Abstract
Intracranial traumatic pseudoaneurysms are rare, and their vessel structures are immature and easy to disrupt, especially in children. Furthermore, it is difficult to diagnose and treat, which is a characteristic of traumatic pseudoaneurysm. In this study, the authors described a traumatic pseudoaneurysm in A2 segment of anterior cerebral artery, and the treatment with stent for structural stability of vessel.
Traumatic pseudoaneurysms are rare cases, and they occupy less than 1% of all intracranial aneurysms. In spite of their high mortality of 30%, it is difficult to diagnose for their rarity.1)
The development of traumatic pseudoaneurysm depends on the mechanism of injury. It can occur after a penetrating or closed head injury, and also after an intracranial surgery such as transsphenoidal surgery, sinus surgery, ventricular taps, stereotactic brain biopsy, and endoscopic third ventriculostomy.4,5,12,14)
Here, we recently experienced the case of traumatic pseudoaneurysm treated with endovascular embolization in a child. We always should keep in mind that the case of falx subdural hematoma (SDH) after head trauma has the possibility of traumatic pseudoaneurysm, and it requires vascular work-up.
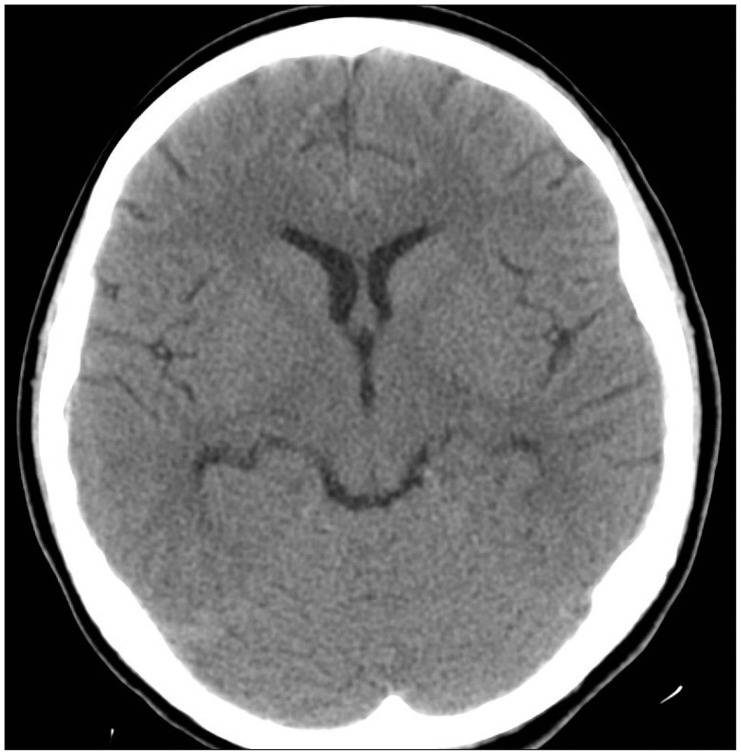
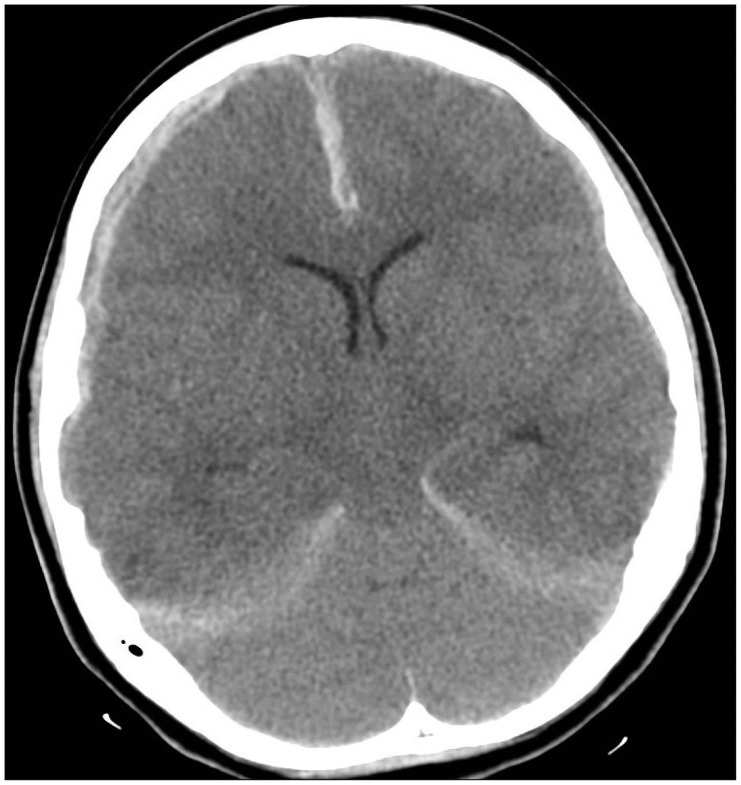
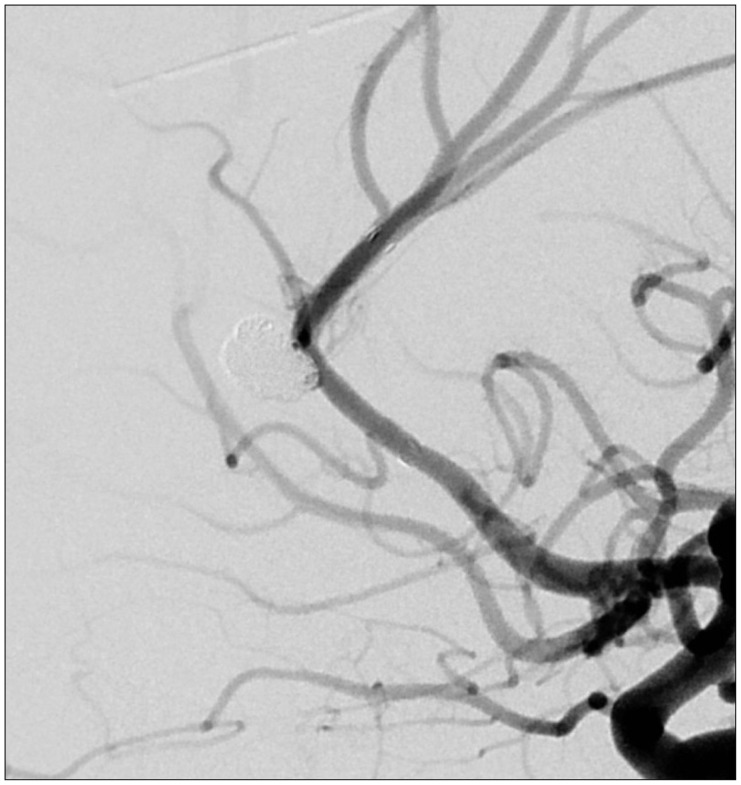
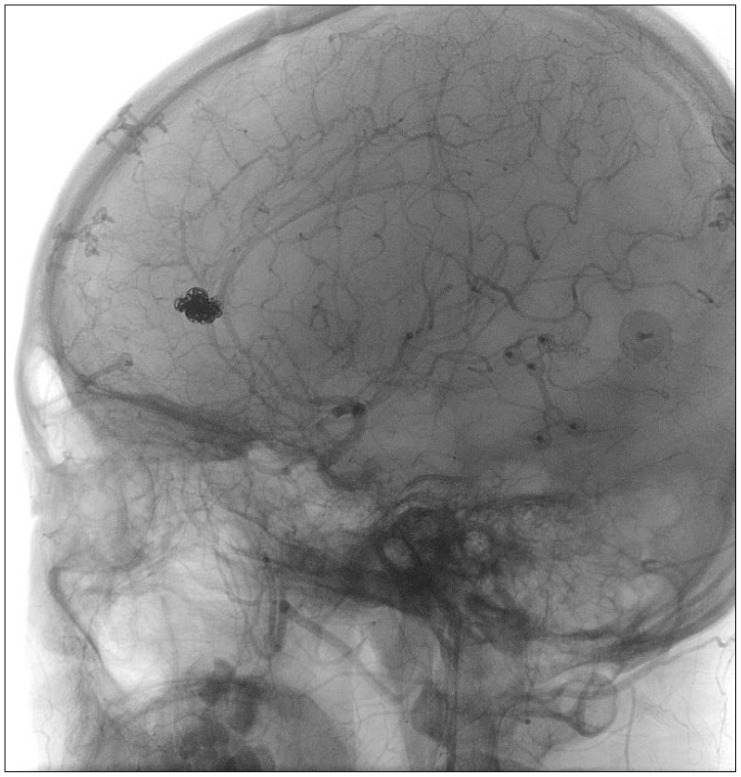
A thirteen-year-old girl was admitted to our medical center due to a traffic accident. She was in a stuporous state, and Glasgow coma scale was checked by E2V1M4. We immediately checked brain computed tomography (CT). On the initial brain CT, a small amount of acute SDH and anterior falx SDH were seen on the right convexity (Figure 1). She was admitted to the general ward and was diagnosed of SDH combined with diffuse axonal injury. We carefully observed her, and her mental state was improved to an alert state one week after the initial trauma. Her follow-up CT, which was performed 1 week after the initial trauma, was shown to be clear of hemorrhage (Figure 2). Her general condition and mental state recovered as time passed. But ten days after the initial trauma, she suffered a sudden attack of seizure and her mental state decreased to a comatose. On follow-up brain CT, a reappearance of convexity and falx SDH showed with severe and diffuse brain swelling (Figure 3). There was no subarachnoid hemorrhage. Immediate decompressive craniectomy and hematoma removal were performed. One day after the operation, we performed an angiography to identify the existence of traumatic pseudoaneurysm. From angiography, we found the traumatic pseudoaneurysm in A2 artery. For her previous craniectomy, anti-thrombotic agent could not be treated premedication. Eleven days after the initial trauma, endovascular embolization was performed (Figure 4). During the operation, stent insertion was preferentially done for instability of vessel. Coil packing for aneurysm was also performed. After endovascular embolization, we administered the patient with anti-thrombotic agent, aspirin, and plavix. On 1 year postoperative follow-up angiography, there was no recanalization at embolized traumatic pseudoaneurysm and her neurological symptom was improved to alert state (Figure 5).
