Abstract
Purpose
Allergic rhinitis (AR) is a common chronic disease. Many factors could affect the development of AR. We investigated early-life factors, such as delivery mode, feeding method, and use of antibiotics during infancy, which could affect the development of AR. In addition, how interactions between these factors and innate gene polymorphisms influence the development of AR was investigated.
Methods
A cross-sectional study of 1,828 children aged 9-12 years was conducted. Three early-life factors and AR were assessed by a questionnaire. Skin prick tests were done. Polymorphisms of TLR4 (rs1927911) and CD14 (rs2569190) were genotyped.
Results
Use of antibiotics during infancy increased the risk of AR (aOR [95% CI] 1.511 [1.222-2.037]) and atopic AR (aOR [95% CI], 1.565 [1.078-2.272]). There were synergistic interactions between caesarean delivery, formula feeding, and use of antibiotics in the rate of atopic AR (aOR [95% CI], 3.038 [1.256-7.347]). Additional analyses revealed that the risk for the development of AR or atopic AR subjects with the TLR4 CC genotype were highest when all the 3 early-life factors were present (aOR [95% CI], 5.127 [1.265-20.780] for AR; 6.078 [1.499-24.649] for atopic AR). In addition, the risk for the development of AR or atopic AR in subjects with the CD14 TT genotype were highest when all the 3 early-life factors were present (aOR [95% CI], 5.960 [1.421-15.002] for AR; 6.714 [1.440-31.312] for atopic AR).
Allergic rhinitis (AR) is a common atopic and chronic disease in childhood. The International Study of Asthma and Allergies in Childhood (ISAAC) was conducted in Korea, and the lifetime prevalence of AR was gradually increased to 16.8% in 1995 and 22.0% in 2000.1 Environmental factors as well as genetic predisposition seem to be risk factors contributing to the development of AR.2
In 1989, the hygiene hypothesis was developed for increasing allergic diseases. It proposed that a lack of exposure to microbes in early life increases the risk of allergy in later life.3,4 This was adapted to the microbiota hypothesis, namely, microbiota changes by lifestyle factors and plays a major role in the development of the immune system.5,6,7 Delivery mode influences initial microbial colonization,6 and feeding method or use of antibiotics could affect the intestinal microbiota.8,9 Moreover, alterations in the microbiota lead to dysbiosis and disease in the neonate and affect long-term health in childhood.10
Intestinal microbiota may play an essential role in T helper 1 (Th1) cell immune responses and the balance between Th1 and Th2 cell immune responses. These immune responses involve major pathogen-recognition receptors like Toll-like receptors (TLRs) with cluster of differentiation (CD) 14 of innate immunity.11,12,13 Genetic polymorphisms that shape immune responses are associated with an increased risk of developing allergic disease. We previously reported the relationships between allergic disease and TLR4 (rs1927911)/CD14 (rs2569190).14,15,16 However, genetic predisposition alone cannot fully explain the rapid rise in the incidence of allergic disease; rather, it is likely that interactions between genes and the environment explain the increased risk of developing allergic disease.17
We investigated early-life risk factors for the development of AR by altering the intestinal microbiota, which included delivery mode, feeding method, and use of antibiotics during infancy. We also determined how genetic variations associated in CD14 (rs2569190) or TLR4 (rs1927911) could interact with early-life risk factors to promote the development of allergic disease.
In total, 1,828 children aged 9-12 years were recruited from 9 elementary schools in 2 areas in Korea, namely, Seoul and Jeongeup. Seoul is the largest urbanized city, and Jeongeup consists of a rural town and rural villages. Of the 1,828 subjects, 1,797 (98.3%) returned the questionnaires. AR patients were defined as children who were diagnosed with AR by the physician using the questionnaire, and atopic AR patients as children who were diagnosed with AR by the physician using the questionnaire as well as by skin prick test results.
