Abstract
Objective
Preventable and potentially preventable traumatic death rates is a method to evaluate the preventability of the traumatic deaths in emergency medical department. To evaluate the preventability of the traumatic deaths in patients who were admitted to neurosurgery department, we performed this study.
Methods
A retrospective review identified 52 patients who admitted to neurosurgery department with severe traumatic brain injuries between 2013 and 2014. Based on radiologic and clinical state at emergency room, each preventability of death was estimated by professional panel discussion. And the final death rates were calculated.
Results
The preventable and potentially preventable traumatic death rates was 19.2% in this study. This result is lower than that of the research of 2012, Korean preventable and potentially preventable traumatic death rates. The rate of preventable and potentially preventable traumatic death of operation group is lower than that of conservative treatment group. Also, we confirmed that direct transfer and the time to operation are important to reduce the preventability.
Conclusion
We report the preventable and potentially preventable traumatic death rates of our institute for evaluation of preventability in severe traumatic brain injuries during the last 2 years. For decrease of preventable death, we suggest that continuous survey of the death rate of traumatic brain injury patients is required.
In the severe trauma patients, the process of initial treatment, transfer and evaluations are very important for the prognosis of patients, including death. The concept of "preventable and potentially preventable traumatic death rates" is a way to evaluate that process.10) The approach by the rate of preventable and potentially preventable traumatic death mathematically determines whether a death of a patient was preventable in comparison with the ideal case where traumatic patients are transferred to hospitals within a proper time limit and receive optimal treatment. This allows the treatment of a trauma patient to be evaluated, pointing out problems.7) The preventable death rate were researched three times in South Korea. According to the research of Kim et al.,7) in 2009 and 2010, 45.7% of all deaths of severe traumatic patients in South Korea were caused by traumatic brain injury (TBI). This indicates that departments of neurosurgery treat a larger proportion of trauma patients than any other department, and therefore evaluation of their treatment adequacy is important. This study examined the preventable and potentially preventable traumatic death rates of patients who had died from severe TBI between 2013 and 2014 in our institute. Authors discussed how to reduce the traumatic death rates.
The subjects of this study were 52 patients who had died in 2013 and 2014 after being hospitalized for neurosurgery treatment via emergency room due to severe traumatic injuries in our institution. The exclusion criteria of patients was as follows: 1) no sufficient hospital information and inability to decide the preventability of death, 2) no diagnostic tests before death of discharge, or 3) death during transport from other hospital after diagnosis of brain injuries.
Most studies on preventable death rate are based on clinical and radiological imaging findings, and the final decision of the preventable and potentially preventable traumatic death is mainly by professional panel consensus discussion.24) Similar to previous studied, professional panel consensus discussions were performed for evaluation of the preventability.
In this study, two neurosurgeons and one thoracic surgeon were designated to evaluate the severity of injury, the state of patients upon arrival at the emergency room, and the appropriateness of treatment. We also examined the probability of survival (Ps) of trauma score and the injury severity score (TRISS), which evaluates the subjects' sex, age, the incident mechanism, whether death was caused by head trauma, and the severity of injury.1) The Ps of TRISS was calculated by using the Abbreviated Injury Scale (AIS) and Revised Trauma Score (RTS). Based on the severity of the injury and the state of the patient, when the AIS score was 6, or at least two of the following conditions were applicable, the death was judged as non-preventable death first, when the AIS score at diagnosis was 5, and the Ps was less than 50%; second, upon admission to the hospital, the patient's RTS was less than 6, and their Ps was less than 50%; and third, the patient had a serious underlying disease (chronic renal failure, liver cirrhosis, etc.), or the patients' cause of death was acute myocardial infarction or pulmonary thromboembolism. In addition, patients who refuse further treatment or signed the do not resuscitate (DNR) order were classified as non-preventable death. When the possibility of resuscitation was at least 75%, it was judged as a preventable death; when the possibility of resuscitation was 25% to 75%, it was judged to be a potentially preventable death; when the possibility of resuscitation was less than 25%, it was judged to be a non-preventable death. The final preventable and potentially preventable traumatic death rates was defined as percentage of all cases of potentially preventable death and preventable death.9)
Enrolled cases were classified into two categories according to stage of treatment process: overall preventability and hospital preventability. Overall preventability refers to the combination of preventable death at pre-hospitalization stage and the hospitalization stage. The preventable death and potentially preventable death at pre-hospitalization stage is judged based on initial treatment and transporting to suitable hospital within reasonable time. We evaluated the preventable death at pre-hospitalization stage to analyze relation of death rate, transference time and direct transporting to our hospital. We determined the preventable death and potentially preventable death at hospitalization stage by analyzing the survival possibility in the process of treatment at emergency room, operation room, intensive care unit and ward. Each stage problems were analyzed in accordance with the table of the previous studies.7) The problem is defined only in relation to the death directly.
