Abstract
Background
This study compares the clinical and radiological results of three most commonly used dynamic stabilization systems in the field of orthopedic surgery.
Methods
A total of 71 patients underwent single-level posterior transpedicular dynamic stabilization between 2011 and 2014 due to lumbar degenerative disc disease. Three different dynamic systems used include: (1) the Dynesys system; (2) a dynamic screw with a PEEK rod; and (3) a full dynamic system (a dynamic screw with a dynamic rod; BalanC). The mean patient age was 45.8 years. The mean follow-up was 29.7 months. Clinical and radiological data were obtained for each patient preoperatively and at 6, 12, and 24 months of follow-up.
Results
Clinical outcomes were significantly improved in all patients. There were no significant differences in the radiological outcomes among the groups divided according to the system used. Screw loosening was detected in 2 patients, and 1 patient developed screw breakage. All patients with screw loosening or breakage underwent revision surgery.
Lumbar degenerative disc disease (DDD) is very common among the middle-aged and older populations. An intervertebral disc cannot repair itself because of a lack of blood supply; therefore, DDD shows a progressive course.12) DDD occurs due to multiple epidemiological factors, such as aging, chronic minor trauma due to bipedal positioning and genetics. Compression of the nerve root, irritation of chemical substances originating from the disc space, and subsequent spinal instability cause low back pain and/or radiating hip and radicular leg pain. The pain occurs due to degeneration of vertebral endplates, the annulus of the intervertebral disc and facet joints.2) Numbness and motor weakness are also common in DDD. In the case of resistant pain and/or neurologic worsening that occurs under medical treatment and physiotherapy, surgery should be considered.
Simple decompression has traditionally been used for single-level DDD; however, the progressive nature of DDD and the subsequent spinal instability that occurs have led surgeons to search for other procedures. During the last 4 decades, thousands of articles have been published regarding fusion surgery for lumbar DDD with the aim of preventing painful motion segments. Although successful results have been reported for fusion procedures, long-term complications, such as pseudoarthrosis, implant breaking or loosening and adjacent segment disease (ASD), can still occur. Furthermore, patient clinical satisfaction is not always compatible with satisfactory postoperative radiological findings.2)
Dynamic stabilization of the lumbar spine has been performed for 20 years with the purpose of either preventing the loading of the intervertebral disc and facet joint or securing the physiological segmental motion of the spine.2) Following its first use by Graf,3) many different techniques and materials for dynamic stabilization have been proposed. Transpedicular dynamic stabilization is the most preferred method performed by spine surgeons. There are several pedicle-based systems to stabilize the spine while allowing limited movement without fusion. It is a common practice to use hinged screws or dynamic rods separately; however, at Koc University Hospital, either semirigid systems or full dynamic systems are used in patients with single-level lumbar DDD. The aim of this study was to investigate the clinical and radiological results of posterior transpedicular single-level dynamic stabilization using 3 different dynamic stabilization systems.
Patients with severe low back pain due to DDD who were unresponsive to conservative treatment and physiotherapy were included in the study. The diagnosis of DDD was based on clinical findings and lumbar magnetic resonance imaging (MRI) examinations. Severe low back pain and a single-level black disc with or without a high intensity zone exhibited by MRI was considered indicators of lumbar DDD. A total of 71 patients (32 females and 39 males) were included in the study. The patients with DDD who presented with radiculopathy were included in this study. All of these patients suffered from painful attacks for a long time before radicular findings.
All patients underwent single-level posterior transpedicular dynamic stabilization between 2011 and 2014. Different dynamic systems were used: (1) the Dynesys system (n = 23; Zimmer Spine, Memphis, TN, USA); (2) the dynamic screw (hinged screw) with a PEEK rod system (n = 31; CD–Horizon Legacy, Medtronic Sofamor Danek, Memphis, TN, USA); and (3) the full dynamic system (a hinged screw with a dynamic rod [BalanC]) (n = 17; CD–Horizon BalanC; Medtronic Sofamor Danek). The patients were randomly given one of the systems, not based on a systematic selection criteria. The mean age of the patients was 45.8 years (range, 19 to 88 years); 43.6 years for the Dynesys group; 44.0 years for the dynamic screw and PEEK rod group; and 51.8 years for the full dynamic group. The mean follow-up time was 29.7 months. Data for each system are presented in Table 1.
