Abstract
Multiple primary or secondary malignancies after anticancer therapy were recently reported to be increasing in frequency. The authors describe a case of metachronous metastatic pulmonary basaloid carcinoma to the central nervous system that was discovered after chemotherapy and radiation therapy for cervical uterine carcinoma. Two different types of cancer developed within some interval. There's the possibility that a secondary pulmonary neoplasm developed after the chemotherapy and radiotherapy conducted as cervical cancer treatment.
Multiple primary or secondary malignancies after anticancer therapy were recently reported to be increasing in frequency because of advancement of chemotherapy technology and resultant longer patient survival times. Metachronous cancers are multiple primary tumors developing at intervals. The incidence of multiple primary malignancies is approximately 0.73% to 11.7% of cancer patients6) and incidence of the metachronous second primary cancers was 3.8%.14)
Intramedullary spinal cord metastasis (ISCM) is found in only 1.65% of autopsy studies of patients with lung cancer.11) ISCM raises many ethical concerns and challenges in treatment because determination of the most appropriate treatment must be made based on medical conditions and expected survival of the patient.
The author experienced a case of metastasis of metachronous basaloid carcinoma of the lung to the brain parenchyma and spinal cord that developed after chemotherapy and radiation therapy for uterine cervical carcinoma.
A 40-year-old female visited the Gynecology Department for evaluation of leg edema. Abdominal computed tomography (CT) showed bilateral hydronephrosis and lymphadenopathy in the pelvic and para-aortic areas. A punch biopsy of the erosive lesion of the uterine cervix revealed a combination of well-differentiated adenocarcinoma and small-cell carcinoma. The histologic findings of the uterine cervix showed adenocarcinoma with an irregular glandular architecture and infiltration of small hyperchromatic tumor cells.
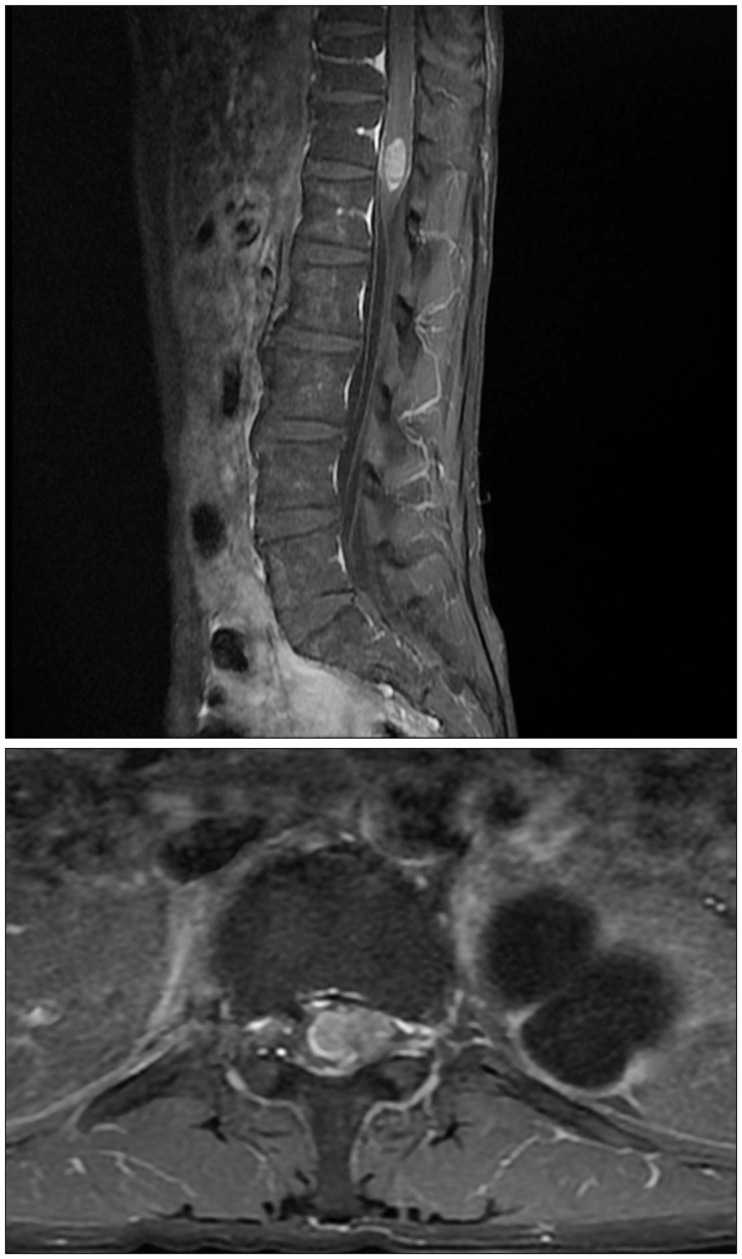
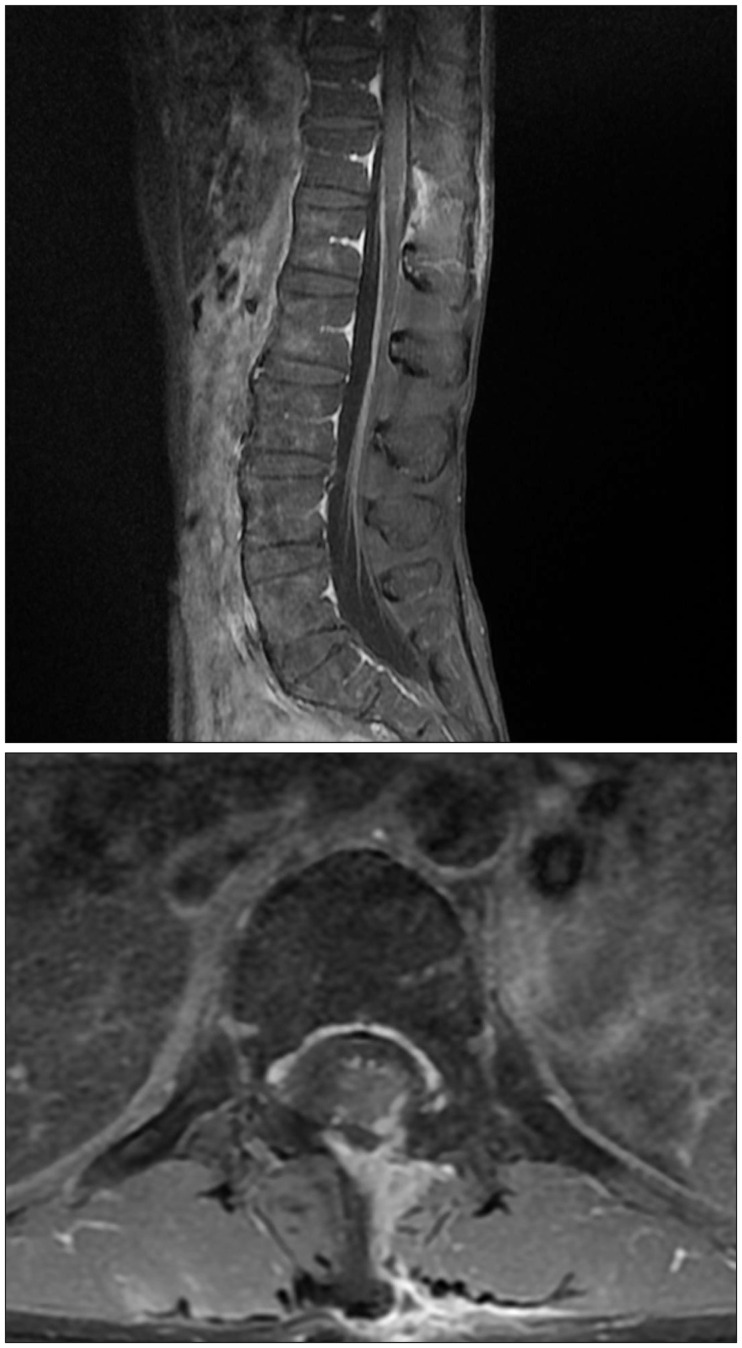
Positron emission tomography (PET) showed the cervix and pelvic and para-aortic lymph nodes lesions. Under a diagnosis of stage IIIB cervical cancer, weekly cisplatin (40 mg/m2) was given in the pelvic and para-aortic areas. In addition to external radiation, intracavitary radiation was administered as concurrent therapy. Follow-up PET carried out 5 months later showed extensive lymph node metastasis along the left paravertebral lymph nodes on the pelvic side. Taxol and carboplatin combination chemotherapy were given for six cycles. After 1 year, PET and chest CT revealed multiple metastatic nodules in both lungs and