Abstract
All iatrogenic vascular injury occurring during discectomy is a rare complication, but fatal if not immediately diagnosed. When a vascular injury is highly suspected during discectomy, immediate vascular evaluation is needed even vital signs are stable during and immediately after the operation. We describe a case of iatrogenic abdominal aortic injury that occurred during discectomy in a spondylodiscitis patient, which was treated by endovascular repair.
Spinal infections, including spondylodiscitis, are often treated conservatively, but if this treatment is not effective, surgery is considered.451314) In these cases, discectomy and debridement of the infected material are developed. If deformity is also present along was with spondylodiscitis, spinal fusion is also recommended.
Vascular injuries occurring during discectomy are rare, but they may cause severe and fatal complications. The great vessels, which are located in front of the vertebral body, are at risk of injury during discectomy. In most vascular injuries, symptoms occur immediately, but the onset of symptoms may be delayed due to pseudoaneurysm, arteriovenous fistula, and the tamponade effect of a hematoma on a susceptible area of an injured vessel during the operation. Immediate signs of vascular injury are decreased blood pressure, increased heart rate, decreased oxygen saturation, and decreased end-tidal CO2.7)
Early diagnosis and endovascular intervention are very important and lead to a relatively favorable outcome.6) If major vessel injury is suspected during discectomy, the surgical procedure should be stopped and rapid abdominal, retroperitoneal evaluation is needed.
We report a case of iatrogenic abdominal aortic injury that occurred during discectomy in a spondylodiscitis patient, which was treated by endovascular repair.
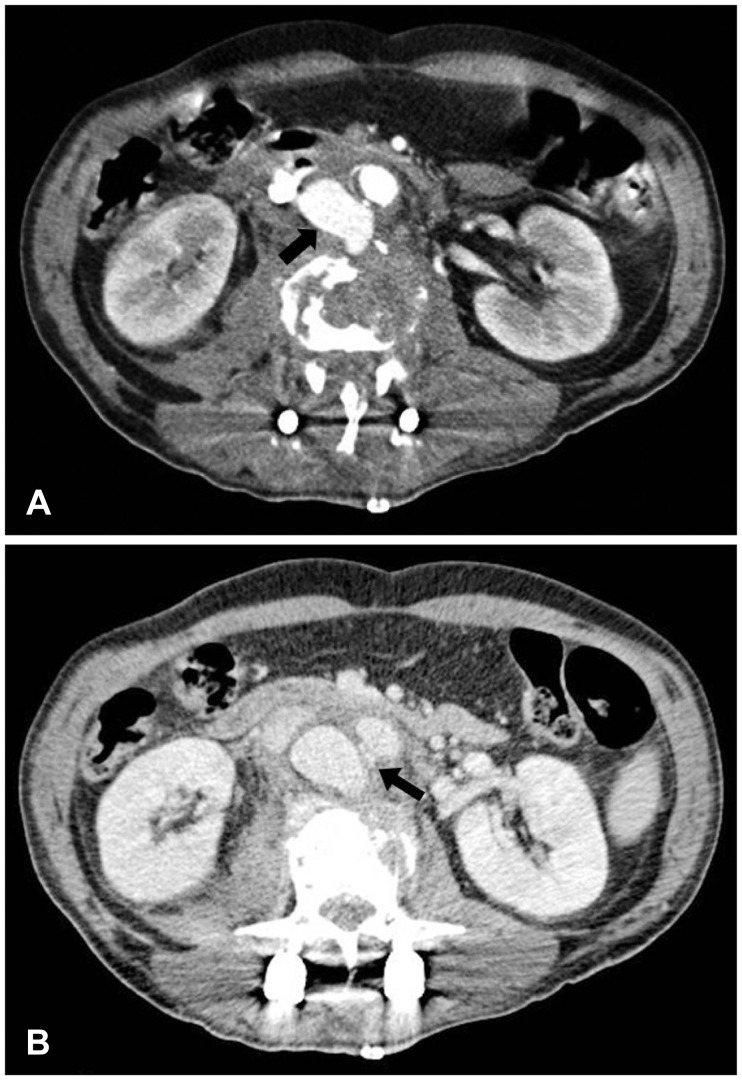
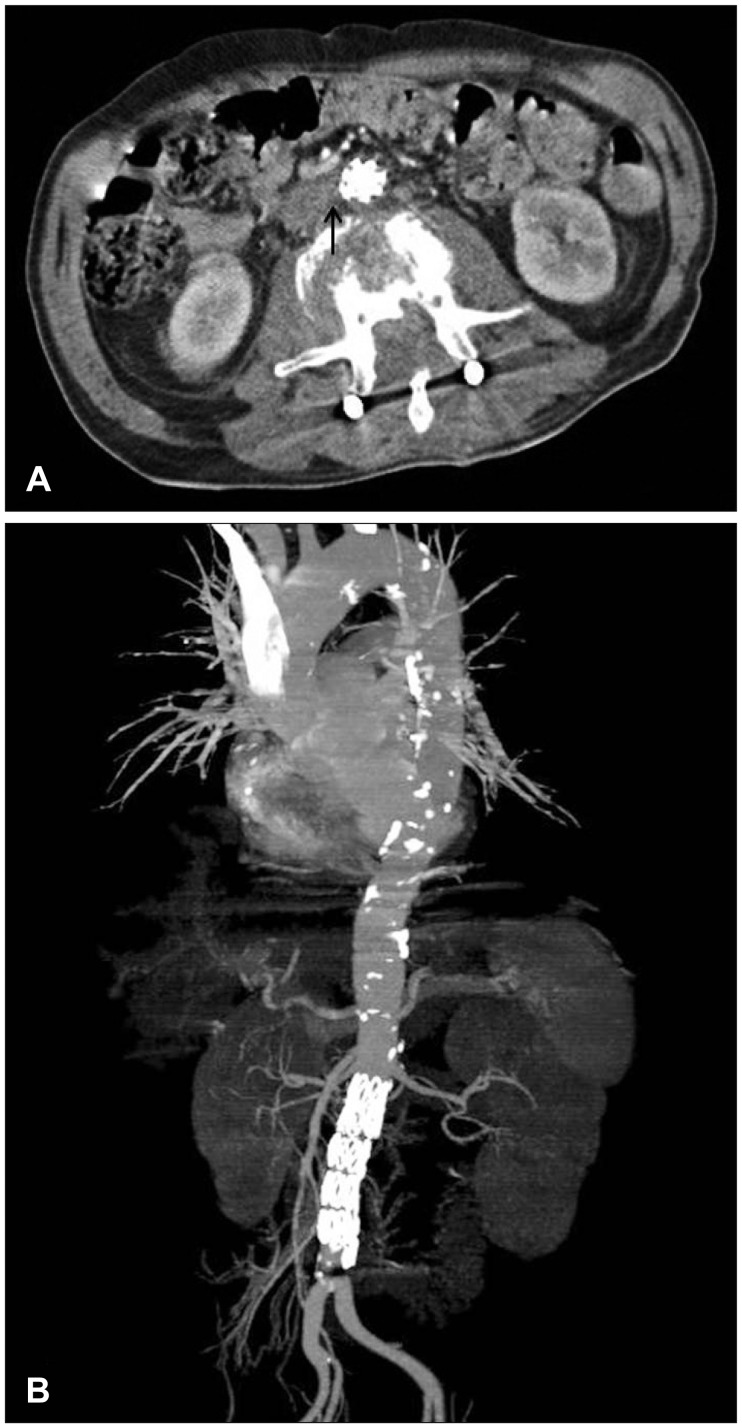
A 70-year-old male was admitted to our emergency room with severe back pain. He complained of severe back pain 7 days ago, during treatment for pneumonia at another hospital. His general condition was poor and he underwent tracheostomy, however, he was able to walk without assistance. Lumbar magnetic resonance imaging showed signal change in the L2–3 vertebral bodies and presence of epidural abscess (Figure 1). We treated him conservatively. However, 3 weeks later, he still complained of back pain and his erythrocyte sedimentation rate and C-reactive protein values did not decrease. We decided to perform an operation. During discectomy and curettage, sudden bleeding occurred in the disc space. We packed the area with Gelfoam and Cottonoid, and the bleeding was controlled. We thought that the bleeding may have occurred from the bone. We mistook vascular injury for the bleeding from the bone because the bleeding was easily controlled using only Gelfoam and Cottonoid. On the next day of the operation, the patient complained of abdominal pain and his blood pressure dropped. We performed abdominal computed tomography imaging and found that a hematoma had displaced a vessel and caused a pseudoaneurysm at the aortocaval space (Figure 2). An emergency stent insertion was conducted at the thoracic surgery department (Figure 3). His vital signs was stabilized after the procedure. The patient was discharged 4 weeks later with no neurological deficit or back pain.
