Abstract
Cisatracurium provides superior hemodynamic stability with only minor release of histamine, and its metabolism via Hoffman elimination is independent of organ function. However, use of cisatracurium is limited because of reportedly slower onset and unsatisfactory intubating conditions. Many studies have shown that remifentanil might provide reliable intubating conditions; thus, we hypothesized that pretreatment with remifentanil before administration of cisatracurium might result in acceptable intubating conditions. Sixty healthy patients scheduled for elective surgery were enrolled and randomly divided into three groups: saline (Group I, n=20), remifentanil 0.5 µg/kg (Group II, n=20), and remifentanil 1.0 µg/kg (Group III, n=20). The anesthesia was induced with propofol 2.0 µg/kg given intravenously over 30 s followed by injection over 30 s of a different dose of remifentanil according to the study protocol. We examined the intubating condition by jaw relaxation, vocal cord state, and diaphragmatic response 90 s after administering cisatracurium. We also measured mean blood pressure, heart rate, and the onset time, which is the interval from the end of neuromuscular blocking agent administration until suppression of maximal T1 on a train-of four sequence. The mean values of the intubating condition after endotracheal intubation in Groups II and III were significantly lower than that in Group I (p<0.005), although the overall onset time of cisatracurium did not differ significantly between the three groups. Our results suggest that supplementation with remifentanil in an induction regimen with cisatracurium improves the quality of the intubating condition even though the onset time of cisatracurium is not shortened.
The ideal neuromuscular blocking agent needs to have the shortest time to endotracheal intubation, the best intubating conditions, and the shortest duration of muscle paralysis.1 In particular, the rapid sequence induction of anesthesia and endotracheal intubation are indicated in emergency situations in the presence of a full stomach or other conditions with an increased risk of aspiration.
Cisatracurium is a new neuromuscular blocking agent in Korea with characteristics that differ from those of other previously used agents. Cisatracurium is a kind of nondepolarizing neuromuscular blocking agent with intermediate action. Because cisatracurium is the isomer of atracurium, the neuromuscular blocking potency of cisatracurium is approximately three-fold that of atracurium and the time to maximum blocking is up to 2 minutes longer for equipotent doses of cisatracurium compared to atracurium.2 A pharmacodynamic profile of cisatracurium is similar to that of atracurium, except for a reportedly slower onset.3 Cisatracurium, unlike atracurium, is devoid of histamine-induced cardiovascular effects in the range of clinical doses. Also, cisatracurium is metabolized by Hoffmann elimination to laudanosine and a monoquaternary acrylate such as atracurium.4 Laudanosine, a metabolite of atracurium or cisatracurium, has central nervous system stimulating properties. Laudanosine is dependent on the liver and kidney for its elimination and its concentration is elevated in patients with hepatic or renal disease.5,6 Unlike atracurium, about five times less laudanosine is produced, and accumulation of this metabolite is not thought to be of any consequence in clinical practice.7 A cisatracurium dose provides superior hemodynamic stability with only minor release of histamine, and its metabolism via Hoffman elimination is independent of organ function. Despite these advantages, however, the use of cisatracurium is limited because of reportedly slower onset and unsatisfactory intubating conditions compared with an equipotent dose of other neuromuscular blocking agents.8,9
Traditionally, many studies have focused on reducing the onset time of nondepolarizing neuromuscular blocking agents. First, briefly, large doses of cisatracurium may shorten onset time. As larger doses are used, the onset time is shortened more. But these times are still much slower than those with succinylcholine or rocuronium.10 Furthermore, large doses of cisatracurium are not suitable for a short period of anesthesia. Secondly, the onset time of a neuromuscular blocking agent may be accelerated by the priming principle; that is, administration of a small subparalyzing dose of the agent several minutes before the principal intubating dose.11 However, during the relatively long priming interval, the awake patient may suffer from distressing symptoms of muscle weakness such as blurred vision, dysphagia, and respiratory difficulty.12 Third, the onset of action of a neuromuscular blocking agent is also influenced by the speed with which the agent is delivered to the synaptic cleft. Ephedrine is a weak, indirect, and direct-acting sympathomimetic agent that improves venous return and increases cardiac output. Albert et al.13 reported that a low dose (70 µg/kg) of ephedrine given before induction of anesthesia improves tracheal intubating conditions 2 minutes after cisatracurium 0.15 mg/kg. However, larger doses of ephedrine induce a statistically significant increase in mean arterial pressure and heart rate during induction of anesthesia.14,15 Thus, this study assumed that another regimen would improve clinical intubating conditions and would shorten the onset time of cisatracurium following administration of remifentanil.