subpleural nodules with vascular connections. A wedge resection of lung was performed. Gross findings of the specimen showed a 2.8×2.7-cm, well-circumscribed, whitish, firm, lobulated mass with hemorrhage and necrosis. The histologic findings of the lung specimen revealed pulmonary basaloid carcinoma which lobulated solid tumor cell sheets with peripheral palisading and comedo type necrosis (Figure 1). Five years later, she visited the clinic again complaining of headache and left hemiparesis. Brain magnetic resonance imaging (MRI) showed a huge heterogeneous mass in the right parieto-occipital area (Figure 2). After the craniotomy and surgical resection of the lesion, patient recovered consciousness and hemiparesis, and the pathologic findings revealed pulmonary basaloid carcinoma. Whole-brain radiation therapy comprising a total dose of 5,500 cGy in 250 cGy daily fractions was administered postoperatively, and six cycles of chemotherapy with genexol and carboplatin was performed. One year after the brain surgery, the patient began to suffer from right leg weakness followed by severe radiating pain on the same side and voiding difficulty. We checked follow up brain CT which did not showed recurrence and lumbar MRI showed an intramedullary tumor at the level of T12-L1 (Figure 3). She underwent gross removal of the spinal tumor through a T12-L2 hemilaminectomy (Figure 4), and the pathologic findings revealed metastatic pulmonary basaloid carcinoma. Her disabling pain was resolved after surgery. Her knee and ankle motor power was improved, enabling her to walk. Booster radiotherapy with a total dose of 4000 cGy in 300 cGy daily fractions was administered in the spine postoperatively. Unfortunately, five months later, she was transferred to the emergency room due to stuporous consciousness, and brain MRI revealed multiple metastatic tumors in the cerebrum, cerebellum, and subependymal area. Reoperation was not feasible, and despite brain radiotherapy, the patient did not recover consciousness and died of brain swelling.
Basaloid carcinoma is a tumor occurring in the basal cells within the epithelium. It also occurs in the skin, anus, tongue, larynx, and lungs.4) Basaloid carcinoma of the lung was first reported by Brambilla et al.5) in 1992. The overall survival rate of patients with cancer has rapidly increased due to the development of intensive multimodal therapies including immunosuppressive and cytotoxic therapies. However, as a result, it has brought about subsequent complications, especially the development of secondary malignant neoplasms, which has increased by 10 to 20 times.5) Some authors reported metachronous tumors induced by radiation therapy.121012) The rate was higher among patients who received adjuvant radiation exceeding 40 Gy, pointing out the possibility of secondary neoplasm development due to chemotherapy.3) In current case, the cell characteristics, including hyperchromatic nuclei, are the same in the lung, brain, and spinal cord based on the immunohistochemistry study, including cytokeratin 7, etc.