We analyzed the preventable death rate whether performed surgery and transferred directly. Also, we compared this study with the research of 2012, Korean preventable and potentially preventable traumatic death rates. Statistical methods were noted in the following tables. All p-values of less than 0.05 were considered to indicate statistical significance. All statistical analyses were conducted with the use of statistical software package SPSS (Version 24.0; SPSS, Inc., Chicago, IL, USA).
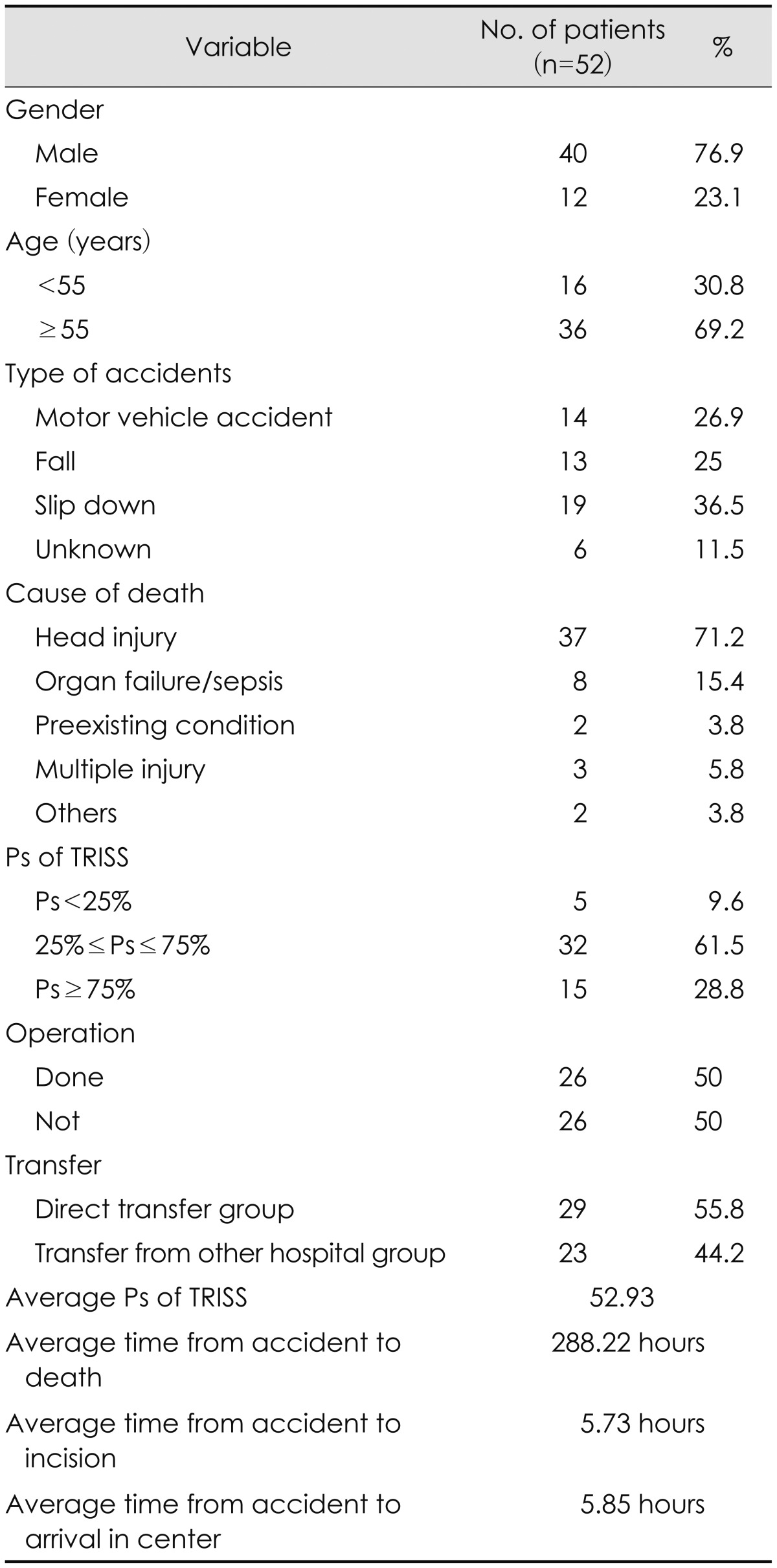
The average age of the patients was 63.2±19.75 years (range, 10-88 years). There were 40 males and 12 females. Among the subjects' incident mechanisms, slipping down accounted for 19 patients, traffic accidents for 14, falling for 13, and unknown for 6. The number of patients whose Ps of TRISS were less than 25% was 5, and 32 patients, between 25 and 75%, and 15 patients, above 75%. Among 52 patients, 26 underwent brain surgery, and 26 were treated conservatively (Table 1).
