Abstract
Purpose
To determine whether we should recommend ultrasonography (US) for an incidental thyroid nodule identified by additional cervicothoracic sagittal T2-weighted image (C-T sag T2WI) of lumbar spine magnetic resonance imaging (MRI).
Materials and Methods
A retrospective study of 61 patients who underwent both lumbar spine MRI and thyroid US between December 2011 and April 2015 was conducted. For all US-found thyroid nodules > 1 cm, investigators evaluated whether there was any correlation between thyroid nodule detectability by C-T sag T2WI and US features such as echogenicity, composition, or suspicion of malignancy.
Results
Solid hypoechoic (2/4; 50%) or mixed echoic nodules (4/8; 50%) appeared to be found relatively more easily by C-T sag T2WI than more benign-looking solid isoechoic (1/4; 25%) or spongiform nodules (0/6; 0%). Among six nodules with ultrasonographic suspicion for malignancy, only one nodule was detected by C-T sag T2WI.
An incidental thyroid nodule is a very common finding in magnetic resonance imaging (MRI) with scan coverage of the neck area (12) , and is also a very important finding because of the high possibility of malignancy (~12-28%) (34). A recent study reported that an incidental thyroid nodule was detected by cervical spine MRI in approximately 5% of patients (5). In lumbar spine MRI, if the additional cervicothoracic sagittal T2-weighted image (C-T sag T2WI) is acquired as a routine scanning protocol, thyroid nodules also can be detected in those images. Although it has been reported previously that cervicothoracic spinal pathologic lesions can be detected very easily through C-T sag T2WI (6), to our knowledge, no reports have evaluated the detection rate of thyroid nodules by lumbar spine MRI, based on findings of thyroid ultrasonography (US). In addition to evaluating detection rates, we sought to determine whether US should be recommended for an incidental thyroid nodule by analyzing different detection rates depending on US character of the nodules.
Background for this study includes the following: 1) interpreting radiologists have limited interest in thyroid lesions found by lumbar spine MRI, although the detection of incidental thyroid lesions has important clinical implications; and 2) there is no widely accepted management guideline for incidental thyroid nodules found by lumbar spine MRI.
The study population included 61 patients (M:F = 9:52; age range, 29-79 years; average age, 56.8 years) with complaints of lower back pain who underwent both routine lumbar spine MRI and thyroid US between December 2011 and April 2015. Reasons for undergoing thyroid US included health check-up (n = 27), follow up for a known thyroid nodule (n = 24), sore throat (n = 4), thyroiditis (n = 4), palpable neck mass (n = 1) and feeling of neck irritation (n = 1). The interval between lumbar spine MRI and thyroid US was 0-27 months, with an average of 9.0 months (+ SD). Patients with post-thyroidectomy or cyst aspiration statuses were excluded. This retrospective study was approved by the Institutional Review Board.
Lumbar spine MRI was performed on a 1.5 T MRI system (Signa Horizon; GE Healthcare Systems, Milwaukee, WI, USA) according to the standard protocol for spinal MRI. After conventional lumbar spine MRI sequences, including sagittal T1-weighted images, sagittal T2-weighted images, fat-suppressed sagittal T2-weighted images, and axial T2-weighted images, were obtained, the C-T sag T2WI sequence also was obtained as a part of the routine lumbar spine MRI protocol. We reviewed the C-T sag T2WI sequence in this study. The imaging parameters of the C-T sag T2WI are follows: TR/TE, 3500/115; matrix size, 448 × 320; field of view (FOV), 39 × 39 cm; slice thickness, 3.5 mm; intersection gap, 0.1 mm; echo train length, 24; readout bandwidth, 83.33 Hz/Px; NEX, 2; and flip angle, 90°. An 8-channel C-T-L Spine Array coil (GE Healthcare Systems) was used. A presaturation band was routinely applied at anterior portion of the C-T sag T2WI without any negative effect on visualization of thyroid gland.
Thyroid US studies were conducted by several radiologists with more than 5 years of experience in thyroid imaging. The radiologists employed one of the following three real-time ultrasonographic machines with linear multifrequency transducers: Prosound Alpha 5 SV (Hitachi Aloka, Tokyo, Japan), Accuvix XG (Samsung Medison, Seoul, Korea), or Toshiba Aplio 500 (Toshiba Corporation, Tokyo, Japan).