This study was approved by the Human Ethics Committees of Hallym University and the principals of the schools attended by the children. Written informed consent was obtained from the parents or guardians of the children.
Demographic factors, potential explanatory and confounding factors, and the prevalence of diseases and symptoms were assessed by a questionnaire that was given to the parents. The written questionnaire based on the ISAAC protocol was translated into Korean.18 The presence of AR in the children was determined by asking specific questions, such as "Has your child ever been diagnosed with allergic rhinitis by a physician?". Delivery mode was determined by the question, "Was your child born by vaginal delivery or caesarian section?". Feeding method was determined by the question, "Was your child breast-fed or formula-fed?". Use of antibiotics during infancy was assessed by the question, "Did your child take antibiotics more than 3 days during infancy?".
Standardized allergen extracts and control solutions from Allergopharma (Reinbek, Germany) were used. The subjects were tested for the following 16 allergens: Dermatophagoides pteronyssinus, D. farinae, dog/cat epithelium, cockroach, grass, mixed tree pollen 1 and 2, Alternaria, Aspergillus, ragweed, mugwort, milk, egg white, peanut, and soybean. A positive reaction was defined as a wheal size ≥3 mm after subtracting the negative control. The skin prick test was performed on 1,510 children (84.0%). One or more positive reactions were considered to indicate atopy.
Genomic DNA was extracted from peripheral blood mononuclear cells, and CD14 (rs2569190), TLR4 (rs1927911) polymorphisms were screened using the TaqMan fluorogenic 5' nuclease assay (ABI, Foster City, CA, USA). The final volume in polymerase chain reaction (PCR) was 5 µL and consisted of 10 ng of genomic DNA, 2.5 µL of TaqMan Universal PCR Master Mix, and 0.13 µL of 40× Assay Mix (Assay ID C_16043997_10 and C_11722141_10). The thermal cycle conditions were as follows: 50℃ for 2 minutes to activate uracil N-glycosylase and to prevent carry-over contamination, 95℃ for 10 minutes to activate DNA polymerase, followed by 45 cycles of 95℃ for 15 seconds and 60℃ for 1 minute. All PCRs were performed by using 384-well plates and a 384-Well Veriti thermal cycler, and the endpoint fluorescent readings were performed by using an ABI 7900 HT Sequence Detection System. Duplicate samples and negative controls were included to ensure genotyping accuracy.
Multivariate logistic regression analysis was used to calculate adjusted odds ratios (aORs) for early-life factors and the association between genetic polymorphisms and the early-life factors with regard to the development of AR. The additive effect of the early-life factors in the context of genotypes was determined. All statistical methods were adjusted for predefined covariates, including sex, age, body mass index, maternal and paternal history of allergic disease, familial income, environmental tobacco smoke, and region. All statistical analyses were performed by using SPSS version 18.0 (SPSS Inc., Cary, NC, USA). The results are presented as aORs and 95% confidence intervals (95% CIs). A P value of <0.05 was considered statistically significant.
In total, 1,540 children answered the question about physician's diagnosis of AR. AR had been diagnosed by a physician in 24% (369/1,540) of the children. The demographic data obtained from children with and without AR are presented in Table 1. Children with AR showed a higher proportion of males and higher frequencies of parental allergic history, parental income, and residence in Seoul than those without. Caesarean delivery and breast feeding were not significantly different between the 2 groups. Children with AR more frequently took antibiotics during infancy.
The prevalence of atopic AR, which was diagnosed by physicians using positive skin prick test results, was 12.8% (197/1,540).
Delivery mode and feeding method were not associated with the rates of AR or atopic AR. Children who had been treated with antibiotics for more than 3 days during infancy were more frequently diagnosed with AR and atopic AR (aOR [95% CIs], 1.511 [1.222-2.037] for AR and aOR [95% CIs], 1.565 [1.078-2.272] for atopic AR) (Table 2).
The risks of AR and atopic AR tended to increase as the number of environmental risk factors became larger (Fig. 1).