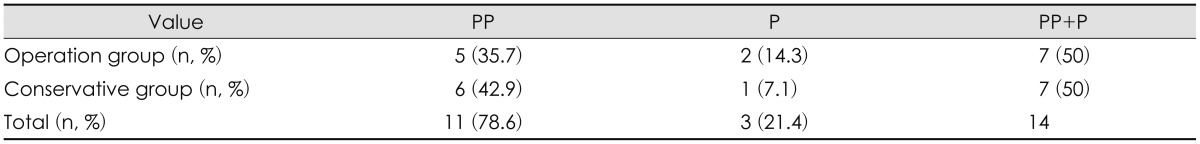
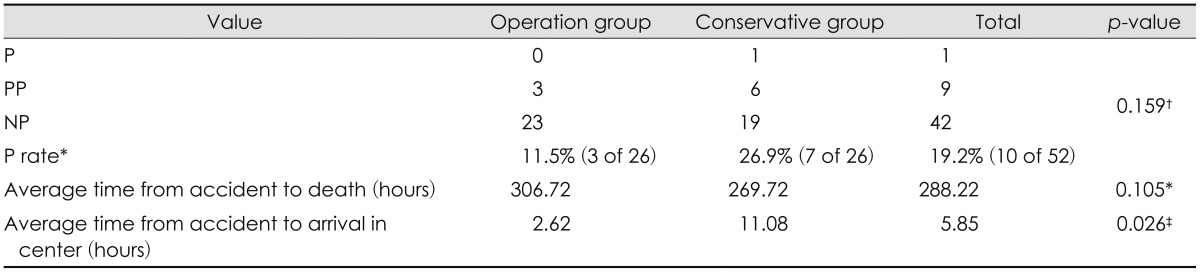
Overall preventable death rate was 19.2% (10 patients of enrolled 52). Most of these patients were cases of potentially preventable death (9 patients, 17.3%). The preventability of operation group was 11.5% and that of conservative group was 26.9%. The average time from the accident to arrival of hospital was 5 hours and 51 minutes. For the overall 52 patients, the average time from the accident to death was 288 hours. In patients who had surgery, it was 306 hours and that of conservative group was 269 hours (Table 2). Only the average time from the accident to arrival of hospital between the two groups showed significant differences. The following studies would be needed because the above analysis did not consider the characteristics and other variables between the two groups. Patients who determined preventable death and potentially preventable death with signing the DNR order were 14. They were classified to non-preventable death (Table 3).