Spondylodiscitis most commonly occurs at L4-5, perhaps due to their relatively large vertebral body and disc space.4) Spondylodiscitis is treated conservatively, but surgical management is needed when there is uncontrolled infection, severe pain, and vertebral destruction-induced spinal instability. If epidural abscesses are present in spondylodiscitis, early surgical management is recommended.11) Discectomy and debridement of the infected material are necessary. Infected disc material is more friable than a degenerative disc.
Vascular injuries after discectomy most frequently occur at the L4-5 level, and by the use of pituitary rongeurs.3) Left common iliac arteries, which are located immediately anterior to the disc space, are the most commonly injured vessels.1) Paramedian or posterolateral approaches for far lateral discs are less likely to injure great vessels compared to standard discectomy for central or paramedian herniated lumbar discs.8) Risk factors for vascular injury during discectomy are adhesion between the vertebral body and retroperitoneal vessels, and disruption of annulus fibrosus and anterior longitudinal ligaments.10) In spondylodiscitis patients, penetrating injuries through vertebral body destruction may be possible.
Late recognition, diagnosis, and treatment increase mortality rate,3) but delayed diagnosis can occur. Susceptible positions during discectomy may tamponade the injured vessel site and can cause delayed hemorrhage. Psedoaneurysms may develop due to localized arterial wall disruption. Abdominal pain, leg edema, high output cardiac failure, and hydronephrosis may occur as the pseudoaneurysm gradually worsens. These symptoms can occur months to years after surgery.10)
Early diagnosis and endovascular intervention are very important, and lead to a relatively favorable outcome. Immediate signs of vascular injury during surgery are decreased blood pressure, increased heart rate, decreased oxygen saturation, and decreased end-tidal CO2.7) If vascular injury is not recognized immediately, rapid blood loss into the retroperitoneal and intraperitoneal space can result in a fatal outcome. When there is high suspicion of vascular injury during discectomy, immediate vascular evaluation is need even if vital signs during and immediately after the operation are stable.912)
Direct repair of injured vessels is associated with high mortality and morbidity rate, hence, endovascular stent grafts are initially used. As endovascular procedures advanced, endovascular stent grafts and coil embolization became more useful and effective,15) especially to treat lesions that are detected late, such as pseudoaneurysm and arteriovenous fistula.8) The patency of an endovascular stent graft is well-preserved.2)
In cases where there is significantly more bleeding than normal cases of general discectomy, vascular evaluation may need to be considered, even if vital signs are stable during and immediately after the operation. If there is abdominal discomfort and decreasing blood pressure after discectomy, the possibility of vascular injury should be considered. More caution is needed when normal anatomical structures are altered, like in the case of spondylodiscitis.
References
1. Bingol H, Cingoz F, Yilmaz AT, Yasar M, Tatar H. Vascular complications related to lumbar disc surgery. J Neurosurg. 2004; 100:249–253. PMID: 15029913.

