Abstract
Purpose
Children admitted to pediatric intensive care unit (PICU) with respiratory tract disease, often have a tendency to be readmitted to PICU with disease progression. We studied the risk factors for readmission to PICU, with respiratory disease progression.
Methods
Among 286 children admitted to Seoul St. Mary's Hospital PICU from April 2009 to March 2012, 129 children admitted with respiratory tract disease were enrolled. We grouped the children readmitted to PICU with respiratory tract disease progression within 2 weeks (readmission group), and the others (control group). We compared basic and respiratory tract disease characteristics at initial PICU admission between them, by retrospective chart review.
Results
Among 129 children, 8 were included in the readmission group, and 121 in the control group. Mortality and underlying disease incidence were higher in the readmission group (P=0.003 and P=0.033, respectively). The readmission group showed higher parenchymal lung disease incidence, and lower initial saturation by pulse oxymeter (SpO2)/fraction of inspiratory oxygen (FiO2), despite underlying disease influence (P=0.035 and P=0.041, respectively). Logistic regression on the underlying disease and respiratory variables showed no single factor with a significantly independent influence on readmission, but parenchymal lung disease had more independent influence.
Conclusion
For PICU readmission with respiratory tract disease progression, parenchymal lung disease and lower initial SpO2/FiO2 can be a risk factor despite underlying disease influence. Underlying disease and each respiratory characteristic were not significantly independent risk factors, suggesting a correlation of factors. But, parenchymal lung disease can be a more independent risk factor.
Figures and Tables
Fig. 1
Outline of participants of our study. Among 286 patients admitted to pediatric intensive care unit (PICU), 129 admitted with respiratory tract disease were enrolled. There was no patient died in first PICU admission. Of course, 8 patients readmitted to PICU with respiratory tract disease progression within 2 weeks were compared with the other 121 patients for clinical characteristics.

Table 1
The comparison of basic clinical characteristics, incidence of mortality and underlying disease at initial PICU admission between readmission group and control group
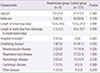
Table 2
The comparison of characteristics of respiratory tract disease at initial PICU admission between readmission group and control group and those according to underlying disease existence

References
1. Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010; 38:65–71.

2. Kahn JM. Understanding economic outcomes in critical care. Curr Opin Crit Care. 2006; 12:399–404.

3. Bone RC, McElwee NE, Eubanks DH, Gluck EH. Analysis of indications for early discharge from the intensive care unit. Clinical efficacy assessment project: American College of Physicians. Chest. 1993; 104:1812–1817.

4. Swann D, Houston P, Goldberg J. Audit of intensive care unit admissions from the operating room. Can J Anaesth. 1993; 40:137–141.

5. Wagner DP, Knaus WA, Draper EA. Identification of low-risk monitor admissions to medical-surgical ICUs. Chest. 1987; 92:423–428.

6. Rosenberg AL, Watts C. Patients readmitted to ICUs*: a systematic review of risk factors and outcomes. Chest. 2000; 118:492–502.
7. Odetola FO, Clark SJ, Dechert RE, Shanley TP. Going back for more: an evaluation of clinical outcomes and characteristics of readmissions to a pediatric intensive care unit. Pediatr Crit Care Med. 2007; 8:343–347.

8. Brown SE, Ratcliffe SJ, Kahn JM, Halpern SD. The epidemiology of intensive care unit readmissions in the United States. Am J Respir Crit Care Med. 2012; 185:955–964.

9. Yoon KB, Koh SO, Han DW, Kang OC. Discharge decision-making by intensivists on readmission to the intensive care unit. Yonsei Med J. 2004; 45:193–198.

10. Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical intensive care unit: patient profiles and possibilities for prevention. Crit Care Med. 1985; 13:961–964.
11. Frost SA, Alexandrou E, Bogdanovski T, Salamonson Y, Davidson PM, Parr MJ, et al. Severity of illness and risk of readmission to intensive care: a meta-analysis. Resuscitation. 2009; 80:505–510.

12. El Halal MG, Barbieri E, Filho RM, Trotta Ede A, Carvalho PR. Admission source and mortality in a pediatric intensive care unit. Indian J Crit Care Med. 2012; 16:81–86.

13. Namachivayam P, Shann F, Shekerdemian L, Taylor A, van Sloten I, Delzoppo C, et al. Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med. 2010; 11:549–555.

14. Campbell AJ, Cook JA, Adey G, Cuthbertson BH. Predicting death and readmission after intensive care discharge. Br J Anaesth. 2008; 100:656–662.

15. Han DW, Nam SB, Lee WK, Lee JS, Kim CS, Shin CS. Clinical outcomes of patients readmitted to intensive care unit. Korean J Anesthesiol. 2004; 47:385–388.

16. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994; 149(3 Pt 1):818–824.

17. Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, de Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ. 2005; 83:353–359.
18. Baigelman W, Katz R, Geary G. Patient readmission to critical care units during the same hospitalization at a community teaching hospital. Intensive Care Med. 1983; 9:253–256.

19. Durbin CG Jr, Kopel RF. A case-control study of patients readmitted to the intensive care unit. Crit Care Med. 1993; 21:1547–1553.

20. Kaben A, Correa F, Reinhart K, Settmacher U, Gummert J, Kalff R, et al. Readmission to a surgical intensive care unit: incidence, outcome and risk factors. Crit Care. 2008; 12:R123.

21. Chen LM, Martin CM, Keenan SP, Sibbald WJ. Patients readmitted to the intensive care unit during the same hospitalization: clinical features and outcomes. Crit Care Med. 1998; 26:1834–1841.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download