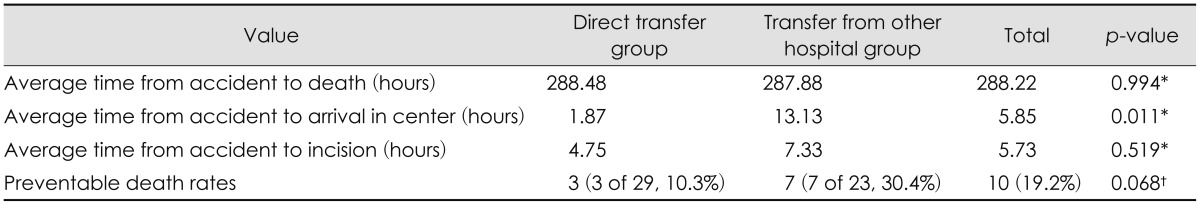
For all 52 patients, the average time taken from the accident to the arrival at the hospital was 5 hours and 51 minutes. In the case of patients who were directly transferred to the hospital, it was 1 hour and 12 minutes. For patients who arrived at the hospital after passing through another hospital, it was 13 hours and 8 minutes. Among the 26 patients who had surgery, the average time from the accident to the beginning of surgery was 5 hours and 44 minutes. Among the patients who had operations, when the patients were directly transferred to the our hospital, the average time from the accident to the beginning of the operation was 4 hours and 52 minutes. In the case of patients passing through other hospitals, it was 7 hours and 20 minutes. The directly transferred patients had less time elapse before surgery (Table 4). Like the results of the operation whether, only the average time from the accident to arrival of hospital between the two groups showed significant differences.
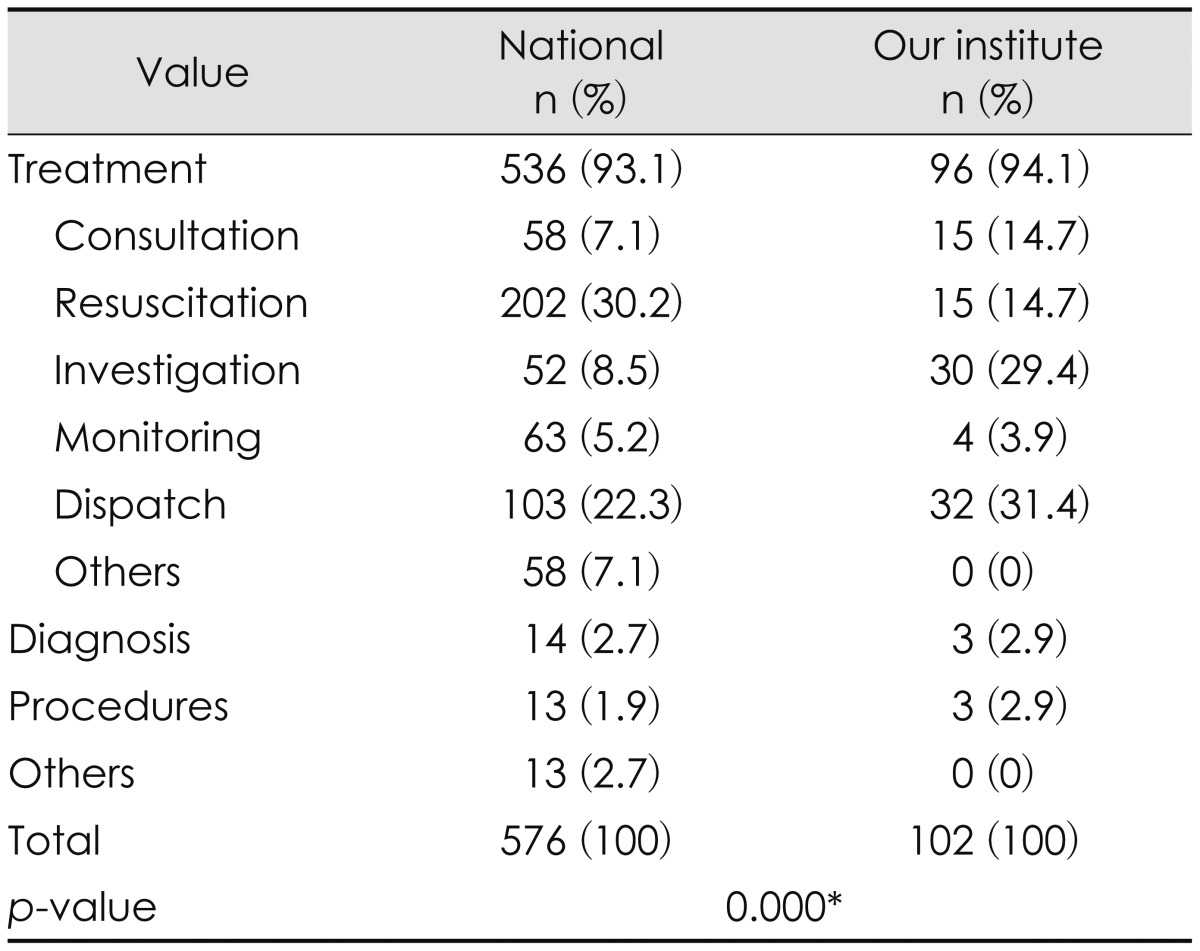
Among 52 patients, 130 problems were detected by panel discussions. It was classified structural problems (28 cases of total 130) that were not currently solved. Except structural problems, problems of process were compared with the research of 2012, Korean preventable and potentially preventable traumatic death rates. Unlike the research, problems of process was mostly investigation and dispatch problems (Table 5).
The preventable and potentially preventable traumatic death rates is a concept that has been used in the United States and the United Kingdom to evaluate treatments for injured patients since the 1960s.35814) South Korea performed the evaluation three times in total from 1997 to 2009, and the whole preventable death rate has been gradually decreasing and is currently comparable to that of advanced countries.
In this study, overall preventable death rate of the patients who were admitted to neurosurgery department was 19.2%. The rate of preventable and potentially preventable traumatic death was lower than that of the research of 2012, Korean preventable and potentially preventable traumatic death rates of 35.2%.7) However, the preventable death rates of TBI patients were not identified in