Abstract
Objective
The purpose of this study was to analyze the clinical manifestations, radiological findings, treatment results, and clinical significance of post-traumatic syringomyelia (PTS).
Methods
We retrospectively reviewed the medical charts of nine surgical patients with symptomatic PTS between 1992 and 2012.
Results
The most common clinical manifestation was development of new motor weakness. The mean interval between the initial injury and the onset of new symptoms 21.9 years. The mean length of the syringes observed on preoperative magnetic resonance images was 7.8 spinal levels. Shunting procedures were performed in five patients. Four patients underwent arachnoidolysis and duraplasty. Patients developed mechanical shunt failure. Postoperatively, one patient showed clinical improvement, four patients were stable, and four patients showed deterioration.
Post-traumatic syringomyelia (PTS) is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord after a trauma. PTS was rarely reported, and the significance of the past history of spinal trauma was overlooked. Symptomatic PTS has a reported prevalence of 4%,4) but the prevalence of asymptomatic PTS among patients with spinal cord injuries (SCIs) is estimated at approximately 28%.9) PTS generally develops within 5 years after the initial spinal injury, but ranges from 6 months to 25 years.2)
The pathophysiology of PTS is not completely understood. It has been proven that post-traumatic arachnoiditis can cause cavitation in the spinal cord and may also cause syringomyelia. The delayed development of syringomyelia after a severe single spinal trauma that results in contusion of the spinal cord without the complication of arachnoiditis is well-known issue. PTS has been treated by shunting procedure or decompression, and outcomes were poor. The purpose of this study was to review the clinical manifestations and surgical treatment results of PTS.
Between 1992 and 2012, nine patients with symptomatic PTS underwent operations. All the patients had evident and progressive neurological symptoms. We excluded patients with congenital anomalies or tumors related to syringomyelia from this analysis. In all nine patients, the syringomyelia was caused by spinal trauma. These patients were examined with preoperative magnetic resonance images (MRI). MRI was used to analyze the injury site, craniocaudal extension of the syrinx, the degree of spinal stenosis, and the quality of the subarachnoid spaces around the syrinx. By the late 1990's, patients underwent the shunting procedures. Arachnoidolysis and duraplasty were performed after the late 1990's. The mean follow-up period was 9.3 years (range, 2-17 years). The major presenting symptoms or signs were assessed in terms of their improvement, stabilization and deterioration.
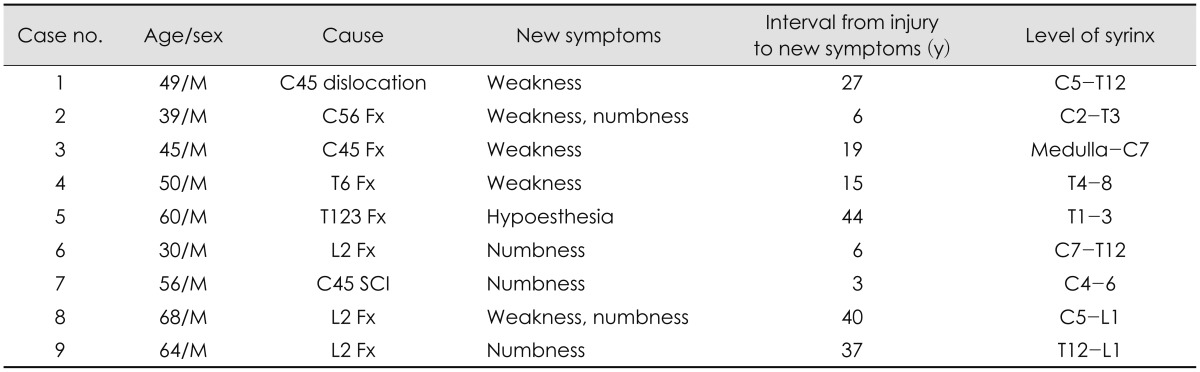
The patients consisted of nine men who were between 30 and 68 years of age (mean, 51.2 years). The mean age at the time of injury was 27.7 years (range, 20-45 years). The mechanisms of injury included a motor vehicle accident in four patients, a fall in four patients, and spinal injury in one patient. Spinal fractures occurred in seven patients, spinal dislocation in one patient, and SCI in one patient. The time intervals between the initial injury and the onset of new symptoms varied greatly, ranging from 3 to 44 years (mean, 21.9 years). Motor weakness in five patients was the most frequent new symptoms, followed by sensory disturbances and pain in four patients, and bladder disturbance in one patient (Table 1).
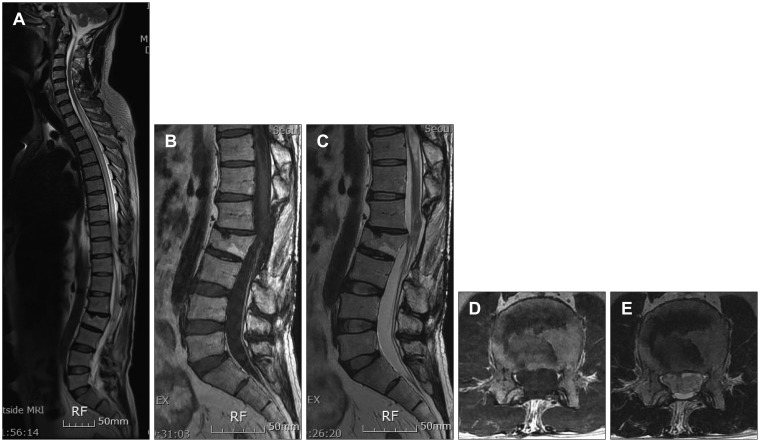
The levels of injury were cervical in four patients, thoracic in two patients, and lumbar in three patients. MRI was the imaging modality of choice for diagnosis. MRI demonstrated syringes and associated abnormalities. Preoperative MRI demonstrated syringes in anywhere from 2 to 16 spinal levels (mean, 7.8 levels). Two patients showed syrinxes at the thoracic levels. The syrinxes existed at the thoracic levels and extended to the cervical level in three patients and to the lumbar level in one patient. Two patients showed syrinxes at the cervical level. In this study, three patients had syrinx extending above and below the site of the original lesion, three patients had syrinx extending above the original lesion, two patients had syrinx extending below the original lesion, and one patient had syrinx at the original lesion. Syrinx extended rostrally into the medulla in one patient. The last patient showed syrinxes at the level of the whole cord (Figure 1).