Recently, many studies have shown that it is possible to successfully intubate the trachea without the use of muscle relaxants, and the combination of propofol and an opioid is a well-established practice in both adult and pediatric practice.16-18 These studies have concluded that remifentanil might improve the intubating condition even if a neuromuscular blocking agent is not used. However, no studies have investigated the effects on intubating conditions when cisatracurium is administrated combined with propofol and remifentanil. In addition, remifentanil has been shown to have a large volume of distribution and rapid clearance (92-76 ml/kg/min) with a similar elimination half-life in all age groups, with means of 3.4-5.7 min,19 making it suitable for rapid onset and short duration of action during rapid sequence induction. The low dose was chosen in an attempt to minimize effects on apnea time and cardiovascular parameters. In the present study, therefore, we hypothesized that pretreatment with remifentanil before administration of cisatracurium might result in an acceptable intubating condition.
After obtaining approval from the Institutional Review Board of the Chonnam National University Hospital and informed written consent from the patients, 60 American Society of Anesthesia I or II patients aged from 25 to 65 years who were undergoing general anesthesia and endotracheal intubation for elective surgery were enrolled in the study. Exclusion criteria were any disorder of the cardiovascular, hepatic, renal, or neuromuscular systems known from history or clinical examination. Patients in whom difficult intubation was expected, such as pregnant or lactating women and patients on medication known to interact with neuromuscular blocking drugs, e.g., antibiotics, antidepressants, anticonvulsants antiarrhythmics, and magnesium sulfate, were also excluded.
The calculated sample was 20 per group with a total sample size of 60 for the three groups of the study. Patients were equally randomly assigned by use of a random number generator to one of the three study groups to receive the following in a double-blinded manner: Group I, saline; Group II, remifentanil 0.5 µg/kg; and Group III, remifentanil 1.0 µg/kg.
All patients were premedicated with midazolam 0.1 mg/kg orally 60 minutes before the induction of anesthesia. Before arrival in the operating room, the patients had an intravenous catheter placed to allow administration of fluids and drugs. Standard monitoring, including noninvasive blood pressure monitoring, electrocardiography, pulse oximetry, and bispectral index score monitoring was applied and assessed continuously. Before induction of anesthesia, surface electrodes were placed over the ulnar nerve at the wrist for neuromuscular monitoring. After loss of consciousness, the ulnar nerve was stimulated at the wrist with a square wave stimulus set at a current of 50 mA and duration of 0.2 ms.20 Each stimulus was delivered in a train-of-four sequence and was repeated every 12 s by using a TOF Guard neuromuscular transmission monitor (Organon Teknika NV, Boxtel, Netherlands).
After the patients breathed 100% oxygen, anesthesia was induced with propofol 2.0 mg/kg given intravenously over 30 s followed by injection of a different dose of remifentanil over 30 s. The remifentanil syringe was prepared by an independent anesthesiologist in a total volume of 10 ml with normal saline. Therefore, all anesthesiologists were blinded to the dose of remifentanil. We performed endotracheal intubation 90 s after the end of cisatracurium administration by the same skilled anesthesiologist who was not involved in the anesthesia technique and was consequently blinded to the dose of remifentanil. To avoid vocal cord injury, endotracheal intubation was not attempted if the vocal cords were fully closed. After intubation, anesthesia was maintained with 50% nitrous oxide in oxygen and 2.0 vol% sevoflurane.
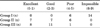
Intubating conditions were graded by using the scoring scale initially described by Cooper et al. (Table 1). The assessed score was classified as a grade of excellent (0-1), good (2-3), poor (4-5), or impossible (6-9), respectively.21 The onset time was defined as the time interval from the end of neuromuscular blocking agent administration to the maximal suppression of T1%. Measurements of heart rate and mean blood pressure were made immediately before induction, immediately before tracheal intubation, and 1 and 3 minutes after tracheal intubation. Patients were monitored for any signs of histamine release clinically through skin changes graded as flush (if redness lasted >120 s), erythema, or wheals8 and the presence of any hemodynamic changes or bronchospasm.
Data were processed by using SPSS version 16.0 (SPSS Inc, Chicago, IL, USA). Quantitative data were expressed as means±standard deviations. Student's t-test was used on parametric data (age, height, weight, aspartate aminotransferase, alanine aminotransferase, creatinine, estimated glomerular filtration rate, mean blood pressure, heart rate, intubating condition score, and onset time) paired within groups and unpaired between groups. The chi-squared test was used for nominal data (gender). A probability value (p value) <0.05 was considered statistically significant.
There were no significant differences between the three groups in gender, age, height, weight, aspartate aminotransferase, alanine aminotransferase, creatinine, or estimated glomerular filtration rate. Neither were there significant differences in the mean blood pressure and heart rate before anesthetic induction (Table 2).
Endotracheal intubation was successful on the first attempt in all patients. The mean value of the intubating condition after endotracheal intubation was significantly lower in Groups II and III than in Group I in a dose-dependent manner (p<0.005; Fig. 1). Intubating conditions were excellent or good in 14 patients in Group II and 19 patients in Group III (Table 3). On the other hand, no patients were classified as having excellent or good intubating conditions in Group I. Fourteen patients in Group I had an impossible intubating condition. The remaining patients were rated as poor. The overall onset time of cisatracurium did not differ significantly between the three groups (p=0.748; Fig. 2). The onset time was 181±53 s in Group I, 188±41 s in Group II, and 178±29 s in Group III.
