Abstract
Here we report a case of penetrating neck injury to the posterior fossa that was shown, using high-resolution computed tomography (HRCT) and digital subtraction angiography (DSA), to involve no vascular injury. A 54-year-old man was brought to the emergency department after a penetrating injury to the left side of the posterior neck and occipital area with a knife. He was in an intoxicated state and could not communicate readily. On initial examination, his vital signs were stable and there was no active bleeding from the penetrating site. Because of concern about possible injury to adjacent vessels, we performed HRCT and DSA sequentially, and identified that the blade of the knife had just missed the arteriovenous structures in the neck and posterior fossa. The patient was then transferred to the operating room where the knife was gently removed. Further careful exploration was performed through the penetrating wound, and we confirmed that there were no major injuries to the vessels and neural structures. Postoperative computed tomography revealed that there was minimal hemorrhage in the left cerebellar hemisphere. The patient made a full recovery without any neurologic deficit. In this case, HRCT is a suitable tool for the initial overall evaluation. For the evaluation of vascular injury, DSA can be a specific and accurate tool. Mandatory exploration widely used for penetrating injuries. After careful preoperative evaluation and interpretation, simple withdrawal of material can be a choice of treatment.
Penetrating neck injury (PNI) is challenging due to in evaluation and management. Vital organ structures, including the major blood vessels, spinal cord, trachea, and esophagus, pass through the neck region, and are tightly packed in a relatively small area. Mahmoodie et al.10) reported that vascular exploration was the most common reason for surgery (in 67.2% of their patients) and the most common surgical intervention was vein ligation. Complications were reported in 9.3% of their patients and the mortality rate was 1.5%.
Penetrating brain injury (PBI) is less prevalent than blunt injury, but has a worse prognosis and a higher mortality rate.9) Foreign bodies can cause immediate complications such as intracranial hemorrhage, pneumocephalus, contusion, and brain or brain stem injury, and can lead to infarction due to damaged vascular territories, abscess, meningitis, and encephalitis. Several imaging techniques have been recommended and a flow chart has been developed for precise evaluation of PBI. However, there is no definite guideline in these patients.1814)
Here we describe a patient who presented with an injury penetrating through the neck to the posterior fossa as the result of an accidental stabbing, focusing on imaging studies for rational and precise decision-making.
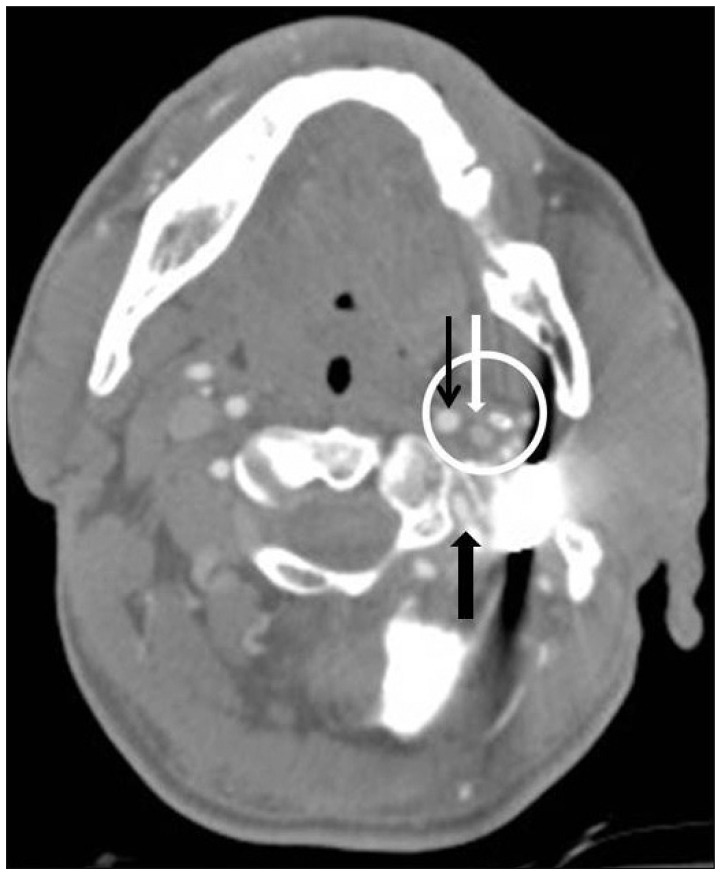
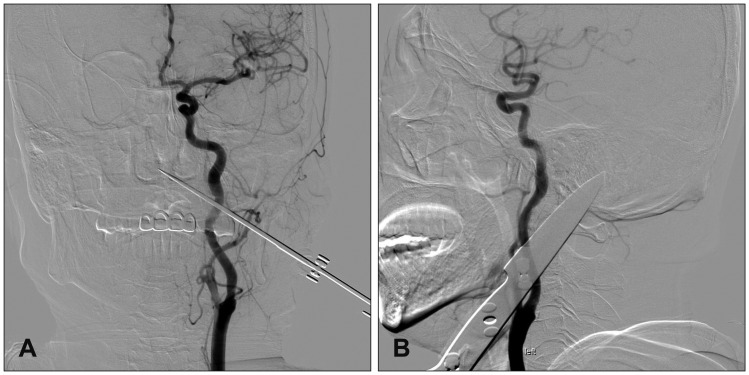
A 54-year-old man was brought to the emergency room with a stab wound on the left side of the upper posterior neck (Figure 1). He was intoxicated, with an initial blood ethanol level of 255 mg/mL. He was not able to communicate and was not cooperative on neurologic examination. The initial blood pressure was 143/90 mmHg, pulse rate was 109 beats/minute, and respiratory rate was 15 times/minute. Hemoglobin was 13.8 g/mL and the platelet count was 324,000/µL. Other laboratory findings were within normal range. There was no massive hemorrhage in the head or neck on three-dimensional high-resolution computed tomography (HRCT) and the cervical spine, trachea, and esophagus were intact. The knife had pierced the paraspinal muscles and the base of the occipital bone behind the stylomastoid foramen (Figure 2). The tip of the knife lay on the roof of the fourth ventricle. The patency of the left cervical carotid artery