Lumbar spine MRI and thyroid US images were interpreted retrospectively by a fellowship-trained musculoskeletal radiologist with 9 years of experience. At first, the radiologist evaluated the number and size of detectable thyroid nodules on each C-T sag T2WI included in lumbar spine MRI. Ambiguous thyroid lesions were excluded from counts to avoid false-positive cases and the possibility of additional cost and time expenditures.
Next, the radiologist determined whether the thyroid nodule was also seen in each thyroid US image. All US-found thyroid nodules were categorized as < 1 cm or > 1 cm in size, and each detection rate by C-T sag T2WI was calculated, based on US findings.
Number, size, and ultrasonographic character were evaluated for all thyroid nodules > 1 cm in each thyroid US. All US-found thyroid nodules > 1 cm were classified into one of five types (solid hypoechoic, solid isoechoic, mixed echoic, spongiform, and purely cystic nodule) by their ultrasonographic echogenicity and composition, based on the revised management guidelines issued by the American Thyroid Association (7). Then, the radiologist investigated whether there was any correlation between thyroid nodule detectability by C-T sag T2WI and US features such as echogenicity, composition, or suspicion for malignancy based on Thyroid Imaging Reporting and Data System for US Features of Nodules (TIRADS) (8).
In a retrospective analysis of a total 61 patients, 102 nodules < 1 cm and 24 nodules > 1 cm were collected from the thyroid US. The detection rate by C-T sag T2WI of lumbar spine MRI was 3.9% (4/102) for nodules of < 1 cm in size and 33.3% (8/24) for nodules > 1 cm, based on thyroid US findings. The difference in the detection rates between < 1-cm nodules and > 1-cm nodules was statistically significant (P < 0.05) (Table 1). The mean size of the detected 12 thyroid nodules by C-T sag T2WI was 12.5 mm.
When categorizing 24 thyroid nodules > 1 cm by US features, the detection rate was 50% for solid hypoechoic (2/4), 50% for mixed echoic (4/8), 25% for solid isoechoic (1/4), 0% for spongiform (0/6), and 50% for purely cystic nodules (1/2). Detection rates of combined solid hypoechoic or mixed echoic nodules (6/12; 50%) - which have more malignant potential in general - were higher than for rates of other subtypes (2/12; 16.7%) (Table 2). However, this variation in detection rates by subtypes was not statistically significant, because of the small number of subjects in the study group (P = 0.2170).
Six nodules were suspicious for malignancy based on TIRADS by US, and were all solid hypoechoic. Two nodules were > 1 cm and four nodules were < 1 cm in size. Only one nodule > 1 cm in size was detected by C-T sag T2WI (Fig. 1), but it was confirmed as benign by biopsy. Two < 1 cm nodules which were not detected by C-T sag T2WI were confirmed as papillary carcinomas by biopsy.
Because C-T sag T2WI has the advantages of having a wide FOV and a whole spine review of segmental variations with a short scan time, many institutions include the sequence in the routine scan protocol of the lumbar spine MRI. In our hospital, the FOV of the sequence is 39 × 39 cm and the scan time is only 105 seconds, and we use it as a routine MRI protocol.
On C-T sag T2WI, the thyroid gland is located in front of the cervical spine and can be delineated relatively clearly if no artifact exists. Nevertheless, many radiologists do not pay attention to thyroid abnormality seen by C-T sag T2WI, and although thyroid nodules are seen, they are often not described in radiologic reading reports. Furthermore, although such nodules may be mentioned, it is unclear whether additional thyroid US is needed or not. Actually also in our hospital, only one thyroid nodule was described in the radiologic reading report among 12 nodules detected retrospectively by C-T sag T2WI. Therefore, in this study, we studied the detection rate of thyroid nodules by C-T sag T2WI and investigated whether US should be recommended for incidental thyroid nodules, based on an analysis of different detection rates depending on US character of the nodules.