Hemodynamic changes within each group are shown in Fig. 3 and Fig. 4. The mean blood pressure and heart rate in all 3 groups decreased more than the baseline value just before endotracheal intubation (p<0.05; Fig. 3, Fig. 4). The mean blood pressure just before endotracheal intubation in Groups II and III was significantly lower than that in Group I (p<0.05). At 1 minute after endotracheal intubation, the mean blood pressure eventually became elevated in all 3 groups. The mean blood pressure in only Group I rose more than the baseline value at 1 minute after endotracheal intubation (p<0.05). In Groups II and III, the mean blood pressure was not significantly different from the baseline value. However, the mean blood pressure at 1 and 3 minutes after endotracheal intubation in Groups II and III was significantly lower than in Group I (p<0.05 or p<0.005).
The heart rate just before endotracheal intubation in Groups II and III was significantly lower than that in Group I (p<0.05). At 1 minute after endotracheal intubation, the heart rate eventually became elevated in all 3 groups. The heart rate in only Group I rose more than the baseline value at 1 and 3 minutes after endotracheal intubation (p<0.05). In Groups II and III, the heart rate was not significantly different from the baseline value. However, the heart rate at 1 and 3 minutes after endotracheal intubation was significantly lower in Groups II and III than in Group I (p<0.05 or p<0.005).
All patients were assessed for intubating condition, onset time, and hemodynamics. The overall onset time of cisatracurium did not differ significantly between the three groups. However, the mean value of the intubating condition after endotracheal intubation in Groups II and III was significantly lower than that in Group I (p<0.005). This finding suggested that supplementation with remifentanil in the cisatracurium induction regimen improved the quality of tracheal intubation in terms of respiratory depressant and analgesic effects. However, the action of remifentanil was not directly involved with muscular relaxation by the neuromuscular blocking agent. Furthermore, hemodynamic changes in both heart rate and mean blood pressure during anesthetic induction were similar between the three groups. The mean blood pressure and heart rate just before and after endotracheal intubation in Groups II and III were significantly lower than in Group I. This suggests that the use of remifentanil can decrease cardiovascular responses and improve the hemodynamic stability during endotracheal intubation.
A rapid sequence induction of anesthesia and endotracheal intubation are indicated in emergency situations in the presence of a full stomach or other conditions with an increased risk of aspiration. Traditionally, succinylcholine has been the neuromuscular blocking drug of choice for rapid sequence induction of anesthesia. However, as a result of its depolarizing effect, succinylcholine can have serious side effects and is contraindicated in many conditions. Rocuronium has the most rapid onset of the currently available nondepolarizing neuromuscular blocking drugs.22 However, animal studies have suggested that rocuronium is mostly metabolized in the liver and excreted through bile, and less than 10% of the unchanged form after a bolus administration is detected in cat urine in 24 hours.23 The duration of neuromuscular blockade of rocuronium at an equipotent single dose may be prolonged and variable in patients with liver and kidney failure.24,25 In this respect, cisatracurium is metabolized by Hoffmann elimination to laudanosine and is recommendable in patients with liver and kidney failure. However, cisatracurium in a clinical dose or method has a relatively long onset time, thus discouraging rapid sequence induction.26,27
As mentioned earlier, the pharmacodynamic profile of cisatracurium is similar to that of atracurium, except for a reportedly slower onset.3 Bluestein and colleagues28 reported that increasing the initial dose of cisatracurium (from 0.1 to 0.15 and 0.2 mg/kg) decreased the mean time of onset (from 4.6 to 3.4 and 2.8 minutes, respectively) and increased the mean time of clinically effective duration (45 to 55 and 61 minutes, respectively). Doses of 0.15 mg/kg (3×ED95) and 0.2 mg/kg (4×ED95) of cisatracurium may produce generally good or excellent conditions of intubation in 2.0 and 1.5 minutes, respectively. The cisatracurium dose of 0.15 mg/kg (3×ED95) is higher than the dose of atracurium 0.5 mg/kg (2×ED95) required to produce clinically acceptable intubation conditions after 120 s.29 Mandal30 conducted a study to determine the minimum possible dose of cisatracurium for achieving excellent to good intubating conditions within 90 s of administration under general anesthesia. They concluded that the minimum dose required to achieve excellent to good intubating conditions with cisatracurium is 0.20 mg/kg at 90 s after administration. In accordance with these results, we can conclude that at the low dose (3×ED95) cisatracurium would not create a superior onset time and intubating condition at 90 s compared with other neuromuscular blocking agents. Thus, this study was designed to compare the effect of saline and remifentanil administration on neuromuscular blocking agent (onset time, intubating condition) and hemodynamic responses by low-dose cisatracurium bolus injection (3×ED95) at 90 s.