DDD causes segmental instability and occurrence of pain is the ultimate result in those patients. The objective of the study was not to compare the 3 different systems but to investigate the effectiveness of dynamic stabilization designed to prevent over-motion in an unstable segment while allowing limited motion of the spine in DDD patients. Since the 3 different systems were used in the patients for the same purpose, there were no differences in indications.
The visual analogue scale (VAS) and Oswestry Disability Index (ODI) scores were assessed in each patient preoperatively and at 6, 12, and 24 months of postoperative follow-up, respectively. The VAS and ODI scores were compared among groups at each follow-up period (Table 2). Statistical analyses were performed using the Wilcoxon signed-rank test, and p < 0.05 was considered to be significant (Table 2).
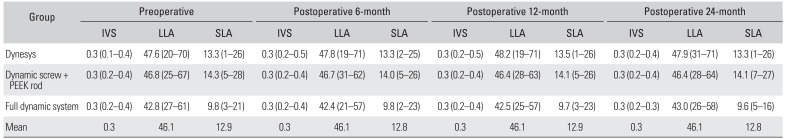
Anteroposterior (AP) and lateral standing radiograms of each patient's lumbar spine were obtained preoperatively and postoperatively at 6, 12, and 24 months of follow-up, respectively. The intervertebral space (IVS) ratio, lumbar lordosis angle (LLA), and segmental lordosis angle (SLA) were measured and the mean values of each group were statistically compared (Table 3 and Fig. 1).
All operations were performed under general anesthesia in the prone position. Following a 3–4 cm midline skin incision, the fascia was opened approximately 3 cm lateral to midline on both sides. The placement of screws was performed using the transmuscular approach with C-arm fluoroscopy guidance. The operation levels of patients were as follows: L2–3 (n = 2), L3–4 (n = 6), L4–5 (n = 42), and L5–S1 (n = 21).
The operation durations ranged between 45 and 90 minutes. No more than 300 mL of blood loss was detected. Neither mortality nor morbidity occurred during the perioperative period. The same operation was performed for all of the dynamic systems used (Dynesys, PEEK roddynamic screw, and full dynamic system [BalanC]) (Figs. 2, 3, 4).
The mean hospital stay was 3.4 days (range, 2 to 8 days). The mean follow-up period was 29.7 months (30.2 months for the Dynesys group; 30.6 months for the dynamic screw and PEEK rod group; and 28.3 months for the full dynamic group). The VAS and ODI scores decreased in the early postoperative period and kept decreasing at 6, 12, and 24 months of follow-up, respectively.
The mean preoperative VAS and ODI scores for the Dynesys group were 7.3 and 67.7, respectively. The mean VAS and ODI scores decreased to 3.2 and 29.5, respectively, at 6 months of follow-up; 2.4 and 14.0, respectively, at 12 months of follow-up; and 2.0 and 12.8, respectively, at 24 months of follow-up. The decrease at each time point was statistically significant (p < 0.05).
The mean preoperative VAS and ODI scores for the dynamic screw and PEEK rod group were 7.1 and 61.8, respectively. The mean VAS and ODI scores decreased to 3.0 and 29.7, respectively, at 6 months of follow-up; 2.3 and 15.4, respectively, at 12 months of follow-up; and 1.7 and 12.8, respectively, at 24 months of follow-up. The decrease at each time point was statistically significant (p < 0.05).
The mean preoperative VAS and ODI scores for the full dynamic group were 7.2 and 66.4, respectively. The mean VAS and ODI scores decreased to 2.5 and 23.7, respectively, at 6 months of follow-up; 2.2 and 14.9, respectively, at 12 months of follow-up; and 1.9 and 12.8, respectively, at 24 months of follow-up. The decrease at each time point was statistically significant (p < 0.05).
The preoperative mean IVS ratio, LLA, and SLA for the Dynesys group were 0.3, 47.6, and 13.3, respectively. The postoperative findings for each measurement were not significantly different when compared with the preoperative values (Table 3).
