Abstract
Cervical epidural abscess (CEA) is a very uncommon disease with diverse clinical presentations. Clinically, it is difficult to diagnose this disease, especially in early stage. We report an atypical case of CEA showing only progressive quadriparesis without any other symptoms or signs of CEA. From this experience, CEA must be considered when progressive quadriparesis without any specific cause is developed in immuno-compromised patients and diabetic patients with polyneuropathies.
Cervical epidural abscess (CEA) is an uncommon disease with diverse clinical presentations. Clinically, it is difficult to diagnose this disease, especially in early stage (1). Early diagnosis of CEA became more frequent with recent development of diagnostic radiology (2). Considering that CEA can cause permanent neurologic deficits if early surgical treatment is not performed (3), the importance of early diagnosis of CEA can not be emphasized enough. Therefore, if a patient shows fever, back pain, and progressive neurologic deficits such as quadriparesis, sphincter dysfunction, and a detectable sensory level, we must consider CEA as the underlying disease (1, 4). We report an atypical case of CEA showing only progressive quadriparesis without any other symptoms or signs of CEA.
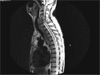
A 71-year-old male with chronic renal failure and diabetes mellitus was admitted for hemodialysis. On admission, vital signs were stable except for mild fever, up to 37.8℃. Mild leukocytosis (11,500/mm3), was revealed in a complete blood count, and an increased blood urine nitrogen (92.7 mg/dL), creatinine (4.7 mg/dL) and serum glucose level (306 mg/dL) were confirmed in blood chemistry. Two hours after the admission, the patients body temperature had increased to 38.3℃ and chest x-ray, blood culture and urine culture were also performed to find the focus of the fever. Also, empirical antibiotics were started. On the second day of admission, body temperature was normalized to 36.5℃ and leukocyte levels decreased to 8,300/mm3. Antibiotics were discontinued and hemodialysis was performed. On the fifth day of admission, progressive quadriparesis beginning from both legs were detectes and a neurologist was consulted for evaluation. At that time, vital signs were stable (120/80-36.8℃-20), while physical examinations showed generalized edema and an appearance indicating chronic illness. A neurologic examination revealed Medical Research Council (MRC) grade IV deficit in the upper extremities and grade III in lower extremities. Also, position and vibration senses were abolished in all extremities, and deep tendon reflexes were decreased in all extremities. Pain and temperature senses were relatively intact and no other neurologic abnormalities, including neck stiffness and sphincter dysfunction, were found. To rule out rapidly progressing acute inflammatory demyelinating polyneuropathy, electromyographic (EMG), nerve conduction (NCS) and cerebrospinal fluid (CSF) studies were performed. The EMG and NCS tests revealed sensory-motor polyneuropathy. The CSF study revealed a leukocyte count of 425/µL (polymorphonuclear leukocyte - 73%), a red blood cell count of 6/µl, a glucose level of 50 mg/dL (serum glucose level was 288 mg/dL), and a protein level of 1168.8 mg/dL. On the sixth day, his motor symptoms grew worsened to grade I in upper extremities and grade 0 in lower extremities. Emergency spinal magnetic resonance imaging was performed, which confirmed a cervical epidural abscess between the fourth and fifth cervical vertebrae (Fig. 1). After emergency surgery, he was treated with broad spectrum antibiotics. Despite the emergency surgery, his motor symptoms did not improve. Blood and abscess cultures showed Methicillin-resistant Staphylococcus aureus. The patient expired despite the treatment with broad spectrum antibiotics for more than a month.
Cervical epidural abscess (CEA) is a very uncommon neurological infectious disease requiring emergency treatment. According to Lasker et al., the incidence of CEA varies between 1 in 70,000 and 1 in 400,000 admissions at major academic teaching hospitals in USA(3). About 70% of spinal epidural abscesses occur between age 31 and 70, with no tendency to any particular decade (5). Staphylococcus is the most common causative organism and accounts for 63% of the cultured organisms (1). The most common risk factor is known to be diabetes mellitus, followed by trauma, intravenous drug abuse, and alcoholism (5). Fever, back pain and progressive neurologic deficits are considered to be the triad of spinal epidural abscess (1, 4, 6) but CEA presenting all these typical symptoms is very rare, and the disease is especially difficult to diagnose in early stages because of the diversity of its clinical course (1). Although earlier diagnoses have been recently achieved with the development of sophisticated imaging. However, it is still difficult to diagnose CEA, especially when it shows an atypical clinical presentation as it did in the early days of this case.
Park et al. reported a case of CEA in 1993 which presented with complete loss of sensory sunctions including pain, temperature, position and vibration, below the fourth thoracic level and progressive paralytic motor weakness (7), but only transient and mild fever and progressive motor weakness were observed in this case. In immuno-compromised patients, as in this case, fever may not appear in spite of CEA (1, 4, 6, 7). Also, it is possible that peripheral polyneuropathies caused by underlying diabetes mellitus may have might masked any specific sensory abnormalities induced by CEA.
Figures and Tables
References
1. Curry WT Jr, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: clinical presentation, management, and outcome. Surg Neurol. 2005. 63:364–371.

2. Kricun R, Shoemaker EI, Chovanes GI, Stephens HW. Epidural abscess of the cervical spine: MR findings in five cases. AJR Am J Roentgenol. 1992. 158:1145–1149.

4. Hancock DO. A study of 49 patients with acute spinal extradural abscess. Paraplegia. 1973. 10:285–288.

5. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000. 23:175–204.

6. Pereira CE, Lynch JC. Spinal epidural abscess: an analysis of 24 cases. Surg Neurol. 2005. 63:Suppl 1. S26–S29.

7. Park HM, Kim SH, Kim J, Kim MH. Epidural abscess secondary to acute osteomyelitis of the cervical spine caused by E. coli. J Korean Neurol Assoc. 1993. 11:630–633.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download