Genotype analysis was performed on 1,299 children for CD14 and on 1,274 for TLR4. Hardy-Weinberg equilibrium tests demonstrated no significant deviation (P>0.05) for the 2 polymorphisms in control subjects. The CD14 TT, TC, and CC genotypes occurred at frequencies of 39.6% (514/1,299), 47.4% (616/1,299), and 13.0% (169/1,299), respectively, while the TLR4 CC, CT, and TT genotypes occurred at frequencies of 35.2% (449/1,274), 48.2% (614/1,274), and 16.6% (211/1,274), respectively.
There was no significant association between the genetic polymorphisms and AR/atopic AR (Supplemental Table 1).
When environmental factors were analyzed in relation to genetic polymorphisms, use of antibiotics during infancy was significantly associated with the CD14 TT genotype in AR and the TLR4 CC genotype in atopic AR. Formula feeding was associated with the CD14 CT+CC genotypes and the TLR4 CT+TT genotypes in atopic AR (Table 3).
Additional analyses were performed to examine the effect of the number of risk factors on the rates of AR or atopic AR in children with different genetic polymorphisms. With regard to CD14 and TLR4 polymorphism, the risks of AR and atopic AR tended to increase as the number of environmental risk factors became larger (Figs. 2 and 3). When all the 3 early-life risk factors were present, the risks of AR and atopic AR were higher in subjects with the TLR4 CC genotype than in those with other genotypes (aOR [95% CIs], 5.127 [1.265-20.780] for AR and aOR [95% CIs], 6.078 [1.499-24.649] for atopic AR) (Fig. 2). When all the 3 early-life risk factors were present, the risks of AR and atopic AR were higher in subjects with the CD14 TT genotype than in those with other genotypes (aOR [95% CIs], 5.960 [1.421-25.002] for AR and aOR [95% CIs], 6.714 [1.440-31.312] for atopic AR) (Fig. 3). The early-life risk factors differently affected genetic polymorphisms.
In our study, use of antibiotics during infancy increased the development of AR and atopic AR. As the number of early-life risk factors became larger, the subjects were more frequently diagnosed with atopic AR in childhood. In addition, the factors interacted with polymorphisms of the TLR4 or CD14 gene when the subjects had 3 risk factors and the TLR4 CC or CD14 TT genotype. This suggests that the risk of AR and atopic AR may increase when subjects with certain genotypes were born by caesarian delivery, were formula-fed, and took antibiotics during infancy.
The 3 early-life factors are similar, which influence the intestinal microbiota and thus alter immune responses.19 In our study, the risk of AR was highest when all the 3 risk factors were present. This suggests that caesarean delivery, formula feeding, and use of antibiotics during infancy may act synergistically to promote the risk of AR, probably by influencing the intestinal microbiota in a synergistic manner.