The preoperative IVS ratio, LLA, and SLA for the dynamic screw with PEEK rod method were 0.3, 46.8, and 14.3, respectively. The postoperative values were not significantly different from the preoperative values (Table 3).
The preoperative IVS ratio, LLA, and SLA for the dynamic screw with the dynamic rod (BalanC) method were 0.3, 42.8, and 9.8, respectively. As in the other groups, the postoperative radiological outcome was not significantly different from the preoperative values (Table 3).
Neither misplacement of the screws, pseudomeningocele, hematoma, neurological worsening nor impaired wound healing were detected in any of the patients; therefore, no early interventions were required. No patient had a second surgery due to ASD. Postoperative infection was observed in 3 patients (4.2%), and all infected patients were treated with long-term antibiotic administration.
Screw loosening was observed in 2 patients, one in the Dynesys group and the other in the dynamic screw and PEEK rod group. The patient in the Dynesys group had screw loosening 1 year after instrumentation at the L5–S1 level. The patient in the dynamic screw and PEEK rod group had screw loosening at 2 years after instrumentation at the L4–5 level. There was also one screw breakage in the Dynesys group at the L4–5 level with L4 screw breakage at 30 months after operation. All patients with screw loosening or breakage underwent revision surgery.
One patient in the Dynesys group presented with an L1 vertebra fracture because of falling; however, the L5–S1 screws and spacers remained intact. This patient underwent an L1 kyphoplasty procedure.
Lumbar spine stabilization is a major concern while managing lumbar DDD because pain, the most common symptom, is the result of segmental instability.4) Although fusion surgery is performed with the goal of stabilization, ASD and pseudoarthrosis may result in an unstable condition at the end.5)
Graf3) reported on the first lumbar spine dynamic stabilization procedure in 1992. Various methods and systems have been used with the aim of stabilizing the vertebral column without fusion, which is often called motion preservation surgery. Total disk replacement, replacement of nucleus, total facet replacement, interspinous devices, and screw-rod systems are commonly used for dynamic stabilization.
Transpedicular dynamic stabilization is a common neurosurgery practice. The effects of ligament systems (Graff [Sem Co., Montrouce, France] or Dynesys), semirigid systems (combining a dynamic rod and a rigid screw or a rigid rod and a dynamic screw), and full dynamic systems (combining a dynamic [hinged] screw and a dynamic rod) were determined. In our institution, either the Dynesys system, a dynamic screw with a PEEK rod, or a dynamic screw with a dynamic rod (BalanC) have been used.
Dynamic stabilization procedure is performed with the purpose of reducing movement at an unstable motion segment without fixing it. So dynamic systems enable physiologic movement of functional segment units within the limits of neutral zone.
Several studies have reported that physiological movements and load carrying function after posterior dynamic stabilization lead healing of disk tissue; thus, rehydration begins even in patients with DDD.678) DDD is a well-known pathology that causes one level or multilevel segmental instability. Most DDD patients have only back pain without neurologic deficit. Pain comes from abnormal movement of a functional segment due to the degenerated disc. Biomechanical studies showed that even dynamic rod and dynamic screw restore loose neutral zone.910) However, posterior dynamic stabilization of patients with a black disk is more likely to reach fusion; therefore, those systems may provide a better quality of life by limiting microinstability while fusion occurs.
The Dynesys system is the most common system for lumbar dynamic stabilization worldwide. Recent reports have shown that the Dynesys system normalizes the neutral zone and controls pathological movements.11) Successful outcomes of the Dynesys system led to the recognition of it as an alternative to lumbar fusion.12) The dynamic transpedicular screw was first used in 1992. Although the Cosmic spinal system (Ulrich medical, Ulm, Germany) has been used with the aim of fusion of the lumbar spine, it has been shown that successful outcomes are obtained without fusion.131415) Safinaz (Medikon, Ankara, Turkey) is the other common dynamic screw that has been used in Turkey. This screw allows up to 20° of flexion–extension and 2° of rotation.13) Biomechanics and finite element studies have shown successful results for both types of dynamic screws.913) The PEEK rod (CD–Horizon Legacy; Medtronic Sofamor Danek) is a dynamic connector that is more flexible than titanium. Furthermore, the PEEK rod with a silicon joint (CD–Horizon BalanC; Medtronic Sofamor Danek) has been used as a hybrid system.
