Influence of alcohol on antimicrobial immunity. Biomed Pharmacother. 2004. 58:84–89.

14. Prasad K, Singh MB. Corticosteroids for managing tuberculous meningitis. Cochrane Database Syst Rev. 2008. 23:CD002244.

15. Thwaites GE, Nguyen DB, Nguyen HD, Hoang TQ, Do TT, Nguyen TC, Nguyen QH, Nguyen TT, Nguyen NH, Nguyen TN, Nguyen NL, Nguyen HD, Vu NT, Cao HH, Tran TH, Pham PM, Nguyen TD, Stepniewska K, White NJ, Tran TH, Farrar JJ. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004. 351:1741–1751.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download