2. Canaud L, Hireche K, Joyeux F, D'Annoville T, Berthet JP, Marty-Ané C, et al. Endovascular repair of aorto-iliac artery injuries after lumbar-spine surgery. Eur J Vasc Endovasc Surg. 2011; 42:167–171. PMID: 21592826.

3. Desaussure RL. Vascular injury coincident to disc surgery. J Neurosurg. 1959; 16:222–228. PMID: 13642113.

4. Devkota P, Krishnakumar R, Renjith Kumar J. Surgical management of pyogenic discitis of lumbar region. Asian Spine J. 2014; 8:177–182. PMID: 24761200.

5. Di Martino A, Papapietro N, Lanotte A, Russo F, Vadalà G, Denaro V. Spondylodiscitis: standards of current treatment. Curr Med Res Opin. 2012; 28:689–699. PMID: 22435926.

6. Erkut B, Unlu Y, Kaygin MA, Colak A, Erdem AF. Iatrogenic vascular injury during to lumbar disc surgery. Acta Neurochir (Wien). 2007; 149:511–515. discussion 516. PMID: 17387429.

7. Hönemann CW, Brodner G, Van Aken H, Ruta U, Durieux ME, Möllhoff T. Aortic perforation during lumbar laminectomy. Anesth Analg. 1998; 86:493–495. PMID: 9495399.
8. Inamasu J, Guiot BH. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien). 2006; 148:375–387. PMID: 16322906.

9. Lee CK, Kim Sc, Kim SH. Common iliac vessel injury after lumbar discectomy. Korean J Spine. 2011; 8:229–231.

10. Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002; 24:189–195. PMID: 12217278.

11. Patel AR, Alton TB, Bransford RJ, Lee MJ, Bellabarba CB, Chapman JR. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014; 14:326–330. PMID: 24231778.

12. Prabhakar H, Bithal PK, Dash M, Chaturvedi A. Rupture of aorta and inferior vena cava during lumbar disc surgery. Acta Neurochir (Wien). 2005; 147:327–329. PMID: 15625589.

13. Santhanam R, Lakshmi K. A retrospective analysis of the management of postoperative discitis: a single institutional experience. Asian Spine J. 2015; 9:559–564. PMID: 26240715.

14. Silber JS, Anderson DG, Vaccaro AR, Anderson PA, McCormick P. Management of postprocedural discitis. Spine J. 2002; 2:279–287. PMID: 14589480.

15. Skippage P, Raja J, McFarland R, Belli AM. Endovascular repair of iliac artery injury complicating lumbar disc surgery. Eur Spine J. 2008; 17(Suppl 2):S228–S231. PMID: 17712578.

FIGURE 1
Sagittal T2-weighted magnetic resonance imaging shows diffuse bone marrow signal change, endplate destruction and epidural abscess formation at the L2–3 level.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download