Dynamic lumbar stabilization together with dynamic (hinged) screw and dynamic rod is a new concept, which is called full dynamic stabilization. Biomechanically, the most appropriate devices that have better harmony with the posterior tension band of a dynamic rod are hinged screws. The most comparative results to a normal functional segment have been obtained by a full dynamic system in a cadaveric destabilized vertebra study wherein breaking and loosening of screws was shown to be less common because of reduced loading stress.101617)
The incidence of implant failure, such as loosening or breakage, is reported to range between 2.6% and 36% after fusion surgery.18) In our current study, 2 of the 71 patients had screw loosening, and 1 screw breakage was detected. All patients with screw loosening or breakage underwent revision surgery. The broken and loose screws were replaced with larger diameter screws.
Even though ASD can potentially occur in all patients after fusion surgery, the approximate incidence of symptomatic ASD is between 5.2% and 18%.19) In our study, neither clinical nor operable ASD was detected after a mean of 29.7 months of follow-up. However, Schaeren et al.20) has reported that degeneration at adjacent segments was still a problem observed in 26 patients during a 4-year dynamic stabilization follow-up period.
In conclusion, posterior dynamic stabilization is a very effective treatment modality in patients with single-level DDD. Several systems, including hinged screws, dynamic rods and combined systems, have been used with high success rates and can prevent fusion-related complications. The use of a hinged screw-dynamic rod system might be more appropriate due to this method more imitates physiologic spine movements.
References
1. Oktenoglu T, Ozer AF, Sasani M, et al. Posterior dynamic stabilization in the treatment of lumbar degenerative disc disease: 2-year follow-up. Minim Invasive Neurosurg. 2010; 53(3):112–116. PMID: 20809451.

2. Roberts S, Evans H, Trivedi J, Menage J. Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am. 2006; 88(Suppl 2):10–14.

3. Graf H. Lumbar instability: surgical treatment without fusion. Rachis. 1992; 4(2):123–137.
4. Smith D, McMurray N, Disler P. Early intervention for acute back injury: can we finally develop an evidence-based approach? Clin Rehabil. 2002; 16(1):1–11.

5. Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008; 33(15):1701–1707. PMID: 18594464.

6. Fay LY, Wu JC, Tsai TY, et al. Intervertebral disc rehydration after lumbar dynamic stabilization: magnetic resonance image evaluation with a mean followup of four years. Adv Orthop. 2013; 2013:437570. PMID: 23738082.

7. Gomleksiz C, Sasani M, Oktenoglu T, Ozer AF. A short history of posterior dynamic stabilization. Adv Orthop. 2012; 2012:629698. PMID: 23326674.

8. Song JJ, Barrey CY, Ponnappan RK, Bessey JT, Shimer AL, Vaccaro AR. Pedicle screw-based dynamic stabilization of the lumbar spine. Pan Arab J Neurosurg. 2010; 14(1):1–8.
9. Bozkus H, Senoglu M, Baek S, et al. Dynamic lumbar pedicle screw-rod stabilization: in vitro biomechanical comparison with standard rigid pedicle screw-rod stabilization. J Neurosurg Spine. 2010; 12(2):183–189. PMID: 20121354.
10. Oktenoglu T, Erbulut DU, Kiapour A, et al. Pedicle screw-based posterior dynamic stabilisation of the lumbar spine: in vitro cadaver investigation and a finite element study. Comput Methods Biomech Biomed Engin. 2015; 18(11):1252–1261. PMID: 24708377.
11. Wurgler-Hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J. Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine (Phila Pa 1976). 2008; 33(3):E66–E72. PMID: 18303447.
12. Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976). 2005; 30(3):324–331. PMID: 15682014.
13. Strempel A. Nonfusion stabilization of the degenerated lumbar spine with Cosmic. In : Kim DH, Cammisa FP, Fessler RG, editors. Dynamic reconstruction of the spine. New York, NY: Thieme Medical Publishers. Inc.;2006. p. 330–339.
