Abstract
The cerebellar infarction resulting from supratentorial craniotomy is uncommon event and its management has been controversial. After removal of space occupying lesion on right frontal area, two cases of remote cerebellar infarctions occurred. We reviewed each cases and the techniques to manage such complications are discussed. Early extraventricular catheter insertion and midline suboccipital craniectomy were effectively performed in obtunded patients from cerebellar infarction.
Intracranial hemorrhage (ICH) and infarction are two of the most important complications following neurosurgery, as they can completely change the course of a disease or the treatment plan. While cerebellar hemorrhage from supratentorial brain surgery or spinal surgery has frequently been reported [123456], cerebellar infarction from supratetorial surgery has not been documented.
Surgical treatments for patients with cerebellar infarction, like suboccipital decompression or extraventricular drainage (EVD) catheter insertion, are known as effective treatments [78910]. For its slow aggravation of cerebellar infarction compared to hemorrhagic counterparts, the timing and the extent of surgery are still controversial [81011]. As there are no randomized controlled study on cerebellar infarction, we still make analogy on this topic from studies of general cerebral infarction [1213141516] and traumatic brain injury [17]. In addition to the benefit of the surgery itself, early craniectomy is another trend leading this field [1218].
Two cases of remote cerebellar infarction from supratentorial neurosurgery, who survived and recovered after early decompressive craniectomy and EVD catheter insertion, are reviewed and technical aspects of the surgical management of cerebellar infarction are discussed.
A 66-year-old female patient who was diagnosed with cerebral infarction in the right frontal lobe presented to our clinic complaining of a mild headache. She had existing diagnoses of hypertension and diabetes mellitus. Her family history was notable in that both parents died from ischemic stroke, one brother had liver cancer and four sisters had hypertension and diabetes mellitus.
As the mass was suggestive of a malignant brain tumor on magnetic resonance (MR) contrast images (Fig. 1A), we decided to confirm the pathology by surgical exploration following a decision by the patient's caregivers, and the mass was removed completely. The consistency of the mass was sticky without significant internal necrosis. We used gliolan, and uptake in the lesion was observed on intraoperative fluorescent imaging (Fig. 1C). After surgery, the patient awoke from anesthesia without any neurologic deficits and was discharged from the neurosurgical intensive care unit (NCU) soon after extubation.
Three days after the operation, the patient complained of nausea and intermittent vomiting accompanied by increased heart rate up to 150 bpm, and electrocardiography showed paroxysmal atrial fibrillation without any change in blood pressure.
The patient had persistent nausea and a mild headache that developed after the operation, but these symptoms were not believed to be caused from complications of the surgery.
Sequential neurologic exams showed progressive obtundation and she finally became stuporous with a greatest response to stimuli of withdrawal of extremities [National Institutes of Health Stroke Scale (NIHSS)=30, Glasgow Coma Scale (GCS)=8, Pupil right/left=bilaterally 3 mm prompt]. An emergency CT scan showed hydrocephalus originating from a compressed 4th ventricle as the bilateral posterior inferior cerebellar artery (PICA) territory infarction progresses (Fig. 1D).
Immediate decompression of the posterior fossa was performed in the prone position. As the brainstem was relatively relaxed from the preoperative CT scan, EVD at the left Frazier's point was initiated first as the dullness seemed to originate from acute hydrocephalus (Fig. 1E). The opening pressure was slightly elevated [18 cm cerebrospinal fluid (CSF)], and good pulsatile oscillation was observed from the CSF.
Suboccipital decompression was performed as the swelling was expected to progress. Her serial follow-up CT image showed compression of brain stem even after the decompressive craniectomy suggesting the benefit of early management (Fig. 1F).
A 57-year-old female with a history of hypertension and diabetes mellitus but no stroke history presented to our hospital for subjective weakness of her left extremities. Her MR scan showed a hypervascular 5.3×4.7 cm mass in the right parasagittal area on contrast-enhanced T1 image (Fig. 2A). She obtained her digital subtracted angiography for its hypervascularity of the tumor from MR angiography and for consideration of embolization of the mass. During the procedure, bilateral middle meningeal arteries and bilateral anterior cerebral arteries were feeding the tumor (Fig. 2B) and left middle meningeal artery was selected for particle embolization to minimize intraoperative bleeding. She was prepared for a craniotomy with a preoperative diagnosis of hemangiopericytoma.
At the time of surgical resection, tumor was surrounded by large vessels (Fig. 2C) and the blood loss was not negligible (2,800 cc over 9 hours), and the volume loss was replaced by both blood transfusion and fluid resuscitation. Right after the operation, CT showed no abnormality except remaining peritumoral edema.
The pathologic report showed the mass was hemangiopericytoma (World Health Organization grade II) with Ki-67 labeling index 8%. Immunohistochemical results were cluster of differentiation 34 positive, epithelial membrane antigen focal positive, and progesterone negative.
She was drowsy after the operation and no other remarkable findings were found from serial neurologic examination that was performed in one hour period. Twenty-four hours later, she was sent for postoperative MR brain scan. Right dominant bilateral cerebellar infarction in PICA territory with acute hydrocephalus was diagnosed (Fig. 2D), which was not seen on the previous CT scan.
This alert patient became drowsy after the tumor removal of supratentorial mass (NIHSS=5, GCS=13, Pupil right/left=2 mm prompt bilaterally). Neurologic scores progressed to become deep drowsy status (NIHSS=17, GCS=11, Pupil right/left=2 mm prompt bilaterally) and respiratory distress required intubation while the patient was in NCU before the decompression.
