1. Leung DY, Bieber T. Atopic dermatitis. Lancet. 2003; 361:151–160.
2. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol. 2006; 118:209–213.
3. Kim HY, Jang EY, Sim JH, Kim JH, Chung Y, Park SH, Hwang EM, Han Y, Ahn K, Lee SI. Effects of family history on the occurrence of atopic dermatitis in infants. Pediatr Allergy Respir Dis. 2009; 19:106–114.
4. Bisgaard H, Halkjaer LB, Hinge R, Giwercman C, Palmer C, Silveira L, Strand M. Risk analysis of early childhood eczema. J Allergy Clin Immunol. 2009; 123:1355–1360.e5.
5. Wang IJ, Guo YL, Weng HJ, Hsieh WS, Chuang YL, Lin SJ, Chen PC. Environmental risk factors for early infantile atopic dermatitis. Pediatr Allergy Immunol. 2007; 18:441–447.
6. Miyake Y, Ohya Y, Tanaka K, Yokoyama T, Sasaki S, Fukushima W, Ohfuji S, Saito K, Kiyohara C, Hirota Y. Osaka Maternal and Child Health Study Group. Home environment and suspected atopic eczema in Japanese infants: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2007; 18:425–432.
7. Sebõk B, Schneider I, Harangi F. Primary Care Paediatricians in Baranya County. Familiar and environmental factors influencing atopic dermatitis in the childhood. J Eur Acad Dermatol Venereol. 2006; 20:418–422.
8. Matsunaga I, Miyake Y, Yoshida T, Miyamoto S, Ohya Y, Sasaki S, Tanaka K, Oda H, Ishiko O, Hirota Y. Osaka Maternal and Child Health Study Group. Ambient formaldehyde levels and allergic disorders among Japanese pregnant women: baseline data from the Osaka maternal and child health study. Ann Epidemiol. 2008; 18:78–84.
9. Purvis DJ, Thompson JM, Clark PM, Robinson E, Black PN, Wild CJ, Mitchell EA. Risk factors for atopic dermatitis in New Zealand children at 3.5 years of age. Br J Dermatol. 2005; 152:742–749.
10. Capristo C, Romei I, Boner AL. Environmental prevention in atopic eczema dermatitis syndrome (AEDS) and asthma: avoidance of indoor allergens. Allergy. 2004; 59:Suppl 78. 53–60.
11. Schäfer T, Heinrich J, Wjst M, Adam H, Ring J, Wichmann HE. Association between severity of atopic eczema and degree of sensitization to aeroallergens in schoolchildren. J Allergy Clin Immunol. 1999; 104:1280–1284.
12. Darsow U, Vieluf D, Ring J. The atopy patch test: an increased rate of reactivity in patients who have an air-exposed pattern of atopic eczema. Br J Dermatol. 1996; 135:182–186.
13. Solé D, Camelo-Nunes IC, Wandalsen GF, Pastorino AC, Jacob CM, Gonzalez C, Wandalsen NF, Rosário Filho NA, Fischer GB, Naspitz CK. Prevalence of symptoms of asthma, rhinitis, and atopic eczema in Brazilian adolescents related to exposure to gaseous air pollutants and socioeconomic status. J Investig Allergol Clin Immunol. 2007; 17:6–13.
14. Ibargoyen-Roteta N, Aguinaga-Ontoso I, Fernandez-Benitez M, Marin-Fernandez B, Guillen-Grima F, Serrano-Monzo I, Hermoso-de-mendoza J, Brun-Sandiumetge C, Ferrer-Nadal A, Irujo-Andueza A. Role of the home environment in rhinoconjunctivitis and eczema in schoolchildren in Pamplona, Spain. J Investig Allergol Clin Immunol. 2007; 17:137–144.
15. Eberlein-König B, Przybilla B, Kühnl P, Pechak J, Gebefügi I, Kleinschmidt J, Ring J. Influence of airborne nitrogen dioxide or formaldehyde on parameters of skin function and cellular activation in patients with atopic eczema and control subjects. J Allergy Clin Immunol. 1998; 101:141–143.
16. Hon KL, Leung TF, Ching G, Chow CM, Luk V, Ko WS, Ng PC. Patterns of food and aeroallergen sensitization in childhood eczema. Acta Paediatr. 2008; 97:1734–1737.
17. Herbarth O, Fritz GJ, Rehwagen M, Richter M, Röder S, Schlink U. Association between indoor renovation activities and eczema in early childhood. Int J Hyg Environ Health. 2006; 209:241–247.
18. Huss-Marp J, Eberlein-König B, Breuer K, Mair S, Ansel A, Darsow U, Krämer U, Mayer E, Ring J, Behrendt H. Influence of short-term exposure to airborne Der p 1 and volatile organic compounds on skin barrier function and dermal blood flow in patients with atopic eczema and healthy individuals. Clin Exp Allergy. 2006; 36:338–345.
19. Leung AD, Schiltz AM, Hall CF, Liu AH. Severe atopic dermatitis is associated with a high burden of environmental Staphylococcus aureus. Clin Exp Allergy. 2008; 38:789–793.