the research of 2012, Korean preventable and potentially preventable traumatic death rates. Therefore, it cannot be directly compared with the results of this study and that of previous study. We might estimated that the preventable death rates of this study is lower than that of TBI patient of previous study as follows. In our department from 2013, it was established a trauma team and system for severe TBI. Though this process could not be compared quantitatively to previous studies, the rate of preventable and potentially preventable traumatic death might be reduced because of decrease of time to transference, blood transfusions, initial treatment and consultation in emergency room, etc.
The number of patients who performed surgery is equal to that of conservative therapy group. However, the operation group's preventability was 11.5% and that of the patients with conservative therapy was 26.9%. It shows that the rate of the group without surgery was higher. Although other variants were not controlled and further study is needed, this result might suggest that expanded treatment and operations can further decrease the death rate.
Patients who determined preventable death or potentially preventable death with signing the DNR order were 14. This result suggests that expanded treatment and operations can further decrease the death rate. We propose that active recommendations for surgery in accordance with the patient's state might prevent death, during the interview with family of patients.
The quick process to operation is necessary to a severe TBI patient who needs operation. In this study, the directly transferred patients took a shorter time to arrive at the hospital, and the time to surgery was also shorter. Therefore, we suggest that fast transfer to the hospital is needed. It is possible to decrease wasted time by connecting certain regions into one area for transference12) and appropriate transference of patients to hospitals. We can expect better results if guidelines and education are given for regional emergency medical technicians, patient transportation, treatment, and triage in the pre-hospital stage.611) Coordination among operation room personnels is necessary to minimize time to incision after the accident and transfer to the emergency center.