From a different point of view, remifentanil has unique properties and undergoes rapid hydrolysis. It has a rapid termination of action owing to hydrolysis by nonspecific tissue esterases with a context-sensitive half-life of just over 3 min, allowing rapid return of spontaneous respiration. Although the onset of effect is similar to that of alfentanil, within 1 to 2 minutes, it has a shorter half-life and the time to recovery is not greatly influenced by the dose.31 Those clinical properties make remifentanil the short-acting opioid of choice for circumstances in which an intense opioid effect of short duration is required.
Recent studies have suggested that short-acting opioids such as alfentanil and remifentanil may provide adequate conditions for laryngoscopy and endotracheal intubation even if neuromuscular blocking agents are not used owing to several properties of these opioids.16-18 In particular, remifentanil has analgesic efficacy and a respiratory depressant effect. When Stevens and Wheatley17 used remifentanil 2 µg/kg in combination with propofol 2 mg/kg, excellent intubating conditions did not exceed 50%. In another study, Klemola et al.32 reported that the administration of remifentanil 4 µg/kg with propofol 2.5 mg/kg provided excellent intubating conditions in only 60% of patients.16 Supplementing a propofol-opioid induction regimen with a nondepolarizing agent improves the quality of tracheal intubation and decreases postoperative hoarseness. Regarding the intubating conditions in our study, it was estimated that use of remifentanil showed a statistically significant difference versus the use of saline with excellent endotracheal intubation conditions.
In addition to acceptable intubation conditions, the usual increase in cardiovascular responses after tracheal intubation was not observed when remifentanil was provided. Cha et al.33 stated that remifentanil 0.5 µg/kg is appropriate for suppressing the cardiovascular responses to endotracheal intubation in adults when anesthesia is in duced by propofol 2 mg/kg or rocuronium 1 mg/kg. Lee et al.34 also reported that remifentanil 1 µg/kg is appropriate when anesthesia is induced by sevoflurane 2 vol% and N2O 50% in adults. McAtamney et al.35 reported that remifentanil 1.0 µg/kg is the optimum dose in adults. Referentially, a high dose of remifentanil provides excellent or satisfactory intubating conditions with acceptable hemodynamic responses in healthy patients with favorable airway anatomy. However, the decrease in arterial pressure following remifentanil might not be well tolerated in less healthy patients such as the elderly, compromised patients, or in patients with clinically significant cardiovascular or cerebrovascular disease. Also, muscle rigidity may be associated with rapid infusions of large doses of potent opioids.36 Thus, the use of remifentanil can decrease such cardiovascular responses; the optimum dose of remifentanil has been reported to be 0.5-1.0 µg/kg. Our results confirm better control of hemodynamic changes following intubation with 0.5-1.0 µg/kg of remifentanil compared with saline. The absence of signs indicating opioid-induced hypotension or muscular rigidity in our patients might be due to the rather low doses of remifentanil. All things considered in our results, in terms of respiratory depressant effects and analgesic efficacy, remifentanil is regarded as being effective in providing acceptable intubation conditions and in preventing the cardiovascular responses to short-term harmful stimulations such as endotracheal intubation and rapid sequence induction.
As a further note, the propofol that we used as the hypnotic agent in our study has a partial depressant effect on pharyngeal and laryngeal muscles. McKeating et al.37 found that when no neuromuscular blocking agent is given, laryngoscopy is easier to perform after propofol than after an equipotent dose of thiopentone, and that pharyngeal and laryngeal activity are more depressed after administration of propofol than after thiopentone. Using a fiberoptic laryngoscope, Barker et al.38 observed that vocal cords adducted to a greater extent after induction of anesthesia with thiopentone than with propofol. More recently, Eames et al.39 revealed that respiratory resistance after tracheal intubation was lower after induction with propofol than after induction with thiopental or with high-dose etomidate. In accordance with these results, we concluded that pharyngeal and laryngeal activities were more depressed after administration of propofol than another hypnotic. The depressant effect of propofol may contribute to improving the intubating condition.
There are some disadvantages and limitations in the present study. This study was conducted in healthy young patients. The actual response using pretreatment with remifentanil before administration of cisatracurium might be quite different in the elderly, compromised patients, or those with clinically significant hepatic failure or renal disease, even though cisatracurium and remifentanil have superior pharmacokinetics and pharmacodynamics in patients with hepatic failure or renal disease. The intubating response might be remarkable and deteriorate, and the decrease in arterial pressure might not be well tolerated in those less healthy patients. In the future, the effects on intubating responses in patients with hepatic failure or clinical renal disease need to be investigated.
In conclusion, our report shows that supplementation with remifentanil in an induction regimen with cisatracurium improves the quality of tracheal intubation even though the onset time of cisatracurium is not shortened. In addition to providing acceptable intubation conditions, use of remifentanil helps to decrease such cardiovascular responses. With pretreatment with remifentanil before administration of cisatracurium, we were able to reproduce the advantages of cisatracurium such as no accumulation of metabolites.
Figures and Tables
FIG. 1
Intubating condition of cisatracurium in Group I, II, III. Group I: saline, Group II: remifentanil 0.5 µg/kg, Group III: remifentanil 1.0 µg/kg. *p<0.005 compared with Group I.