We report a case of traumatic pseudoaneurysm formed at A2 artery, which resulted from a high-velocity, non-penetrating injury. Traumatic pseudoaneurysms can be developed through certain mechanisms, and they are categorized into low-velocity injuries and high-velocity injuries. In our case, the injury was high-velocity and blunt trauma.1) These pseudoaneurysms can create severe neurological defects such as decreased mental state, paralysis, or even death.9)
The traumatic pseudoaneurysms are developed by the disruption of elements of the vessel wall involving intima, media, and adventitia. This condition of vessel leads to instability and causes formation of traumatic pseudoaneurysm, dissection, and fistula.3,8)
It is hard to decide the proper treatment method for pseudoaneurysm. The traditional method of treatment is surgical clipping for aneurysm, but this method is often not possible, as pseudoaneurysms are unstable and are generally false aneurysms.6) When surgical method is performed, excision of the involved vessel is considered. When proximal vessels are involved, bypass surgery should be considered. For the last three decades, endovascular technique for pseudoaneurysm has not been a mainstay, due to the high incidence of false aneurysms and risk of rupturing induced by structural instability of pseudoaneurysm.4,11,13) But recently, there are some reports of traumatic pseudoaneurysms which were treated by endovascular embolization, and many of them were treated with satisfying results. In our case, we considered both bypass surgery and endovascular embolization for pseudoaneurysm. We chose endovascular treatment because the patient's neurological status and condition were too poor to proceed with bypass surgery. Technically, it would also be difficult to proceed with bypass surgery because of the patient's high intracranial pressure. Considering risk of rebleeding, we decided to proceed with endovascular embolization for the traumatic pseudoaneurysm despite risk for occlusion of parent artery. The stent insertion was performed during the operation in order to make a structural stability of pseudoaneurysm.
In some cases, traumatic pseudoaneurysms disappeared spontaneously.7) Amirjamshidi et al.2) reported that 19.4% of the aneurysms found to disappear spontaneously. But considering the mortality rate of pseudoaneurysm, once a traumatic pseudoaneurysm is diagnosed, treatment should be recommended.
In most of the cases, the pathogenic mechanism of posttraumatic falx SDH is linked to venous tearing involving the parasagittal bridging veins. These veins are stretched by the tangential forces.10) A2 arteries are neighbored with bridging vein. In our case, the forces of falx affected A2 artery and adventitia of vessel was injured.
We experienced a successful endovascular treatment of traumatic pseudoaneurysm resulting from high-velocity and non-penetrating trauma in a child. As seen in this case, an evaluation of vascular abnormality formation should be considered when falx SDH is seen initially, or appearance of hemorrhage occurs during a resolving state of primary hemorrhage after a head trauma, and when the mechanism of trauma is penetrating or high-velocity non-penetrating. The endovascular treatment with stent can be an alternative choice for traumatic pseudoaneurysms.
References
1. Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am. 1995; 6:775–797. PMID: 8527918.