With regard to delivery mode, neonates born by vaginal delivery are exposed to the mother's vaginal and intestinal flora as they pass through the birth canal, and consequently their bacterial communities resemble their mother's flora.7 Subjects born by caesarean section have microbial colonization later; the lack of exposure to the maternal vaginal and intestinal flora results in colonization with different species of bacteria.7,20
There have been many studies that suggest breast milk protects against allergic disease. Breast milk contains multiple immunomodulatory compounds, including IgA antibodies to microorganisms, nucleotides, oligosaccharides, antimicrobial proteins, and food proteins.21,22 Bioactive molecules in breast milk could modulate neonatal gut microbiota composition, and lactating mothers introduce their gut microbiota to infants.23
The present study showed that use of antibiotics during infancy was associated with a higher risk of developing AR. Many previous studies have also shown that early use of antibiotics promotes the development of allergic disease.24,25 Even though antibiotics are more often prescribed to children who are predisposed to develop allergic disease,26 recent epidemiologic studies have demonstrated that changes in the microbiota as a consequence of early use of antibiotics can result in the dysregulation of host immune homeostasis and an increased risk of atopy and allergic disease.27,28,29 This may reflect that early use of antibiotics shifts the composition of the microbiota, changes in metabolites, and loss of required nutrients, followed by mucosal immunity.9
In our study, the CC genotype of TLR4 rs1927911 showed a higher risk of being diagnosed with AR if subjects were born by caesarian section, were formula-fed, and took antibiotics during infancy. Several previous studies have indicated that these 3 risk factors are associated with TLRs. Vaginal delivery enhances the expressions of TLR2 and TLR4 in neonatal monocytes.30 Breast-feeding is known to influence TLR-mediated cytokine responses of neonates31 and to modulate interactions between the host immune system and the gut microbiota.23 Antibiotics targeting Gram-negative bacteria would primarily affect TLR4, and consequently depletion of the microbiota after antibiotic treatment results in reduced TLR signaling and downstream regulation of innate defenses.32
Also, some evidence indicates that the intestinal microbiota has immunomodulatory effects through activation of pattern recognition receptors, including TLRs.33 Activation of TLR signaling by intestinal commensal bacteria can induce growth factors and cytokines that are required to exert cytoprotective and reparative effects on intestinal epithelial cells.34 In addition, TLR4 recognition of lipopolysaccharide is capable of inducing CD25 and Foxp3 expression in lamina propria lymphocytes and modulates regulatory T-cell responses in the gut.35,36 Through these mechanisms, TLR signaling pathways have been implicated in protection against allergic disease.36 Therefore, alteration and depletion of the microbiota change TLR signaling, followed by downstreaming innate defense and regulatory mechanisms, consequentially increasing allergic disease.9,36,37
Even though several SNPs of TLR4 have been investigated in most studies,38,39,40 TLR4 rs1927911 has been reported in a few studies on allergy. Penders et al.38 have documented a decreased risk of sensitization in children with the rs10759931 TLR CC genotype, Kerkhof et al.40 have reported that the risk of physician-diagnosed asthma increases with increasing PM2.5 levels at the birth address in children with the TT genotype of TLR4 rs1927911. To the best of our knowledge, there is no report on TLR4 rs1927911 with AR. In our study, the subjects with CC genotype of TLR4 rs1927911 had a higher risk of AR than those with other genotypes, which is the first report on their relationship.
CD14 is involved in the recognition and signal transduction of bacterial endotoxin along with TLR4.41 Simpson et al.43 have reported the association between CD14 rs2569190 polymorphism and endotoxin exposure in relation to allergic sensitization. In children with the C allele of CD14 SNP, increasing endotoxin exposure is associated with a reduction in the risk of sensitization, whereas in those with the T allele, increasing endotoxin exposure is not so.42,43 It has been indicated that children with the TT genotype have a significantly higher mean total IgE level and a higher prevalence of atopy by the active use of mite allergen-impermeable mattress covers and that serum IgE levels are similar regardless of the use of mite allergen impermeable mattress covers in children with the TT genotype.44,45 However, it has been reported that the prevalence of atopy increases through the active multifaceted intervention program in children with CC/CT genotypes and that the risk of sensitization increases in those with CC genotypes related to E. coli colonization.38,46
The present study included a relatively large number of samples and achieved a high response rate. This is the first study to investigate whether TLR4 rs1927911 or CD14 rs2569190 polymorphisms interact with early-life environmental factors in a synergistic manner, which may have influenced the intestinal microbiota to promote the development of AR and atopic AR. The present study has some limitations. First, a question arises whether the parental recall of use of antibiotics in infancy could be reliable. Second, fecal sample analysis that depicts the effect of environmental factors on the intestinal microbiota during early childhood was not performed in the present study. Nevertheless, the present study suggests that in subjects who have different genotypes of innate immunity genes, development of AR may depend on caesarean delivery, formula feeding, and use of antibiotics during infancy. It is meaningful that some environmental factors influencing the intestinal microbiota contribute to the development of AR. Further prospective studies are needed to confirm our results.