FIG. 2
Onset time of cisatracurium in Group I, II, III. Group I: saline, Group II: remifentanil 0.5 µg/kg, Group III: remifentanil 1.0 µg/kg. Statistical significance accepted when p<0.05. There was no statistically significant difference between the groups.

FIG. 3
Changes in the mean blood pressure in Group I, II, III. GroupI : saline, Group II: remifentanil 0.5 µg/kg, Group III : remifentanil 1.0 µg/kg. B: baseline, 0: just before intubation, 1 and 3: 1 and 3 minutes after intubation. *p<0.05 compared with baseline, †p<0.05 compared with Group I, ‡p<0.005 compared with Group I.

FIG. 4
Changes in the heart ratein Group I, II, III. Group I: saline, Group II: remifentanil 0.5 µg/kg, Group III: remifentanil 1.0 µg/kg. B: baseline, 0: just before intubation, 1 and 3: 1 and 3 minutes after intubation. *p<0.05 compared with baseline, †p<0.05 compared with Group I, ‡p<0.005 compared with Group I.

TABLE 1
Assessment of intubating condition

Modified from Cooper et al.13 Intubating conditions were rated to a higher score if one of the three conditions required was not met.
TABLE 2
Demographic data

Values are Mean±SD. Estimating glomerular filtration rate is calculated by Cockcroft-Gault equation. Statistical significance accepted when p<0.05. There was no statistically significant difference between the groups. Group I: saline, Group II: remifentanil 0.5 µg/kg, Group III: remifentanil 1.0 µg/kg.
ACKNOWLEDGEMENTS
This study was supported by a grant (CRI12048-1) from the Chonnam National University Hospital Research Institute of Clinical Medicine.
References
1. Sluga M, Ummenhofer W, Studer W, Siegemund M, Marsch SC. Rocuronium versus succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. Anesth Analg. 2005. 101:1356–1361.