It has been stated that the majority of spinal metastasis is connected to brain metastasis, and such seeding could thus easily occur.8) Hematogenous spread is a hypothesis commonly accepted in the majority of studies. One noteworthy hypothesis is that intraspinal metastasis is established as portacaval circulation and pulmonary circulation form bypass when coughing and sneezing through spread via a paravertebral plexus of veins (Batson's vein plexus).9) In particular, the tumors that develop due to hematogenous spread are well defined and circumscribed such that they are discrete between the tumor and the spinal cord, thereby rendering them easy to eliminate.7) In current case, the border between metastatic tumor and cord was relatively discrete in MRI finding and also in surgical field and other intraspinal canal lesion was not observed.
Considering that the mean survival time among patients with brain metastasis is 12 to 15 months, surgical resection in patients with ISCM and neurologic deficit is a delicate issue. Therefore, in determining the additional operation for the ISCM of such patients should be seriously considered for ethical problem. Generally, the survival rate of patients with ISCM who receive only radiation therapy is 4 months, whereas the average survival rate of those who receive both surgery and radiation therapy is 6 months.13) However, this is especially true in the patient described herein, who demonstrated a poor response to chemotherapy and radiation therapy.
The authors reported a metastasis case of metachronous pulmonary basaloid carcinoma that showed after chemotherapy and radiation therapy for cervical uterine carcinoma. So there's the possibility that a secondary pulmonary neoplasm developed due to the chemotherapy and radiotherapy conducted as cervical cancer treatment.
References
1. Alexander MJ, DeSalles AA, Tomiyasu U. Multiple radiation-induced intracranial lesions after treatment for pituitary adenoma. Case report. J Neurosurg. 1998; 88:111–115. PMID: 9420081.
2. Amirjamshidi A, Abbassioun K. Radiation-induced tumors of the central nervous system occurring in childhood and adolescence. Four unusual lesions in three patients and a review of the literature. Childs Nerv Syst. 2000; 16:390–397. PMID: 10958546.
3. Argani P, Laé M, Ballard ET, Amin M, Manivel C, Hutchinson B, et al. Translocation carcinomas of the kidney after chemotherapy in childhood. J Clin Oncol. 2006; 24:1529–1534. PMID: 16575003.