was suspected to be intact because there was no perivascular hematoma or leakage of blood around the vessel (Figure 3). No signs of tearing were seen in the basilar artery or its major vessels, including the posterior inferior cerebellar artery. However, because of the metal artifact, we could not guarantee that there were no combined vascular injuries. Computed tomography (CT) revealed no intraventricular hemorrhage in the fourth ventricle. We then performed digital subtraction angiography (DSA) to further investigate possible damage to the vascular structures. On injection of the left carotid artery, the blood flow was intact and showed no signs of arterial damage (Figure 4). On injection of the left vertebral artery, the arterial and venous phases indicated normal patency (Figure 5).
Based on these imaging findings, we proceeded to surgery to remove the knife and explore the penetrating wound using a microscope with simultaneous preparation for open craniotomy. The knife was gently removed without much difficulty under general anesthesia. There was minimal bleeding from the stabbing canal and there appeared to be no active bleeding from the major vessels. After about 20 minutes of observation, the wound was carefully irrigated and subsequently closed.
On the postoperative CT scan, a small hemorrhage was noted on the left cerebellar tonsil, but this was seen to resolve gradually on follow-up CT. The patient made a full recovery without any neurologic deficit, and was discharged on postoperative day 18.
It is widely known that when assessing a PNI, the neck region can be divided into three areas according to the point of entry of the foreign body. Zone I is the horizontal area between the clavicle and cricoid cartilage. The common carotid arteries, proximal vertebral arteries, subclavian arteries, trachea, and esophagus are located in this area. Zone II is the area between the cricoid cartilage and the angle of the mandible. Zone III is the area between the angle of the mandible and the base of the skull, through which pass the distal external carotid arteries, vertebral arteries and jugular veins. Therefore, the present case can be considered a Zone III PNI. A foreign body in the neck can damage vital structures, including the major blood vessels, trachea, and esophagus, resulting in increased risk of mortality and morbidity. Singh et al.13) reported that the current mortality rate for PNI is 3% to 6% and one of the most common complications of PNI are vascular trauma, occurring in 25% of cases, with mortality rates approaching 50%. Evaluation for injury to major structures is the first important task to perform in the emergency room.
Gracias et al.6) have recommended CT scanning as an accurate and rapid method for evaluating the trajectory of penetration and Saito et al.12) have reported that CT angiography has high sensitivity and a negative predictive value for vascular injury. However, the artifact generated by the foreign body on CT scan is a major obstacle when trying to determine if the surrounding structures are free from injury, as it was in this case. Some authors have also reported DSA to be a useful tool for evaluation of PBI and PNI.37) DSA can provide clinicians with much information, including on vessel patency, leakage of blood, delayed capillary refill time, and any other vascular abnormalities. However, DSA has several limitations and complications. First, it is time-consuming to perform and requires the patient to be taken to the angiography suite, so may not be suitable for unstable patients. In addition, as Ferguson et al.5) have pointed out, DSA still misses about 1% of vascular injuries. Nevertheless, the use of three-dimensional rotational angiography can provide detailed structural information enabling precise pre-surgical planning. In our case, the blade was crossing over the major arterial passage. The vessel injuries were not fully appreciated on conventional two-dimensional images because the vessels and the foreign body were seen as overlapped. DSA with rotational images was necessary to gain additional views from various projection angles.