2. Kleinman W NG, Nitti JT, Raya J. Morgan GE MM, Murray MJ, editors. Neuromuscular blocking agents. Clinical anesthesilogy. 2006. 4th ed. New York: Lange Medical Books;205.
3. Mellinghoff H, Radbruch L, Diefenbach C, Buzello W. A comparison of cisatracurium and atracurium: onset of neuromuscular block after bolus injection and recovery after subsequent infusion. Anesth Analg. 1996. 83:1072–1075.
4. Wastila WB, Maehr RB, Turner GL, Hill DA, Savarese JJ. Comparative pharmacology of cisatracurium (51W89), atracurium, and five isomers in cats. Anesthesiology. 1996. 85:169–177.

5. Canfell PC, Castagnoli N Jr, Fahey MR, Hennis PJ, Miller RD. The metabolic disposition of laudanosine in dog, rabbit, and man. Drug Metab Dispos. 1986. 14:703–708.
6. Parker CJ, Hunter JM. Pharmacokinetics of atracurium and laudanosine in patients with hepatic cirrhosis. Br J Anaesth. 1989. 62:177–183.

7. Kisor DF, Schmith VD, Wargin WA, Lien CA, Ornstein E, Cook DR. Importance of the organ-independent elimination of cisatracurium. Anesth Analg. 1996. 83:1065–1071.

8. Correa CM, Sudo GZ, Sudo RT. Hemodynamic effects of atracurium and cisatracurium and the use of diphenhydramine and cimetidine. Rev Bras Anestesiol. 2010. 60:52–63.

9. Kirov K, Motamed C, Decailliot F, Behforouz N, Duvaldestin P. Comparison of the neuromuscular blocking effect of cisatracurium and atracurium on the larynx and the adductor pollicis. Acta Anaesthesiol Scand. 2004. 48:577–581.

10. Lighthall GK, Jamieson MA, Katolik J, Brock-Utne JG. A comparison of the onset and clinical duration of high doses of cisatracurium and rocuronium. J Clin Anesth. 1999. 11:220–225.

11. Schwarz S, Ilias W, Lackner F, Mayrhofer O, Foldes FF. Rapid tracheal intubation with vecuronium: the priming principle. Anesthesiology. 1985. 62:388–391.
12. Mirakhur RK, Lavery GG, Gibson FM, Clarke RS. Intubating conditions after vecuronium and atracurium given in divided doses (the priming technique). Acta Anaesthesiol Scand. 1986. 30:347–350.

13. Albert F, Hans P, Bitar Y, Brichant JF, Dewandre PY, Lamy M. Effects of ephedrine on the onset time of neuromuscular block and intubating conditions after cisatracurium: preliminary results. Acta Anaesthesiol Belg. 2000. 51:167–171.
14. Leykin Y, Pellis T, Lucca M, Gullo A. Effects of ephedrine on intubating conditions following priming with rocuronium. Acta Anaesthesiol Scand. 2005. 49:792–797.

15. Tan CH, Onisong MK, Chiu WK. The influence of induction technique on intubating conditions 1 min after rocuronium administration: a comparison of a propofol-ephedrine combination and propofol. Anaesthesia. 2002. 57:223–226.

16. Klemola UM, Mennander S, Saarnivaara L. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand. 2000. 44:465–469.

17. Stevens JB, Wheatley L. Tracheal intubation in ambulatory surgery patients: using remifentanil and propofol without muscle relaxants. Anesth Analg. 1998. 86:45–49.
18. Taha S, Siddik-Sayyid S, Alameddine M, Wakim C, Dahabra C, Moussa A, et al. Propofol is superior to thiopental for intubation without muscle relaxants. Can J Anaesth. 2005. 52:249–253.