14. Strempel A, Moosmann D, Stoss C, Martin A. Stabilisation of the degenerated lumbar spine in the nonfusion technique with cosmic posterior dynamic system. Wall St J. 2006; 1(1):40–47.
15. von Strempel A, Neekritz A, de Muelenaere P, du Toit G. Dynamic versus rigid spinal implants. In : Gunzburg R, Szpalski M, editors. Lumbar spinal stenosis. Philadelphia, PA: Lippincott Williams & Wilkins;2000. p. 275–285. .
16. Erbulut DU, Kiapour A, Oktenoglu T, Ozer AF, Goel VK. A computational biomechanical investigation of posterior dynamic instrumentation: combination of dynamic rod and hinged (dynamic) screw. J Biomech Eng. 2014; 136(5):051007. PMID: 24599026.

17. Erbulut DU, Zafarparandeh I, Hassan CR, Lazoglu I, Ozer AF. Determination of the biomechanical effect of an interspinous process device on implanted and adjacent lumbar spinal segments using a hybrid testing protocol: a finiteelement study. J Neurosurg Spine. 2015; 23(2):200–208. PMID: 25932601.

18. Mohi Eldin MM, Ali AM. Lumbar transpedicular implant failure: a clinical and surgical challenge and its radiological assessment. Asian Spine J. 2014; 8(3):281–297. PMID: 24967042.

19. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004; 29(17):1938–1944. PMID: 15534420.
20. Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008; 33(18):E636–E642. PMID: 18708915.

Fig. 1
The intervertebral space ratio was measured by dividing half of the sum of the anterior (A) and posterior (B) intervertebral disc heights by the upper vertebral body height (H). The lumbar lordosis (LL) angle was measured as the angle between the superior endplates of L1 and S1. The segmental lordosis (α) angle was measured as the angle created by a line drawn from the superior endplate of the upper vertebra and a line drawn from the inferior endplate of the lower vertebra of the operation segment.
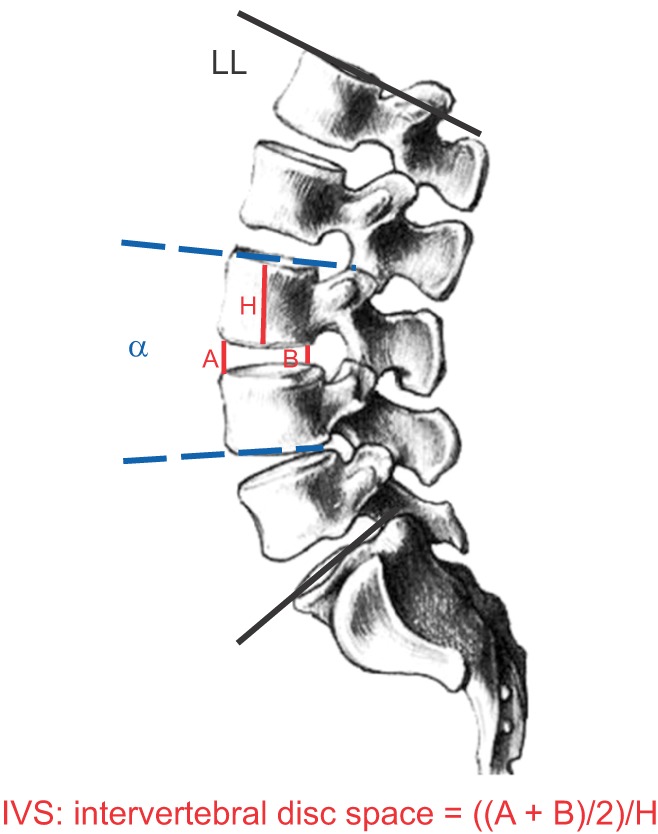
Fig. 2
A 61-year-old female patient complained of back pain and left sciatica. She had an approximate 20-year history of back pain attacks. During the latest attack, she noticed sciatica in her left leg. (A) The T2-weighted sagittal magnetic resonance imaging (MRI) showed spontaneous L5–S1 level fusion (yellow arrow) and herniation at level L4–5 (white arrow). (B) The axial section of T2-weighted MRI showed protrusion of the disc on the left side (white arrow). The lateral direct X-ray (C) and anteroposterior X-ray (D) were taken 2 years after the operation performed using dynamic screws (blue arrows) and a dynamic rod (red arrows) (BalanC; Medtronic Sofamor Danek). Postoperatively, the patient had no complaint of back pain or severe back pain attacks.