Recently, Kim et al. (5) reported that one or more incidental thyroid nodules were detected in 5.1% of all patients who underwent cervical spine MRI. In our study, 11 of 61 patients (18.0%) had one or more thyroid nodules seen by C-T sag T2WI (two nodules in only one patient), so the prevalence in the present study was far higher than that in the previous study. The biggest reason is that 24 of 61 patients (39.3%) in our study group underwent thyroid US for follow-up of known thyroid nodules, so that the incidence must be much higher than that of the general public. Even though the thyroid nodule incidence was far higher than that of previous studies due to selection bias, a relatively larger number of thyroid nodules rather helped to solve the primary question of our study trying to determine what percentage of known 126 thyroid nodules can be detected by additional C-T sag T2WI. As a result, only 12 nodules (9.5%) were detected so that we concluded there are limits to the reliability of thyroid nodule detection by C-T sag T2WI. Nevertheless, judging from the high incidence rate, C-T sag T2WI can be expected to have a comparable level of ability to detect an incidental thyroid nodule with only sagittal images of wide FOV in comparison with cervical spine MRI, including both axial and sagittal images of narrow FOV. This is also supported by the fact that the mean size of the detected thyroid nodules by C-T sag T2WI was 12.5 mm in our study, which is slightly larger but similar to the mean size of 11.6 mm in the study by Kim et al. (5).
The detection rate of thyroid nodules < 1 cm by C-T sag T2WI was very low, at 3.9% (4/102). Even though the detection rate of thyroid nodules > 1 cm was relatively higher, the reliability for detection seemed unsatisfactory; only 8 of 24 nodules > 1 cm in size were detected by C-T sag T2WI, and only 2 of 5 nodules > 2 cm were detected. We chose the 1-cm size as an important criterion in this study, because some previous management guidelines pertaining to incidental thyroid nodules have recommended further action, such as thyroid US, history taking, or thyroid function test if the incidental thyroid nodule is larger than 1 cm (7910).
It has been reported that there is a positive correlation between the size of a thyroid nodule and its malignancy potential (11). So one result of this study that larger nodules are more easily detected by C-T sag T2WI may mean that, speaking as a different angle, an incidental thyroid nodule detected by C-T sag T2WI can be more likely a larger nodule with relatively more malignant potential than usual US-found incidental thyroid nodules.
With all US-found thyroid nodules > 1-cm, the combined detection rate of solid hypoechoic or mixed echoic nodules (6/12; 50%) which have more malignant potential in general was higher than that of other subtypes (2/12; 16.7%) (Figs. 2, 3). Solid hypoechoic nodules are well known for the most common feather of malignant nodules (81213) . Recent reports also have found a high probability of malignancy for mixed echoic nodules (approximately 5-18%) (31415). Therefore, even though the overall detection rate of thyroid nodules by C-T sag T2WI is low, we need to pay attention to the finding that solid hypoechoic or mixed echoic nodules with relatively greater potential of malignancy might be detected more easily than solid isoechoic or spongiform nodules, which have a relatively greater possibility of being benign. This underlies our opinion that it would be better to recommend US for an incidental thyroid nodule detected by C-T sag T2WI. In other words, most incidental thyroid nodules detected by C-T sag T2WI are > 1-cm solid hypoechoic or mixed echoic nodules, so we suggest that it would be better to recommend thyroid US for identifying malignancy.
However, we could not find any evidence that thyroid nodules that are suspicious for malignancy on the basis of US findings can be more easily detected by C-T sag T2WI. In this study, a total of 6 nodules showed suspicious US features (e.g., taller-than-wide appearance, marked hypoechogenicity). Among these, 4 nodules < 1 cm were not detected by C-T sag T2WI, and only one of two nodules > 1 cm was detected by C-T sag T2WI. It was the only nodule mentioned by a radiologic reading report in our hospital, and it appeared as a 12-mm solid hypoechoic nodule but was confirmed as benign by biopsy (Fig. 1). So in the future, to figure out relation of thyroid malignancy and chance of detection by C-T sag T2WI, further researches with a larger patient group will be needed.
The study had several limitations. First, because a thyroid nodule is very small compared to the wide FOV of C-T sag T2WI, definitive assessments of the existence of thyroid nodules seem to be a fundamentally subjective exercise. Second, we cannot produce statistically significant results for analysis with nodules > 1 cm owing to a small number of cases. Third, because of the time interval of up to 27 months between US and MRI, we cannot exclude the possibility that some thyroid nodules changed in size, shape, or number during this period. Finally, results may vary because other institutions may employ different MRI or US machines and may use different routine parameters of C-T sag T2WI such as FOV or matrix size.