In conclusion, the present study showed that early-life risk factors significantly interacted with polymorphisms of the TLR4 and CD14 gene in pediatric patients with AR. The results of the present study suggest that the development of AR may be influenced by interactions between early-life risk factors and that the interactions can be modified by genetic polymorphisms. Therefore, early microbial contact through vaginal delivery, breast feeding method, and use of antibiotics during infancy could be effective in modulating risk factors of AR.
Figures and Tables
Fig. 1
The adjusted odds ratios of allergic rhinitis and atopic allergic rhinitis increase as the number of early-life environmental risk factors increases. The data are adjusted for age, sex, parental income, parental history of allergic diseases, body mass index, exposure to tobacco smoke, and region. *P<0.05. AR, allergic rhinitis.

Fig. 2
The adjusted odds ratios of allergic rhinitis and atopic allergic rhinitis increase when subjects have all the 3 early-life environmental risk factors and the CC genotype of TLR4. The data are adjusted for age, sex, parental income, parental history of allergic diseases, body mass index, exposure to tobacco smoke, and region. *P<0.05.

Fig. 3
The adjusted odds ratio of allergic rhinitis or atopic allergic rhinitis increase when subjects have all the 3 early-life environmental risk factors and the TT genotype of CD14. The data are adjusted for age, sex, parental income, parental history of allergic diseases, body mass index, exposure to tobacco smoke, and region. *P<0.05.

Table 1
General characteristics of the study subjects and the prevalence of allergic rhinitis

Table 2
Influence of early-life environmental factors in the development of allergic rhinitis and atopic allergic rhinitis in childhood
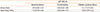
Table 3
Influence of early-life environmental factors in the development of allergic rhinitis and atopic allergic rhinitis according to genotypes

ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare, Republic of Korea (A092076).
References
1. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008; 51:343–350.
2. Kim WK, Kwon JW, Seo JH, Kim HY, Yu J, Kim BJ, et al. Interaction between IL13 genotype and environmental factors in the risk for allergic rhinitis in Korean children. J Allergy Clin Immunol. 2012; 130:421–426.e5.
3. Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989; 299:1259–1260.
4. Lee SY, Kwon JW, Seo JH, Song YH, Kim BJ, Yu J, et al. Prevalence of atopy and allergic diseases in Korean children: associations with a farming environment and rural lifestyle. Int Arch Allergy Immunol. 2012; 158:168–174.
5. Orrhage K, Nord CE. Factors controlling the bacterial colonization of the intestine in breastfed infants. Acta Paediatr Suppl. 1999; 88:47–57.
6. Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010; 107:11971–11975.
7. Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics. 2006; 118:511–521.
8. Fallani M, Young D, Scott J, Norin E, Amarri S, Adam R, et al. Intestinal microbiota of 6-week-old infants across Europe: geographic influence beyond delivery mode, breast-feeding, and antibiotics. J Pediatr Gastroenterol Nutr. 2010; 51:77–84.
9. Willing BP, Russell SL, Finlay BB. Shifting the balance: antibiotic effects on host-microbiota mutualism. Nat Rev Microbiol. 2011; 9:233–243.
10. Murgas Torrazza R, Neu J. The developing intestinal microbiome and its relationship to health and disease in the neonate. J Perinatol. 2011; 31:Suppl 1. S29–S34.
11. Koppelman GH, Reijmerink NE, Colin Stine O, Howard TD, Whittaker PA, Meyers DA, et al. Association of a promoter polymorphism of the CD14 gene and atopy. Am J Respir Crit Care Med. 2001; 163:965–969.
12. Baldini M, Lohman IC, Halonen M, Erickson RP, Holt PG, Martinez FD. A Polymorphism* in the 5' flanking region of the CD14 gene is associated with circulating soluble CD14 levels and with total serum immunoglobulin E. Am J Respir Cell Mol Biol. 1999; 20:976–983.