20. Schirmer WN, Pian LB, Szymanski MS, Gauer MA. Air pollution in internal environments and sick building syndrome. Cien Saude Colet. 2011; 16:3583–3590.
21. Hanifin JM, Rajka G. Diagnositc features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1980; Suppl 92. 44–47.
22. Choi H, Schmidbauer N, Sundell J, Hasselgren M, Spengler J, Bornehag CG. Common household chemicals and the allergy risks in pre-school age children. PLoS One. 2010; 5:e13423.
23. Kim H, Bernstein JA. Air pollution and allergic disease. Curr Allergy Asthma Rep. 2009; 9:128–133.
24. Charpin D, Penard-Morand C, Raherison C, Kopferschmitt C, Lavaud F, Caillaud D, Annesi-Maesano I. Long-term exposure to urban air pollution measured through a dispersion model and the risk of asthma and allergy in children. Bull Acad Natl Med. 2009; 193:1317–1328.
25. Weichenthal S, Dufresne A, Infante-Rivard C. Indoor ultrafine particles and childhood asthma: exploring a potential public health concern. Indoor Air. 2007; 17:81–91.
26. Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, Smith KR. Woodsmoke health effects: a review. Inhal Toxicol. 2007; 19:67–106.
27. Jedrychowski W, Perera F, Maugeri U, Mrozek-Budzyn D, Miller RL, Flak E, Mroz E, Jacek R, Spengler JD. Effects of prenatal and perinatal exposure to fine air pollutants and maternal fish consumption on the occurrence of infantile eczema. Int Arch Allergy Immunol. 2011; 155:275–281.
28. Pénard-Morand C, Charpin D, Raherison C, Kopferschmitt C, Caillaud D, Lavaud F, Annesi-Maesano I. Long-term exposure to background air pollution related to respiratory and allergic health in schoolchildren. Clin Exp Allergy. 2005; 35:1279–1287.
29. Song S, Lee K, Lee YM, Lee JH, Lee SI, Yu SD, Paek D. Acute health effects of urban fine and ultrafine particles on children with atopic dermatitis. Environ Res. 2011; 111:394–399.
30. Alghamdi MA, Shamy M, Redal MA, Khoder M, Awad AH, Elserougy S. Microorganisms associated particulate matter: a preliminary study. Sci Total Environ. 2014; 479-480:109–116.
31. Jenerowicz D, Silny W, Dańczak-Pazdrowska A, Polańska A, Osmola-Mańkowska A, Olek-Hrab K. Environmental factors and allergic diseases. Ann Agric Environ Med. 2012; 19:475–481.
32. Garrett MH, Hooper MA, Hooper BM, Rayment PR, Abramson MJ. Increased risk of allergy in children due to formaldehyde exposure in homes. Allergy. 1999; 54:330–337.
33. Maruo YY, Yamada T, Nakamura J, Izumi K, Uchiyama M. Formaldehyde measurements in residential indoor air using a developed sensor element in the Kanto area of Japan. Indoor Air. 2010; 20:486–493.
34. Hun DE, Corsi RL, Morandi MT, Siegel JA. Formaldehyde in residences: long-term indoor concentrations and influencing factors. Indoor Air. 2010; 20:196–203.
35. Shin SH, Jo WK. Longitudinal variations in indoor VOC concentrations after moving into new apartments and indoor source characterization. Environ Sci Pollut Res Int. 2013; 20:3696–3707.
36. Weisse K, Lehmann I, Heroux D, Kohajda T, Herberth G, Röder S, von Bergen M, Borte M, Denburg J. The LINA cohort: indoor chemical exposure, circulating eosinophil/basophil (Eo/B) progenitors and early life skin manifestations. Clin Exp Allergy. 2012; 42:1337–1346.
37. Farrow A, Taylor H, Northstone K, Golding J. Symptoms of mothers and infants related to total volatile organic compounds in household products. Arch Environ Health. 2003; 58:633–641.
38. Li WM, Lee SC, Chan LY. Indoor air quality at nine shopping malls in Hong Kong. Sci Total Environ. 2001; 273:27–40.
39. Yoshida T, Ogawa M, Goto H, Ohshita A, Kurose N, Yokosawa F, Hirata M, Endo Y. Clinical findings of the patients with sick building syndrome and the results of environmental measurement. Sangyo Eiseigaku Zasshi. 2011; 53:25–32.
40. Chuard C. Pet-associated infections. Rev Med Suisse. 2009; 5:1985–1990.
41. Chapman JA. Stachybotrys chartarum (chartarum = atra = alternans) and other problems caused by allergenic fungi. Allergy Asthma Proc. 2003; 24:1–7.
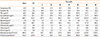
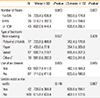
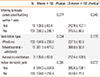
 P<0.05,
P<0.05,  P<0.1,
P<0.1,  P<0.15. PM, particulate matter; CO2, carbon dioxide; CO, carbon monoxide; NO2, nitrogen dioxide; TVOC, total volatile organic compound.
P<0.15. PM, particulate matter; CO2, carbon dioxide; CO, carbon monoxide; NO2, nitrogen dioxide; TVOC, total volatile organic compound.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download