4. Bhagavathi S, Chang CH. Multicentric basaloid carcinoma of lung clinically mimicking metastatic carcinoma: a case report. Int J Surg Pathol. 2009; 17:68–71. PMID: 18480394.

5. Brambilla E, Moro D, Veale D, Brichon PY, Stoebner P, Paramelle B, et al. Basal cell (basaloid) carcinoma of the lung: a new morphologic and phenotypic entity with separate prognostic significance. Hum Pathol. 1992; 23:993–1003. PMID: 1381335.

6. Demandante CG, Troyer DA, Miles TP. Multiple primary malignant neoplasms: case report and a comprehensive review of the literature. Am J Clin Oncol. 2003; 26:79–83. PMID: 12576929.
7. Findlay JM, Bernstein M, Vanderlinden RG, Resch L. Microsurgical resection of solitary intramedullary spinal cord metastases. Neurosurgery. 1987; 21:911–915. PMID: 3437960.

8. Grem JL, Burgess J, Trump DL. Clinical features and natural history of intramedullary spinal cord metastasis. Cancer. 1985; 56:2305–2314. PMID: 4052974.

9. Hargraves RW, Cotelingam JD, Harris RD, Pulliam MW. Unusual metastasis to the cauda equina: case report. Neurosurgery. 1986; 19:828–830. PMID: 3785635.

10. Hope AJ, Mansur DB, Tu PH, Simpson JR. Metachronous secondary atypical meningioma and anaplastic astrocytoma after postoperative craniospinal irradiation for medulloblastoma. Childs Nerv Syst. 2006; 22:1201–1207. PMID: 16570196.

11. Okamoto H, Shinkai T, Matsuno Y, Saijo N. Intradural parenchymal involvement in the spinal subarachnoid space associated with primary lung cancer. Cancer. 1993; 72:2583–2588. PMID: 8402479.

12. Sasayama T, Nishihara M, Tanaka K, Mizukawa K, Ehara K, Kanomata N, et al. Two metachronous tumors induced by radiation therapy: case report and review of the literature. J Neurooncol. 2008; 88:315–320. PMID: 18373066.

13. Schiff D, O'Neill BP. Intramedullary spinal cord metastases: clinical features and treatment outcome. Neurology. 1996; 47:906–912. PMID: 8857717.

14. Tabuchi T, Ito Y, Ioka A, Miyashiro I, Tsukuma H. Incidence of metachronous second primary cancers in Osaka, Japan: update of analyses using population-based cancer registry data. Cancer Sci. 2012; 103:1111–1120. PMID: 22364479.

