INTRODUCTION
Craniofacial resection (CFR) for anterior skull-base tumors has been used for about 30 years as a general surgical procedure since its original description [
1]. Classical CFR consists of transfacial/transnasal and transcranial approaches. Recently, the endonasal approach using the endoscope, substitutive for the open transfacial approach, has been used as a universal surgical route. Furthermore, due to the development of the endoscope technique and instruments, a pure endoscopic approach, without a transcranial approach, has been attempted for tumor removal in the anterior skull base [
2].
Although the pure endoscopic approach has been comprehensively compared with the classical traditional combined approach, there are many differences between the two groups of patients, and many constraints on the accurate comparison of the surgical results [
3]. One study used purely endoscopic approach for the lesions without definitive invasion into skull base [
4]. The study was limited by patient selection in being able to compare the surgical results of the classic CFR with the endoscopic techniques. Also, surgical outcomes by transcranial approach have recently improved as the result of advancement in microsurgical instruments and techniques.
In the light of these advancements, there is a need to re-evaluate the indications of CFR with endoscopic approach. The purpose of this study is to evaluate the surgical results for CFR in our hospital with the review of the recently published data.
MATERIALS AND METHODS
This study fulfilled all the requirements for patient anonymity and was approved by the Institutional Review Board (MP 2015-010). From 2001 to 2012, 17 patients underwent CFR for anterior skull-base malignancies in our hospital. The benign pathologic case was excluded. The medical records were evaluated for patient demographics, clinical features, staging, preoperative treatment, operative procedure, extent of tumor extension, postoperative complication, follow-up, recurrence rate, and survival rate. Mean follow-up duration was 41 months (range, 2-103 months).
Based on the preoperative computed tomography scan and/or magnetic resonance imaging and intraoperative findings, the exact location of tumor and its extension into orbit or intracranial structures were evaluated. The tumors were classified according to both the Kadish and Biller staging systems. The Kadish staging system describes three stages to determine the location and extension of olfactory neuroblastoma [
4]: Stage A: tumor confined to the nasal cavity; Stage B: tumor confined to the nasal cavity and one or more paranasal sinus; and Stage C: tumor extending beyond the nasal cavity or paranasal sinuses, and includes involvement of the orbit, base of skull, or intracranial extension. The Biller staging system has four stages to determine the location and extension of remaining other tumors [
5]. T1 stage is defined as a tumor involving the nasal cavity and adjacent paranasal sinuses (excluding sphenoid), with or without erosion of the bone of the anterior cranial fossa. T2 stage is defined as a tumor extending into the periorbital tissue or protruding into the anterior cranial fossa. T3 stage is defined as a tumor involving the brain that is resectable with margins. T4 stage is defined as a non-resectable tumor. All specimens were examined in our pathology department.
Overall survival (OS) was calculated from the date of surgery until death, or until the date of the last follow-up visit for patients who were still alive. Relapse-free survival (RFS) was also calculated as the time from the date of surgery to the date of recurrence or death. Survival rate was analyzed by the Kaplan-Meier method and compared with the log-rank test. For the multivariate analysis, independent prognostic factors were determined using the Cox's proportional hazards model. The statistical analysis was performed using SPSS version 20.0 software program for Windows (SPSS Inc., Chicago, IL, USA). The level of significance was set at p<0.05.
RESULTS
Patient demographics and clinical symptoms at the time of initial diagnosis are listed in
Table 1. The most common symptoms were epistaxis and nasal obstruction. Two patients with paranasal malignancies underwent radiochemotherapy before CFR. The median age was 56 years (range, 34-74 years) and male to female ratio was 12 to 5. The most common pathological type was squamous cell carcinoma (6 patients). Tumors invaded only in the cribriform plate in 5 patients, extended through dura in 4 patients, and involved brain parenchyma in 7 patients. Orbit involvement was noted in 6 patients. All olfactory neuroblastomas were classified as stage C of the Kadish system. Majority of the remaining tumors were classified as T3 or T4 of the Biller classification system.
Classical bifrontal craniotomy was combined with endoscopic endonasal approach in 14 patients. External approach was used in 3 patients with severe orbital involvement for orbital exenterating (
Table 2). Reconstruction of the anterior fossa floor was performed using vascularized flap in 16 patients (94%). Apart from 3 cases requiring free flap after orbital exenterating, the remaining 13 cases underwent nasoseptal flap. Gross total resection was achieved in all cases. Four patients (20%) experienced postoperative complications including local wound problem [3 patients; 2 with cerebrospinal fluid (CSF) leakage] and brain abscess (1 patient). One patient with liver cirrhosis died from unexpected varix bleeding. Although postoperative treatment such as radiotherapy or chemotherapy was performed in 14 patients, local recurrence was seen in 6 patients (35%).