Because of high-resolution image study modality, the selective operation and conservative management is one of options in treatment of PNI. Also, adequate exploration can reduce tissue damages and decrease morbidity rate. Cosan et al.4) reported that simple withdrawal of material can be one of the treatment methods in penetrating injuries. For using this simple withdrawal method, neurovascular evaluation should be fully done and interpretation should be careful. The shape of penetrating material and vector are also considerable factors in penetrating injuries. In the stab wound cases, the tract is cone shape. The diameter of handle is much larger than tip of the knife. Removal material opposite to stabbing vector is much safer than removal from the tip.
Cerebrospinal fluid (CSF) leakage is one of the most common complications after traumatic brain injury. Bell et al.2) reported that 4.6% cases of traumatic brain injury developed post-traumatic CSF leakage. In this case, there was no definite clue for suggesting CSF leakage on post-operative CT scan and clinical presentation. Because it is one of the most common complications and it can increase the mortality, close observation and image study should be done for follow up period. The most common treatment of CSF leakage is an exploration and closure of leakage point tightly. Interestingly, Meirowsky et al.11) reported there was a spontaneous closure of CSF leakage in 44% patients who had fistulas complicating missile wounds of the brain. The characteristics of the entry and exit zone, transventricular trajectories, existence of air sinus penetration are risk factors of CSF leakage. In this case, there is no evidence of CSF leakage in operation fields. The distance between entry zone and penetrated dura is longer than a skull vault penetrating injury. Also, large amount of neck muscle and fascia can seal of CSF leakage. In that reasons, we do not explore penetrated dura site, just tightly close neck muscle and fascia. There is no CSF leakage sign and symptom postoperatively. But, limited debridement can be a limitation of this procedure method. Removal of infected tissue is another aim of exploration. Surgeon can explore just via a small canal and irrigation through it. There is no evidence of infection in this case. But, the risk of simple withdrawal of material and comparison to mandatory exploration should be evaluated near future.
As in this case, when a vessel injury is suspected, the initial HRCT evaluation should be coupled with DSA to avoid inappropriate management of PNI and PBI.
PNI and PBI are complex and come with high morbidity and mortality rates. The most common cause of these complications is vascular injury. The initial evaluation of a combined injury in Zone III and the posterior fossa should include not only the soft and musculoskeletal tissue but also assessment for vascular injury. HRCT is a suitable tool for the initial overall evaluation and DSA is a specific and accurate tool for detection of vascular injury. After careful evaluation and interpretation, simple withdrawal of stabbed material can be a choice of treatment.
References
1. Arabi B, Alden TD, Chesnut RM, Downs JH 3rd, Ecklund JM, Eisenberg HM, et al. Neuroimaging in the management of penetrating brain injury. J Trauma. 2001; 51:S7–S11. PMID: 11505193.
2. Bell RB, Dierks EJ, Homer L, Potter BE. Management of cerebrospinal fluid leak associated with craniomaxillofacial trauma. J Oral Maxillofac Surg. 2004; 62:676–684. PMID: 15170277.