13. Tesse R, Pandey RC, Kabesch M. Genetic variations in toll-like receptor pathway genes influence asthma and atopy. Allergy. 2011; 66:307–316.
14. Choi WA, Kang MJ, Kim YJ, Seo JH, Kim HY, Kwon JW, et al. Gene-gene interactions between candidate gene polymorphisms are associated with total IgE levels in Korean children with asthma. J Asthma. 2012; 49:243–252.
15. Hong SJ, Kim HB, Kang MJ, Lee SY, Kim JH, Kim BS, et al. TNF-alpha (-308 G/A) and CD14 (-159T/C) polymorphisms in the bronchial responsiveness of Korean children with asthma. J Allergy Clin Immunol. 2007; 119:398–404.
16. Kim HY, Jung YH, Hong K, Jang GC, Seo JH, Kwon JW, et al. Gene-environment interaction between Toll-like receptor 4 and mold exposure in the development of atopic dermatitis in preschool children. Allergy Asthma Respir Dis. 2013; 1:129–137.
17. Jones G. Susceptibility to asthma and eczema from mucosal and epidermal expression of distinctive genes. Curr Allergy Asthma Rep. 2007; 7:11–17.
18. Hong SJ, Kim SW, Oh JW, Rah YH, Ahn YM, Kim KE, et al. The validity of the ISAAC written questionnaire and the ISAAC video questionnaire (AVQ 3.0) for predicting asthma associated with bronchial hyperreactivity in a group of 13-14 year old Korean schoolchildren. J Korean Med Sci. 2003; 18:48–52.
19. Guarner F, Malagelada JR. Gut flora in health and disease. Lancet. 2003; 361:512–519.
20. Adlerberth I, Strachan DP, Matricardi PM, Ahrné S, Orfei L, Aberg N, et al. Gut microbiota and development of atopic eczema in 3 European birth cohorts. J Allergy Clin Immunol. 2007; 120:343–350.
21. Savilahti E, Tainio VM, Salmenperä L, Siimes MA, Perheentupa J. Prolonged exclusive breast feeding and heredity as determinants in infantile atopy. Arch Dis Child. 1987; 62:269–273.
22. Savilahti E. Interaction of early infant feeding, heredity and other environmental factors as determinants in the development of allergy and sensitization. Nestle Nutr Workshop Ser Pediatr Program. 2008; 62:157–168.
23. Rautava S, Luoto R, Salminen S, Isolauri E. Microbial contact during pregnancy, intestinal colonization and human disease. Nat Rev Gastroenterol Hepatol. 2012; 9:565–576.
24. Wjst M, Hoelscher B, Frye C, Wichmann HE, Dold S, Heinrich J. Early antibiotic treatment and later asthma. Eur J Med Res. 2001; 6:263–271.
25. McKeever TM, Lewis SA, Smith C, Collins J, Heatlie H, Frischer M, et al. Early exposure to infections and antibiotics and the incidence of allergic disease: a birth cohort study with the West Midlands General Practice Research Database. J Allergy Clin Immunol. 2002; 109:43–50.
26. Shreiner A, Huffnagle GB, Noverr MC. The "Microflora Hypothesis" of allergic disease. Adv Exp Med Biol. 2008; 635:113–134.
27. Verhulst SL, Vael C, Beunckens C, Nelen V, Goossens H, Desager K. A longitudinal analysis on the association between antibiotic use, intestinal microflora, and wheezing during the first year of life. J Asthma. 2008; 45:828–832.
28. Kozyrskyj AL, Ernst P, Becker AB. Increased risk of childhood asthma from antibiotic use in early life. Chest. 2007; 131:1753–1759.
29. Russell SL, Gold MJ, Hartmann M, Willing BP, Thorson L, Wlodarska M, et al. Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep. 2012; 13:440–447.