FIGURE 1
Gross findings of wedge-resected lung show a 2.8×2.7-cm, well-circumscribed, whitish, firm, lobulated mass with hemorrhage and necrosis. (B) Microscopic findings show a well-circumscribed, lobulated, solid tumor with peripheral palisading and edematous lung parenchyma (hematoxylin and eosin [H & E] stain, ×40). (C) The tumor shows small cuboidal-to-fusiform tumor cells with moderately hyperchromatic nuclei and nuclear pleomorphism as well as multifocal necrosis (H & E stain, ×100). (D) Immunohistochemistry (IHC) of cytokeratin 7 reveals diffuse positivity in tumor cells (cytokeratin 7, ×200). (E) Immunohistochemistry of P16 reveals diffuse positivity in tumor cells (P16, ×100). (F) IHC of CD99 reveals dot-like positivity in tumor cell cytoplasm (CD99, ×200).
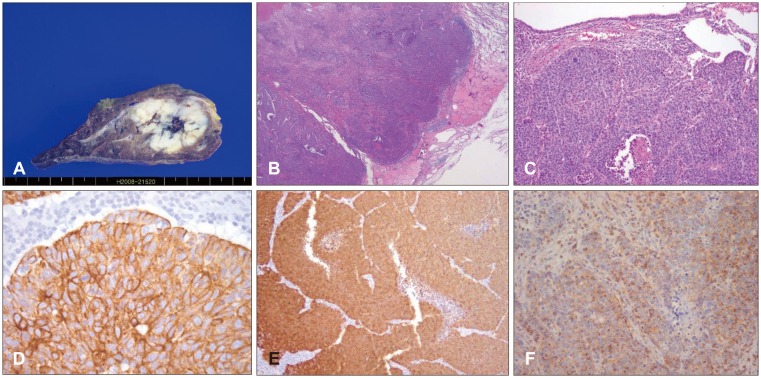
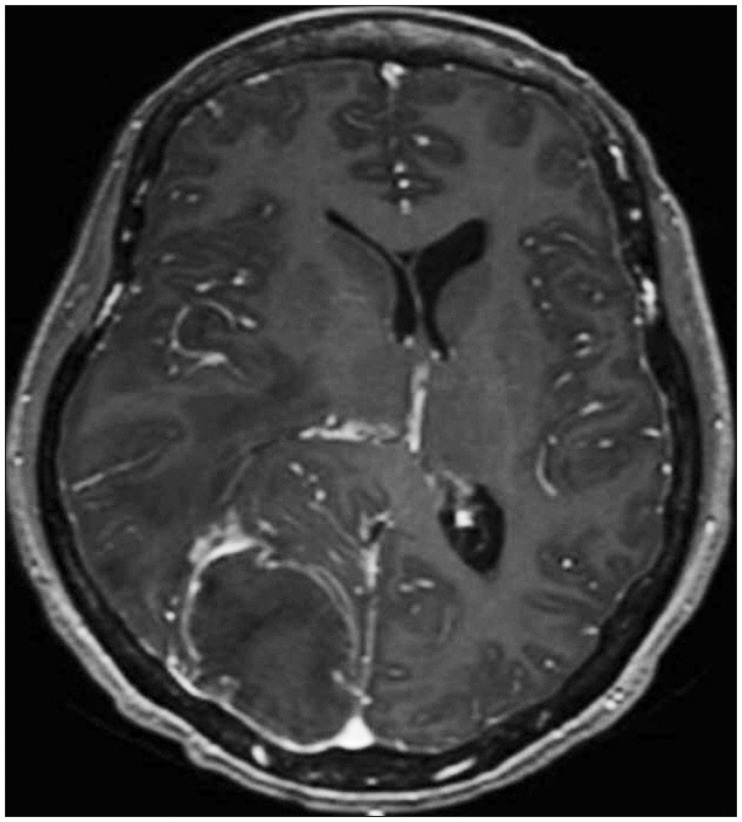
FIGURE 2
Brain magnetic resonance imaging with contrast enhancement. Shows 6×4-cm rim enhanced mass with vasogenic edema in the right parieto-occipital lobe.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download