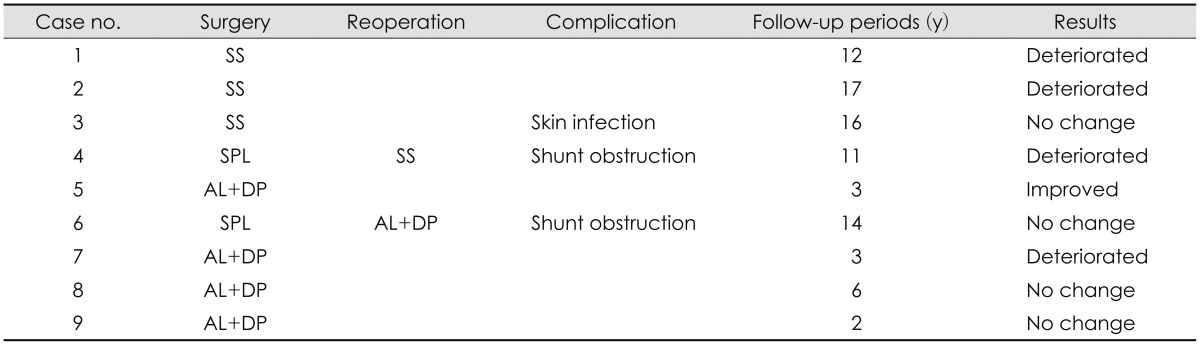
Nine patients underwent surgical intervention. Five patients underwent shunt placement (three syringo-subarachnoid shunts, two syringo-pleural shunt). Arachnoidolysis and syringes were performed in four patients. In five patients with shunting procedures, two patients underwent further operations because of shunt failure. Postoperative complications occurred in three patients with shunt placement: two patients experienced mechanical shunt failure and one patient had an infection at the operative site (Table 2).
At the final follow-up, four patients showed no neurological change, four patients experienced worsening of their neurological symptoms, and one patient slightly improved with regards to trunk hypoesthesia. Of the five patients who underwent shunting procedures, two patients stabilized and three deteriorated. Of the four patients who underwent arachnoidolysis and duraplasty, two patients stabilized and one deteriorated. One patient improved slightly with regards to trunk hypoesthesia.
Two patients underwent the second operation. One patient underwent further shunt operation 7 years after the initial surgery because of paraparesis and spasticity progression and syrinx re-expansion. The other patient underwent arachnoidolysis and duraplasty as the second operation 12 years after the first shunt placement because of progressive pain and numbness.
PTS is an uncommon but increasingly recognized cause of morbidity following SCI. The development of a syrinx takes months to years after the initial injury. The most frequent presenting symptoms of PTS are pain, numbness or increased weakness, and the reported interval between spinal trauma and the presenting neurological symptoms ranges from 2 months to 36 years.13) In this study, most common symptom is the numbness and weakness and the mean interval between the initial injury and the onset of new symptoms was 21.9 years.
Previous reports showed that syrinx extension may be due to secondary distention of the epidural veins or pressure changes leading to cerebrospinal fluid (CSF) movement during a Valsalva maneuver.8) Furtheromre, PTS most commonly extends above from the injury site; though, less frequently, it may also have an inferior component.10) In this study, syringes usually extended above or above and below from spinal injury sites.
Surgery is performed on patients with syrinx that become symptomatic. Syringo-peritoneal shunts and syringo-pleural shunts are commonly used in patients with syringomyelia associated with spinal arachnoiditis because of adhesion in the spinal subarachnoid space.6) The placement of all types of shunts may be followed by significant morbidity requiring additional surgical procedures.1,3,5,7,11,12) Problems specific to the shunt operation include dislodged, blocked, and infected drains. Shunting procedures were widely used with encouraging early results, although long-term results has been questioned recently. They are not directed at the etiology of syringomyelia. A higher rate of shunt failure (approximately 50%) and poor long-term outcomes were reported from various shunting procedures.1,12) In this study, we performed shunting procedures in five patients; two patients stabilized and three deteriorated. Thus, our study outcome was similar to that of previous reports. Mechanical shunt failures occurred in two of the five patients. Shunt obstruction and spinal cord tethering may account for the gradual neurological deterioration.
The occurrence of pressure differences between the zone above the arachnoiditis and that below seems to be important. Permitting free communication among the CSF pathways so that there are no pressure differentials across the walls of the cord is exxential.14) Decompressive procedures may have beneficial effects unless the patient shows longitudinally extensive arachnoiditis. The first line of treatment should focus on restoring the normal CSF flow at the trauma level and untethering the cord and duroaplasty.12)
In this study, the post-traumatic tethering, which may lead to a progressive myelopathy, could not be released well. Of the 4 patients who underwent arachnoidolysis and duraplasty, two patients showed no neurological changes, one patient improved, and one patient deteriorated. Arachnoidolysis and duraplasty had no better long-term results than shunt-ing operations.
References
1. Batzdorf U, Klekamp J, Johnson JP. A critical appraisal of syrinx cavity shunting procedures. J Neurosurg. 1998; 89:382–388. PMID: 9724111.