As the patient's mental status deteriorated from drowsy to deeply drowsy, we performed an EVD catheter insertion at right Frazier's point (Fig. 2E). Opening pressure was not measured for its quick and explosive drainage at the time of insertion of the catheter. Draining CSF frequently, decompressive suboccipital craniectomy was approached from midline (Fig. 2F).
Although incidence of postoperative cerebellar infarction after supratentorial craniotomy is not known, the number of such complications requiring decompressive surgery should be limited for several reports of good outcome after medical management in selected patients [810]. However, cerebellar infarction cases should be considered as possible surgical candidates requiring early management on the new basis for decompressive craniectomy [1216] while the progression of disease is much slower than its hemorrhagic counterpart.
The principle of the treatment of cerebellar infarction is focused on sufficient decompression of the posterior fossa and the prevention of possible neurologic deficits from hydrocephalus or brain herniation; such techniques mostly lead to a good outcome [19]. Both of our cases showed altered mental status, which required surgery to manage the acute phase of the complication.
We treated both cases by first inserting an EVD catheter followed by midline approach suboccipital decompression. Upward herniation might come from excessive drainage of CSF and some authors warned of such complication necessitating suboccipital craniectomy should be done early [820]. As the recognition of obtunded patient was immediate after the event and the decision of opening up posterior fossa was prompt, the extent of swelling of cerebellum should have been minimal while the deteriorations of the patient were regarded as a result from acute hydrocephalus by narrowed distal CSF pathways. However the opening pressures from both patients were not detrimental (about 10-15 cm CSF). After resolution of the hydrocephalus, the next step was posterior fossa decompression. Intermittent intraoperative drainage of EVD should have maintained stable intracranial pressure.
In both cases, our patients had bilateral stroke on their cerebellum mandating bilateral decompression. Although hockey stick shaped incision could be facilitated for suboccipital decompression, midline approach was used to cover both sides of cerebellum. A curvilinear incision over the midline is made to promote postoperative wound recovery. An incision extending from 2-3 cm above inion down to C2 level was scored and dilated using self-retaining cerebellar retractor. Preoperative measurement for sufficient decompression of posterior fossa was validated using a ruler. After demarcation of the area for craniectomy, two burr holes were placed just under the inion 1 cm from midline symmetrically to avoid possible sinus bleeding. Bony segment between burr holes were thinned using match-head drill and thin layer of the bone was remained for completion with Kerrison rongeurs of 45 degree.
CSF overdrainage has frequently been associated with complications of the cerebellar region [321]. ICH in the cerebellum after brain surgery or spinal surgery is thought to be caus-ed by the loss of excessive CSF volume. Hemorrhagic infarc-tion has also been regarded as a complication of CSF over-drainage [22]. In each of our cases, however, the volume of CSF leakage was not substantial and cerebellar infarction still occurred. Our hypothesis that, the cerebellar infarction was caused by anomalies in vascular structure, is still speculative and difficult to prove (Table 1).
In case 1, the patient had both hypertension and diabetes mellitus, but coronary artery occlusive disease was not a definitive diagnosis at the time of surgery. The patient experienced a sudden increase in heart rate accompanied by slightly decreased systolic blood pressure. We are unsure whether the cardiac condition preceded the ischemic changes or if sudden ischemic changes in the cerebellum caused paroxysmal atrial fibrillation with rapid ventricular response. Preoperatively, although we had digitally subtracted images of the cerebral vessels, the right vertebral artery injection image was not taken and there was no PICA from left vertebral artery injection (Fig. 1B) suggesting anomalous distribution of the right PICA in the bilateral cerebellum. In case 2, massive blood loss occurred during the operation. This patient also had a history of hypertension and diabetes mellitus. Preoperative MR angiography showed hypervascularity of the tumor mass, bilateral fetal-type posterior communicating arteries, and decreased posterior circulation (Fig. 2B). We managed massive hemorrhage during the operation from the feeding arteries of the hemangiopericytoma in good cooperation with anesthesiologists. Although the immediate postoperative CT scan was clear without any evidence of cerebellar infarction, hemodynamic instability after such bleeding might have played a role in the development of cerebellar infarction.
Minimizing changes inside the brain and related environment seems essential to avoid complications. Several authors report excessive blood loss during neurosurgery causes cerebellar hemorrhage [22123]. In our case, continued blood loss from a hemangiopericytoma could have caused such a complication. Sometimes oozing without sufficient coagulation can lead to an underestimation of blood loss, placing the patient in danger.
In conclusion, remote cerebellar infarction could occur after supratentorial craniotomy. Understanding the possibility of remote cerebellar infarction from a surgery of supratentorial mass can help making decisions from clinical practice. Even when this complication occurs, in selected cases, early EVD catheter insertion followed by suboccipital craniectomy can help patients survive and recover back to good condition.
Figures and Tables
Fig. 1
Neuroimaging studies. A: MRI, contrast enhancing mass in the right frontal area. B: Digital subtraction angiography, there were no right vertebral artery injection images, and the PICA territory was not evaluated for feeder vessels. C: Gliolan fluorescent intraoperative image showing a red glowing mass inside a cavity. D: Postoperative CT, bilateral PICA territorial infarction accompanying acute hydrocephalus. E: Postoperative CT, decreased ventricle size after insertion of the EVD. F: CT, midline suboccipital craniectomy. PICA, posterior inferior cerebellar artery; EVD, extraventricular drainage.