30. Shen CM, Lin SC, Niu DM, Kou YR. Labour increases the surface expression of two Toll-like receptors in the cord blood monocytes of healthy term newborns. Acta Paediatr. 2009; 98:959–962.
31. Belderbos ME, Houben ML, van Bleek GM, Schuijff L, van Uden NO, Bloemen-Carlier EM, et al. Breastfeeding modulates neonatal innate immune responses: a prospective birth cohort study. Pediatr Allergy Immunol. 2012; 23:65–74.
32. Brandl K, Plitas G, Mihu CN, Ubeda C, Jia T, Fleisher M, et al. Vancomycin-resistant enterococci exploit antibiotic-induced innate immune deficits. Nature. 2008; 455:804–807.
33. Round JL, Lee SM, Li J, Tran G, Jabri B, Chatila TA, et al. The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science. 2011; 332:974–977.
34. Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004; 118:229–241.
35. Shirai Y, Hashimoto M, Kato R, Kawamura YI, Kirikae T, Yano H, et al. Lipopolysaccharide induces CD25-positive, IL-10-producing lymphocytes without secretion of proinflammatory cytokines in the human colon: low MD-2 mRNA expression in colonic macrophages. J Clin Immunol. 2004; 24:42–52.
36. McLoughlin RM, Mills KH. Influence of gastrointestinal commensal bacteria on the immune responses that mediate allergy and asthma. J Allergy Clin Immunol. 2011; 127:1097–1107.
37. Wells JM, Loonen LM, Karczewski JM. The role of innate signaling in the homeostasis of tolerance and immunity in the intestine. Int J Med Microbiol. 2010; 300:41–48.
38. Penders J, Thijs C, Mommers M, Stobberingh EE, Dompeling E, Reijmerink NE, et al. Host-microbial interactions in childhood atopy: toll-like receptor 4 (TLR4), CD14, and fecal Escherichia coli. J Allergy Clin Immunol. 2010; 125:231–236.e1-5.
39. Arbour NC, Lorenz E, Schutte BC, Zabner J, Kline JN, Jones M, et al. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat Genet. 2000; 25:187–191.
40. Kerkhof M, Postma DS, Brunekreef B, Reijmerink NE, Wijga AH, de Jongste JC, et al. Toll-like receptor 2 and 4 genes influence susceptibility to adverse effects of traffic-related air pollution on childhood asthma. Thorax. 2010; 65:690–697.
41. Sly PD, Holt PG. Role of innate immunity in the development of allergy and asthma. Curr Opin Allergy Clin Immunol. 2011; 11:127–131.
42. Eder W, Klimecki W, Yu L, von Mutius E, Riedler J, Braun-Fahrländer C, et al. Opposite effects of CD 14/-260 on serum IgE levels in children raised in different environments. J Allergy Clin Immunol. 2005; 116:601–607.
43. Simpson A, John SL, Jury F, Niven R, Woodcock A, Ollier WE, et al. Endotoxin exposure, CD14, and allergic disease: an interaction between genes and the environment. Am J Respir Crit Care Med. 2006; 174:386–392.
44. Corver K, Kerkhof M, Brussee JE, Brunekreef B, van Strien RT, Vos AP, et al. House dust mite allergen reduction and allergy at 4 yr: follow up of the PIAMA-study. Pediatr Allergy Immunol. 2006; 17:329–336.
45. Woodcock A, Lowe LA, Murray CS, Simpson BM, Pipis SD, Kissen P, et al. Early life environmental control: effect on symptoms, sensitization, and lung function at age 3 years. Am J Respir Crit Care Med. 2004; 170:433–439.
46. Chan-Yeung M, Ferguson A, Watson W, Dimich-Ward H, Rousseau R, Lilley M, et al. The Canadian Childhood Asthma Primary Prevention Study: outcomes at 7 years of age. J Allergy Clin Immunol. 2005; 116:49–55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download