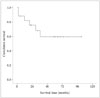
The mean OS time after CFR of anterior skull base tumors was 69.0 months [95% confidence interval (CI): 47.5-90.5 months, the median survival time was not reached]. One-, 2-, and 5-year survival rate was 82.3%, 76.5%, and 64.7%, respectively (
Fig. 1). The results of analyses of the variables that could be correlated with OS are shown in
Fig. 2 and
Table 3. On univariate and multivariate analysis, postoperative radiotherapy was significantly related with survival time.
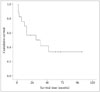
In a view of RFS, the mean RFS time after the operation was 47.1 months (95% CI: 25.9-68.4 months, the median survival time was 30.0 months). One-, 2-, and 5-year RFS rate was 64.7%, 47.1%, and 30.7%, respectively (
Fig. 3). On univariate and multivariate analysis, postoperative radiotherapy was also significantly related with RFS time (
Fig. 4,
Table 4). Considering the small number of this study, however, pathologic type showed somewhat relationship with OS (
p=0.057) and RFS (
p=0.053) after the operation.
DISCUSSION
Anterior CFR has remained the gold standard for the management of tumors involving the anterior skull base. The addition of postoperative radiation with or without chemotherapy has shown a favorable effect on treatment result of advanced malignancies of the paranasal sinus extending to the anterior skull base [
6]. The continuous improvement in endoscopic surgical instrumentation led to the advance of endoscopic-assisted CFR for sinonasal malignancies [
7]. In recent years, there has been increasing popularity of purely endoscopic resection of malignant tumors involving the anterior skull base [
289]. Resection should be radical, regardless of approach modalities for the lesion, because patients with local relapse after previous treatment have a worse prognosis [
2].
Because of the relative rarity of anterior CFR, there are few centers that treated adequate numbers of patients for meaningful analysis of outcomes [
10]. In an effort to overcome these difficulties, an international collaborative study on craniofacial surgery for malignant skull base tumors collected data from 1,307 patients in 2003. With a median follow-up of 25 months, the 5-year overall, disease-specific, and recurrence-free survival rate was 54%, 60%, and 53%, respectively [
11]. Tumor-related variables, such as the histological variation, intracranial tumor extent, status of surgical margin, and postoperative complication, influence outcomes [
1112]. Many studies of CFR have reported postoperative complications as high as 40%, and postoperative mortality rate has remained about 5% [
111213]. According to the literatures, complications after CFR includes CSF leakage, frontal pneumocephalus, local wound infection, meningitis and disturbance of central nervous systems. The CSF leakage, wound infection, meningitis occurred more frequently than other complications. The CSF leakage was recovered with conservative treatment but wound infection and meningitis were fatal requiring invasive antibiotics or reoperation [
91014]. These surgical limitations have prompted the search for more safe approaches to the anterior skull base [
9]. Endonasal techniques are thought to offer several advantages. When compared to the traditional anterior CFR, the use of pure endonasal endoscopic resection is associated with a decreased blood loss, benefit of a desirable cosmetic outcome and faster recovery [
9]. Comparing the results of traditional CFR with pure endoscopic resection continues to be difficult because most published reports on exclusive endoscopic approach resection include small case series of patients with a short follow-up [
10]. In addition, Hanna et al. [
2] treated with exclusive endoscopic approach only patients with earlier disease stage with limited or no skull base involvement. As the interest of endoscopic resection of tumors involving the anterior skull base increases, concurrent improvements in traditional techniques are occurring [
3]. The traditional anterior CFR and the endoscopic resection might not be two opposing techniques, but two useful methods to achieve the goal of a safe and radical resection when they were properly applied [
10].
In order to better understand the role of CFR, we assessed our surgical outcomes in the context of recently published series [
31014]. Previously reported 5-year OS rate, gross total resection rate, complication rate are 46-72%, 98-100%, and 9.7-47%, respectively (
Table 5). Histology, extent of intracranial involvement, increasing age, incomplete tumor removal, and staging were associated with poor survival outcome [
101516]. The status of the surgical margins is an important predictor for overall, disease-specific, and recurrence-free survival [
14]. The histological finding of the primary tumor and extent of intracranial involvement is also a significant predictor of overall, disease-specific, and recurrence-free survival [
1217]. Increased age was reported as a risk factor for poor survival [
14]. In our study, postoperative radiotherapy was significant predictor for longer OS and RFS. Neuroblastoma type seemed to be related with prolonged OS and RFS, compared to other pathologies.
In conclusion, this study was basically a retrospective investigation of a relatively small number of patients, possibly leading to selection bias. Although there are limitations in number of cases and follow-up duration, our study shows that CFR followed by adjuvant radiotherapy can remain the primary option for malignant tumors involving anterior skull base, especially with intracranial extension.











 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download