2. Amirjamshidi A, Rahmat H, Abbassioun K. Traumatic aneurysms and arteriovenous fistulas of intracranial vessels associated with penetrating head injuries occurring during war: principles and pitfalls in diagnosis and management. A survey of 31 cases and review of the literature. J Neurosurg. 1996; 84:769–780. PMID: 8622150.
3. Britz GW, Mayberg MR. Pathology of cerebral aneurysms and subarachnoid hemorrhage. In : Welch KMA, Caplan LR, Reis DJ, Siesjö BK, Weir B, editors. Primer on cerebrovascular diseases. San Diego, CA: Academic Press;1997. p. 498–502.
4. Ciceri EF, Regna-Gladin C, Erbetta A, Chiapparini L, Nappini S, Savoiardo M, et al. Iatrogenic intracranial pseudoaneurysms: neuroradiological and therapeutical considerations, including endovascular options. Neurol Sci. 2006; 27:317–322. PMID: 17122940.

5. Dunn IF, Woodworth GF, Siddiqui AH, Smith ER, Vates GE, Day AL, et al. Traumatic pericallosal artery aneurysm: a rare complication of transcallosal surgery. Case report. J Neurosurg. 2007; 106(2 Suppl):153–157. PMID: 17330545.
6. Golshani K, Britz GW, Yoo A, West GA. Traumatic cerebral aneurysms secondary to penetrating intracranial injuries. In : Winn HR, editor. Youmans neurological surgery. ed 6. Philadelphia, PA: Saunders;2011. p. 4000–4003.
7. Halbach VV, Higashida RT, Hieshima GB, Goto K, Norman D, Newton TH. Dural fistulas involving the transverse and sigmoid sinuses: results of treatment in 28 patients. Radiology. 1987; 163:443–447. PMID: 3562824.

8. Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin. 1983; 1:155–182. PMID: 6680158.

9. Kieck CF, de Villiers JC. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984; 60:42–46. PMID: 6689727.

10. Lee M, Kim MS, Yoon SW. Interhemispheric subdural hematoma presenting with falx syndrome after trauma. J Korean Neurotraumatol Soc. 2010; 6:158–161.

11. Lempert TE, Halbach VV, Higashida RT, Dowd CF, Urwin RW, Balousek PA, et al. Endovascular treatment of pseudoaneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 1998; 19:907–911. PMID: 9613510.
12. Rayes M, Bahgat DA, Kupsky WJ, Mittal S. Middle cerebral artery pseudoaneurysm formation following stereotactic biopsy. Can J Neurol Sci. 2008; 35:664–668. PMID: 19235456.

13. Rückert RI, Rutsch W, Filimonow S, Lehmann R. Successful stent-graft repair of a vertebrojugular arteriovenous fistula. J Endovasc Ther. 2001; 8:495–500. PMID: 11718408.

14. Zanini MA, Borges RA, Nunes Aquino GH, de Freitas CC. Iatrogenic cortical aneurysm post-craniotomy. Br J Neurosurg. 2010; 24:214–215. PMID: 20121386.

FIGURE 1
On initial brain computed tomography, a small amount of acute subdural hematoma (SDH) and anterior falx SDH were seen on the right convexity.
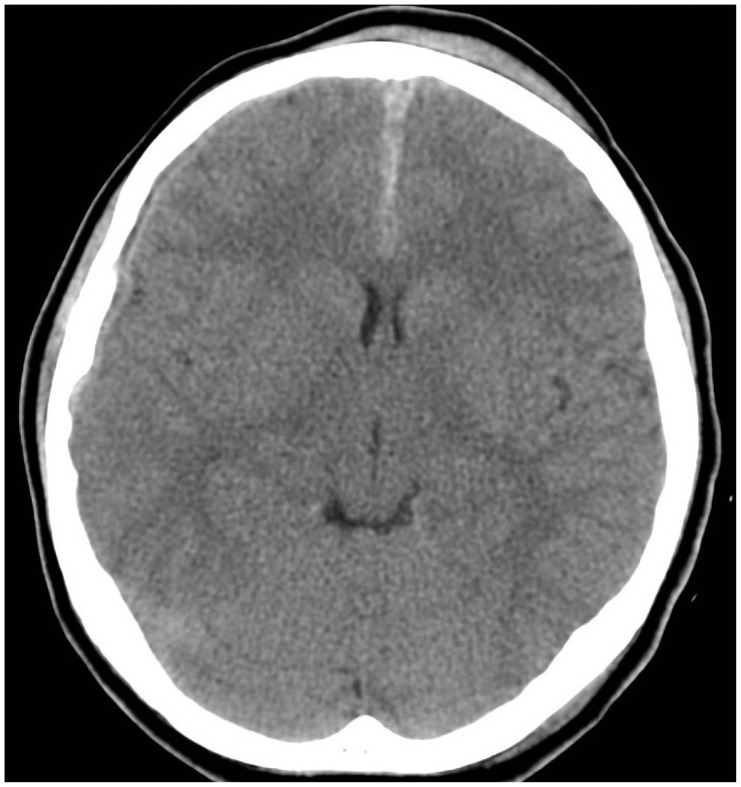
FIGURE 2
Follow-up computed tomography, which was performed 1 week after the initial trauma, was shown to be clear of hemorrhage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download