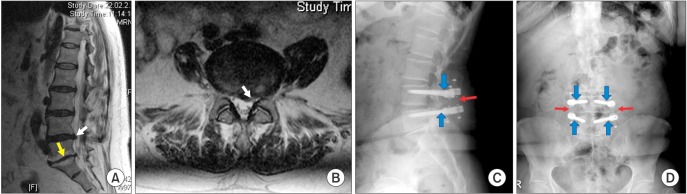
Fig. 3
A 55-year-old male patient had severe back pain and left leg pain. The patient had severe back pain attacks intermittently for 30 years. (A) The T2-weighted sagittal magnetic resonance imaging (MRI) showed lumbar disc herniation at the L4–5 level (arrow). (B) The axial section of T2-weighted MRI showed disc herniation on the left side (arrow). The lateral direct (C) and anteroposterior X-ray (D) show the Dynesys system (Zimmer Spine) used for stabilization in the patient.
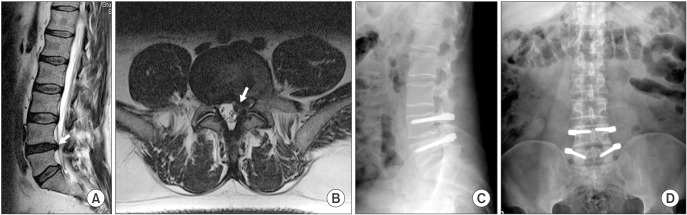
Fig. 4
A 47-year-old female patient had severe back pain attacks for a total of 8 years with 4 severe attacks occurring in the most recent year. Each pain episode lasted 1 week. (A) The T2-weighted sagittal magnetic resonance imaging (MRI) showed herniation at the L4–5 level (white arrow). (B) The axial section of T2-weighted MRI showed midline protrusion at the L4–5 level (white arrow). The lateral direct X-ray (C) and anteroposterior X-ray (D) were taken following stabilization with a dynamic screw and a dynamic PEEK rod (blue arrows) in the patient.
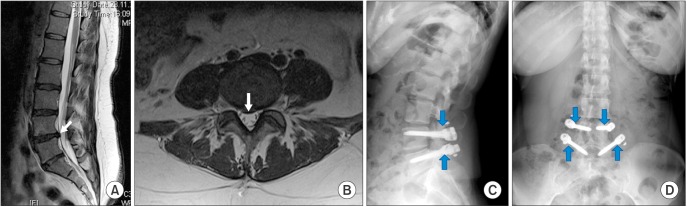
Table 1
Data for Groups with Single-Level Dynamic Stabilization
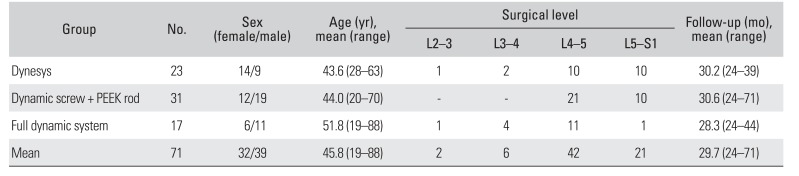
Table 2
Scores of VAS and ODI in All Groups
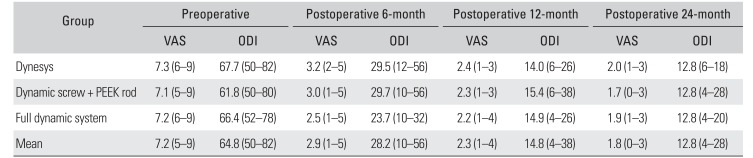
Table 3
Mean Values of Vertebral Parameters of All Groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download