In conclusion, there were limits to the reliability of thyroid nodule detection by C-T sag T2WI; very few thyroid nodules < 1 cm in size and only one-third of the nodules > 1 cm were detected by the sequence. But if once an incidental thyroid nodule is seen by C-T sag T2WI, it is more likely a > 1-cm solid hypoechoic or mixed echoic nodule with relatively more malignant potential rather than a < 1-cm solid isoechoic or spongiform nodule. For this reason, in that case, we suggest that it would be better to recommend thyroid US for identifying malignancy than not to do so.
Figures and Tables
Fig. 1
A 65-year-old woman with a 12-mm right thyroid nodule. (a) Thyroid US reveals an unparalleled solid hypoechoic thyroid nodule with microcalcifications, which is suspicious for malignancy. The nodule was diagnosed as benign by fine needle aspiration biopsy. (b) After 3 months, C-T sag T2WI of lumbar spine MRI for evaluation of lower back pain shows a T2-high signal intensity nodule in the thyroid (arrow).

Fig. 2
A 74-year-old woman with a 25-mm right thyroid nodule. (a) The thyroid nodule shows mixed solid and cystic composition in the US. (b) C-T sag T2WI of lumbar spine MRI two days later shows a nodule with cystic component in the thyroid (arrow). It can be mistaken for a much smaller nodule in the MR images.
Fig. 3
Undetected > 1-cm thyroid nodules. (a, b) A spongiform thyroid nodule of a 55-year-old woman. (c, d) A solid isoechoic thyroid nodule of a 56-year-old woman. These nodules were not identified by C-T sag T2WI of lumbar spine MRI.

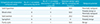
Table 1
Detection Rate for Thyroid Nodules by C-T sag T2WI of L-spine MRI, correlating with Thyroid US

Table 2
Echogenicity and Composition of > 1-cm Thyroid Nodules detected by US and C-T sag T2WI of L-spine MRI
References
1. Kamath S, Jain N, Goyal N, Mansour R, Mukherjee K. Incidental findings on MRI of the spine. Clin Radiol. 2009; 64:353–361.
2. Grady AT, Sosa JA, Tanpitukpongse TP, Choudhury KR, Gupta RT, Hoang JK. Radiology reports for incidental thyroid nodules on CT and MRI: high variability across subspecialties. AJNR Am J Neuroradiol. 2015; 36:397–402.
3. Nam-Goong IS, Kim HY, Gong G, et al. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endocrinol (Oxf). 2004; 60:21–28.
4. Kang HW, No JH, Chung JH, et al. Prevalence, clinical and ultrasonographic characteristics of thyroid incidentalomas. Thyroid. 2004; 14:29–33.
5. Kim K, Emoto N, Mishina M, et al. Incidental detection of thyroid nodules at magnetic resonance imaging of the cervical spine. Neurol Med Chir (Tokyo). 2013; 53:77–81.
6. Seo J, Park SY, Lee JW, Lee GY, Kang HS. The value of additional cervicothoracic spine sagittal T2-weighted images included in routine lumbar spine MR imaging. J Korean Soc Magn Reson Med. 2013; 17:91–100.
7. Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association (ATA) guidelines taskforce on thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.
8. Kwak JY, Han KH, Yoon JH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology. 2011; 260:892–899.
9. Serpell J. Management guidelines for patients with thyroid nodules. ANZ J Surg. 2010; 80:765–766.
10. Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006; 16:109–142.
11. Kamran SC, Marqusee E, Kim MI, et al. Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab. 2013; 98:564–570.
12. Wong KT, Ahuja AT. Ultrasound of thyroid cancer. Cancer Imaging. 2005; 5:157–166.
13. Moon WJ, Jung SL, Lee JH, et al. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008; 247:762–770.
14. Lee MJ, Kim EK, Kwak JY, Kim MJ. Partially cystic thyroid nodules on ultrasound: probability of malignancy and sonographic differentiation. Thyroid. 2009; 19:341–346.
15. Bellantone R, Lombardi CP, Raffaelli M, et al. Management of cystic or predominantly cystic thyroid nodules: the role of ultrasound-guided fine-needle aspiration biopsy. Thyroid. 2004; 14:43–47.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download