19. Ross AK, Davis PJ, Dear Gd GL, Ginsberg B, McGowan FX, Stiller RD, et al. Pharmacokinetics of remifentanil in anesthetized pediatric patients undergoing elective surgery or diagnostic procedures. Anesth Analg. 2001. 93:1393–1401.

20. Plaud B, Debaene B, Donati F. The corrugator supercilii, not the orbicularis oculi, reflects rocuronium neuromuscular blockade at the laryngeal adductor muscles. Anesthesiology. 2001. 95:96–101.

21. Cooper R, Mirakhur RK, Clarke RS, Boules Z. Comparison of intubating conditions after administration of Org 9246 (rocuronium) and suxamethonium. Br J Anaesth. 1992. 69:269–273.

22. Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008. (2):CD002788.

23. Khuenl-Brady K, Castagnoli KP, Canfell PC, Caldwell JE, Agoston S, Miller RD. The neuromuscular blocking effects and pharmacokinetics of ORG 9426 and ORG 9616 in the cat. Anesthesiology. 1990. 72:669–674.

24. Robertson EN, Driessen JJ, Booij LH. Pharmacokinetics and pharmacodynamics of rocuronium in patients with and without renal failure. Eur J Anaesthesiol. 2005. 22:4–10.

25. van Miert MM, Eastwood NB, Boyd AH, Parker CJ, Hunter JM. The pharmacokinetics and pharmacodynamics of rocuronium in patients with hepatic cirrhosis. Br J Clin Pharmacol. 1997. 44:139–144.

26. Amin AM, Mohammad MY, Ibrahim MF. Comparative study of neuromuscular blocking and hemodynamic effects of rocuronium and cisatracurium under sevoflurane or total intravenous anesthesia. Middle East J Anesthesiol. 2009. 20:39–51.
27. Lin SP, Chang KY, Chen YJ, Lin SM, Chang WK, Chan KH, et al. Priming with rocuronium to accelerate the onset time of cisatracurium during intubation. J Chin Med Assoc. 2009. 72:15–19.

28. Bluestein LS, Stinson LW Jr, Lennon RL, Quessy SN, Wilson RM. Evaluation of cisatracurium, a new neuromuscular blocking agent, for tracheal intubation. Can J Anaesth. 1996. 43:925–931.

29. Belmont MR, Lien CA, Quessy S, Abou-Donia MM, Abalos A, Eppich L, et al. The clinical neuromuscular pharmacology of 51W89 in patients receiving nitrous oxide/opioid/barbiturate anesthesia. Anesthesiology. 1995. 82:1139–1145.

30. Mandal P. Intubating conditions after cisatracurium administration: a dose response study in adults. J Anaesth Clin Pharmacol. 2002. 18:147.
31. Egan TD, Minto CF, Hermann DJ, Barr J, Muir KT, Shafer SL. Remifentanil versus alfentanil: comparative pharmacokinetics and pharmacodynamics in healthy adult male volunteers. Anesthesiology. 1996. 84:821–833.
32. Klemola UM, Mennander S, Saarnivaara L. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand. 2000. 44:465–469.

33. Cha JW, Kwak SH, Kim SJ, Choi JI, Kim CM, Jeong ST, et al. Optimal dose of remifentanil to blunt hemodynamic response to laryngoscopy and endotracheal intubation during induction of anesthesia with propofol. Korean J Anesthesiol. 2006. 51:292–296.

34. Lee JR, Jung CW, Lee JH, Choi IY, Seo KS, Kim HK, et al. Optimal dose of remifentanil to suppress cardiovascular responses to laryngoscopic endotracheal intubation. Korean J Anesthesiol. 2005. 49:780–785.

35. McAtamney D, O'Hare R, Hughes D, Carabine U, Mirakhur R. Evaluation of remifentanil for control of haemodynamic response to tracheal intubation. Anaesthesia. 1998. 53:1223–1227.

36. Thompson JP, Rowbotham DJ. Remifentanil-an opioid for the 21st century. Br J Anaesth. 1996. 76:341–343.

37. McKeating K, Bali IM, Dundee JW. The effects of thiopentone and propofol on upper airway integrity. Anaesthesia. 1988. 43:638–640.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download