3. Berne JD, Reuland KR, Villarreal DH, McGovern TM, Rowe SA, Norwood SH. Internal carotid artery stenting for blunt carotid artery injuries with an associated pseudoaneurysm. J Trauma. 2008; 64:398–405. PMID: 18301205.

4. Cosan TE, Arslantas A, Guner AI, Vural M, Kaya T, Tel E. Injury caused by deeply penetrating knife blade lodged in infratemporal fossa. Eur J Emerg Med. 2001; 8:51–54. PMID: 11314822.

5. Ferguson E, Dennis JW, Vu JH, Frykberg ER. Redefining the role of arterial imaging in the management of penetrating zone 3 neck injuries. Vascular. 2005; 13:158–163. PMID: 15996373.

6. Gracias VH, Reilly PM, Philpott J, Klein WP, Lee SY, Singer M, et al. Computed tomography in the evaluation of penetrating neck trauma: a preliminary study. Arch Surg. 2001; 136:1231–1235. PMID: 11695963.
7. Herrera DA, Vargas SA, Dublin AB. Endovascular treatment of penetrating traumatic injuries of the extracranial carotid artery. J Vasc Interv Radiol. 2011; 22:28–33. PMID: 21109458.

8. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011; 4:395–402. PMID: 21887033.

9. Liu WH, Chiang YH, Hsieh CT, Sun JM, Hsia CC. Transorbital penetrating brain injury by branchlet: a rare case. J Emerg Med. 2011; 41:482–485. PMID: 18950975.

10. Mahmoodie M, Sanei B, Moazeni-Bistgani M, Namgar M. Penetrating neck trauma: review of 192 cases. Arch Trauma Res. 2012; 1:14–18. PMID: 24719835.

11. Meirowsky AM, Caveness WF, Dillon JD, Rish BL, Mohr JP, Kistler JP, et al. Cerebrospinal fluid fistulas complicating missile wounds of the brain. J Neurosurg. 1981; 54:44–48. PMID: 7463119.

12. Saito N, Hito R, Burke PA, Sakai O. Imaging of penetrating injuries of the head and neck: current practice at a level I trauma center in the United States. Keio J Med. 2014; 63:23–33. PMID: 24965876.
13. Singh RK, Bhandary S, Karki P. Managing a wooden foreign body in the neck. J Emerg Trauma Shock. 2009; 2:191–195. PMID: 20009310.

14. Temple N, Donald C, Skora A, Reed W. Neuroimaging in adult penetrating brain injury: a guide for radiographers. J Med Radiat Sci. 2015; 62:122–131. PMID: 26229677.

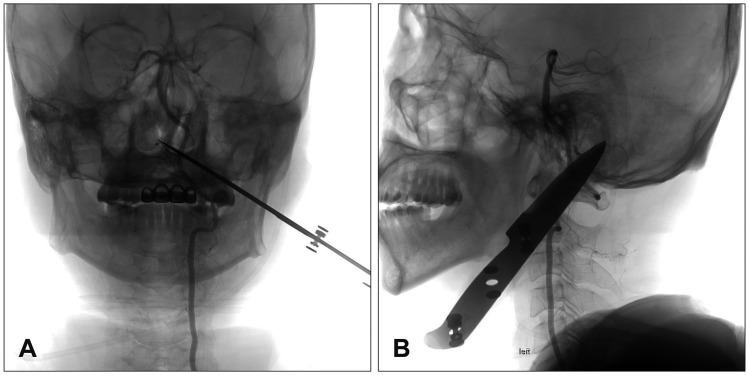
FIGURE 1
Photograph taken in the emergency room. (A) The knife is shown to be penetrating from behind the left mandible (B) toward the occiput.
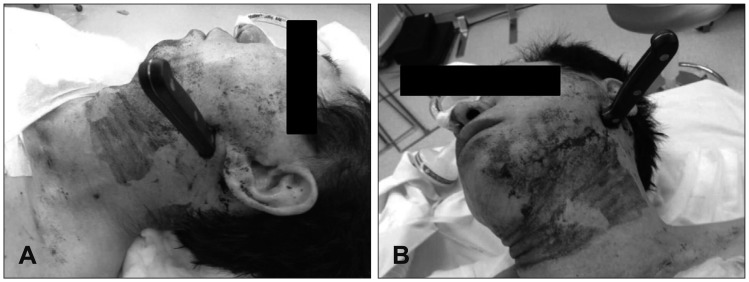
FIGURE 2
(A) Three-dimensional reconstructed computed tomography showing that the knife pierced the paraspinal muscles on the left side and (B) the base of the occipital bone behind the stylomastoid foramen.
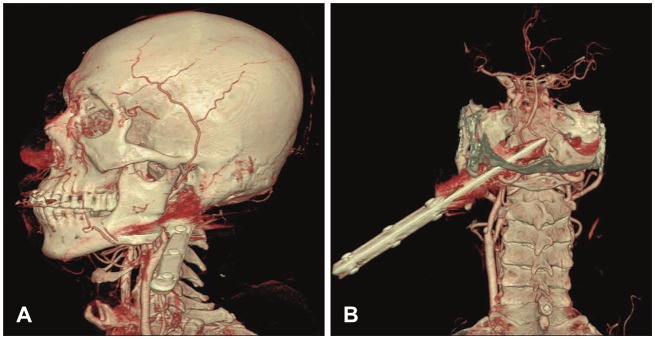
FIGURE 3
High-resolution computed tomography showing the major vessels (white circle) were a little apart from the blade of the penetrating knife. Internal carotid artery (narrow black arrow), internal jugular vein (white arrow), and vertebral artery (black arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download