Fig. 2
Neuroimaging studies. A: MR, a brain tumor in the right frontal parasagittal area. B: Digital subtraction angiography, hypervascular tumor with feeder vessels from the anterior cerebral artery. C: Intraoperative imaging of the tumor shows engorged vessels around the mass. D: Postoperative MR scan showing bilateral PICA and AICA territory infarctions. E: Postoperative CT with decreased ventricle size after insertion of the EVD. F: CT, swollen cerebellum compressing the brain stem. AICA, anterior inferior cerebellar artery; PICA, posterior inferior cerebellar artery; EVD, extraventricular drainage.
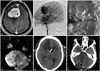
Table 1
General information of each patient

References
1. Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F, Post KD. Intracerebral hemorrhage occurring remote from the craniotomy site. Neurosurgery. 1996; 39:1114–1121. discussion 1121-2

2. Cavanilles-Walker JM, Tomasi SO, Sgier F, Kröber M. Remote cerebellar haemorrhage after lumbar spine surgery: case report. Arch Orthop Trauma Surg. 2013; 133:1645–1648.

3. Ha SH, Kim EM, Ju HM, Lee WK, Min KT. Remote cerebellar hemorrhage after unruptured cerebral aneurysm surgery: two cases report. Korean J Anesthesiol. 2014; 67:213–216.

4. Karaeminogullari O, Atalay B, Sahin O, et al. Remote cerebellar hemorrhage after a spinal surgery complicated by dural tear: case report and literature review. Neurosurgery. 2005; 57:1 Suppl. E215. discussion E215.

5. Morofuji Y, Tsunoda K, Takeshita T, et al. Remote cerebellar hemorrhage following thoracic spinal surgery. Neurol Med Chir (Tokyo). 2009; 49:117–119.
6. Konya D, Ozgen S, Pamir MN. Cerebellar hemorrhage after spinal surgery: case report and review of the literature. Eur Spine J. 2006; 15:95–99.

7. Ivamoto HS, Numoto M, Donaghy RM. Surgical decompression for cerebral and cerebellar infarcts. Stroke. 1974; 5:365–370.

8. Chen HJ, Lee TC, Wei CP. Treatment of cerebellar infarction by decompressive suboccipital craniectomy. Stroke. 1992; 23:957–961.

9. Rieke K, Krieger D, Adams HP, Aschoff A, Meyding-Lamade U, Hacke W. Therapeutic Strategies in Space-Occupying Cerebellar Infarction Based on Clinical, Neuroradiological and Neurophysiological Data. Cerebrovasc Dis. 1993; 3:45–55.

10. Baldauf J, Oertel J, Gaab MR, Schroeder HW. Endoscopic third ventriculostomy for occlusive hydrocephalus caused by cerebellar infarction. Neurosurgery. 2006; 59:539–544. discussion 539-44

12. Vahedi K, Hofmeijer J, Juettler E, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007; 6:215–222.

13. Frank JI, Schumm LP, Wroblewski K, et al. Hemicraniectomy and durotomy upon deterioration from infarction-related swelling trial: randomized pilot clinical trial. Stroke. 2014; 45:781–787.

14. Ropper AH. Hemicraniectomy--to halve or halve not. N Engl J Med. 2014; 370:1159–1160.
15. Jüttler E, Unterberg A, Woitzik J, et al. Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke. N Engl J Med. 2014; 370:1091–1100.

16. Vahedi K, Vicaut E, Mateo J, et al. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007; 38:2506–2517.

17. Cooper DJ, Rosenfeld JV, Murray L, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011; 364:1493–1502.

18. Cho DY, Chen TC, Lee HC. Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction. Surg Neurol. 2003; 60:227–232. discussion 232-3

19. Mathew P, Teasdale G, Bannan A, Oluoch-Olunya D. Neurosurgical management of cerebellar haematoma and infarct. J Neurol Neurosurg Psychiatry. 1995; 59:287–292.

20. Seelig JM, Selhorst JB, Young HF, Lipper M. Ventriculostomy for hydrocephalus in cerebellar hemorrhage. Neurology. 1981; 31:1537–1540.

21. You SH, Son KR, Lee NJ, Suh JK. Remote cerebral and cerebellar hemorrhage after massive cerebrospinal fluid leakage. J Korean Neurosurg Soc. 2012; 51:240–243.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download