In the analysis of problems of the hospital stage in our study, diagnosis and dispatch to other place within hospital were more than half. Specifically, lack of immediately available diagnostic equipment was the most. If diagnostic equipment and paramedics are supplemented, the problems might be reduced.
This study has limitations. First, autopsy findings were not included in the data. It is possible to evaluate the death of reason by final autopsy findings, however this study employed clinical findings instead. According to Stothert et al.,13) when clinical data and autopsy data are compared, there is 30% dissonance. This difference affects 5% of preventable death judgments. For more precise results, research including autopsy findings is essential. Second, this study excluded patients who had cardiac arrest when transferred to the hospital, as well as during treatment, because their death causes were not clear. In this regard, there may be selection bias. Third, this study examined a small number of patients and single center study. Fourth, to judge the probability of death, it was carried out by panel consensus discussion. It is thought that this matter be improved by trying quantitative analysis such as TRISS, International Classification of Diseases (ICD)-based injury severity score.
In this study, authors report the preventable and potentially preventable traumatic death rates about severe TBI during for 2 years. Although various limitations are described as above, this study is significant because there are not many studies about preventable death rate on severe TBI. We identify that the rate of preventable and potentially preventable traumatic death of severe TBI is lower in comparison with all patients. Also, quick processing in transfer and operation might be supposed to lower the preventable death rate. For decrease of preventable death rate, a follow up research in neurosurgery department is needed.
References
1. Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987; 27:370–378. PMID: 3106646.
2. Cales RH, Trunkey DD. Preventable trauma deaths. A review of trauma care systems development. JAMA. 1985; 254:1059–1063. PMID: 3894708.

3. Cayten CG, Stahl WM, Agarwal N, Murphy JG. Analyses of preventable deaths by mechanism of injury among 13,500 trauma admissions. Ann Surg. 1991; 214:510–520. PMID: 1953102.

4. Draaisma JM, de Haan AF, Goris RJ. Preventable trauma deaths in The Netherlands--a prospective multicenter study. J Trauma. 1989; 29:1552–1557. PMID: 2685338.
5. Gorman DF, Teanby DN, Sinha MP, Wotherspoon J, Boot DA, Molokhia A. Preventable deaths among major trauma patients in Mersey Region, North Wales and the Isle of Man. Injury. 1996; 27:189–192. PMID: 8736294.

6. Hussain LM, Redmond AD. Are pre-hospital deaths from accidental injury preventable? BMJ. 1994; 308:1077–1080. PMID: 8173428.

7. Kim H, Jung KY, Kim SP, Kim SH, Noh H, Jang HY, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med. 2012; 23:189–197.
8. Kreis DJ Jr, Plasencia G, Augenstein D, Davis JH, Echenique M, Vopal J, et al. Preventable trauma deaths: Dade County, Florida. J Trauma. 1986; 26:649–654. PMID: 3723641.
9. MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma. 1999; 47:S34–S41. PMID: 10496608.

10. MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006; 354:366–378. PMID: 16436768.

11. Papadopoulos IN, Bukis D, Karalas E, Katsaragakis S, Stergiopoulos S, Peros G, et al. Preventable prehospital trauma deaths in a Hellenic urban health region: an audit of prehospital trauma care. J Trauma. 1996; 41:864–869. PMID: 8913218.
12. Polk HC Jr. Quality, safety, and transparency. Ann Surg. 2005; 242:293–301. PMID: 16135916.
13. Stothert JC Jr, Gbaanador GB, Herndon DN. The role of autopsy in death resulting from trauma. J Trauma. 1990; 30:1021–1025. PMID: 2388303.

14. Yates DW, Woodford M, Hollis S. Preliminary analysis of the care of injured patients in 33 British hospitals: first report of the United Kingdom major trauma outcome study. BMJ. 1992; 305:737–740. PMID: 1422327.

TABLE 3
Patients who determined preventable death or potentially preventable death with signing the do not resuscitate




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download