2. Carroll AM, Brackenridge P. Post-traumatic syringomyelia: a review of the cases presenting in a regional spinal injuries unit in the north east of England over a 5-year period. Spine (Phila Pa 1976). 2005; 30:1206–1210. PMID: 15897837.
3. Edgar R, Quail P. Progressive post-traumatic cystic and non-cystic myelopathy. Br J Neurosurg. 1994; 8:7–22. PMID: 8011197.

4. el Masry WS, Biyani A. Incidence, management, and outcome of post-traumatic syringomyelia. In memory of Mr Bernard Williams. J Neurol Neurosurg Psychiatry. 1996; 60:141–146. PMID: 8708641.

5. Hida K, Iwasaki Y, Imamura H, Abe H. Posttraumatic syringomyelia: its characteristic magnetic resonance imaging findings and surgical management. Neurosurgery. 1994; 35:886–891. discussion 891. PMID: 7838337.
6. Kaynar MY, Koçer N, Gençosmanoğlu BE, Hanci M. Syringomyelia--as a late complication of tuberculous meningitis. Acta Neurochir (Wien). 2000; 142:935–938. discussion 938-939. PMID: 11086834.
7. Klekamp J, Batzdorf U, Samii M, Bothe HW. Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma. J Neurosurg. 1997; 86:233–240. PMID: 9010425.

8. Parziale JR, Frates EP. Dyspnea: an unusual presentation of posttraumatic syringomyelia. Am J Phys Med Rehabil. 2006; 85:185–186. PMID: 16428913.

9. Perrouin-Verbe B, Lenne-Aurier K, Robert R, Auffray-Calvier E, Richard I, Mauduyt de la Grève I, et al. Post-traumatic syringomyelia and post-traumatic spinal canal stenosis: a direct relationship: review of 75 patients with a spinal cord injury. Spinal Cord. 1998; 36:137–143. PMID: 9495005.

10. Quencer RM, Green BA, Eismont FJ. Posttraumatic spinal cord cysts: clinical features and characterization with metrizamide computed tomography. Radiology. 1983; 146:415–423. PMID: 6849087.

11. Sgouros S, Williams B. A critical appraisal of drainage in syringomyelia. J Neurosurg. 1995; 82:1–10. PMID: 7815110.

12. Sgouros S, Williams B. Management and outcome of posttraumatic syringomyelia. J Neurosurg. 1996; 85:197–205. PMID: 8755746.

13. Umbach I, Heilporn A. Review article: post-spinal cord injury syringomyelia. Paraplegia. 1991; 29:219–221. PMID: 1870887.
14. Williams B. Post-traumatic syringomyelia, an update. Paraplegia. 1990; 28:296–313. PMID: 2235038.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download