Abstract
Background
The aims of our study were to evaluate the success rate of irrigation and debridement with component retention (IDCR) for acutely infected total knee arthroplasty (TKA) (< 4 weeks of symptom duration) and to analyze the factors affecting prognosis of IDCR.
Methods
We retrospectively reviewed 28 knees treated by IDCR for acutely infected TKA from 2003 to 2012. We evaluated the success rate of IDCR. All variables were compared between the success and failure groups. Multivariable logistic regression analysis was also used to examine the relative contribution of these parameters to the success of IDCR.
Results
Seventeen knees (60.7%) were successfully treated. Between the success and failure groups, there were significant differences in the time from primary TKA to IDCR (p = 0.021), the preoperative erythrocyte sedimentation rate (ESR; p = 0.021), microorganism (p = 0.006), and polyethylene liner exchange (p = 0.017). Multivariable logistic regression analysis of parameters affecting the success of IDCR demonstrated that preoperative ESR (odds ratio [OR], 1.02; p = 0.041), microorganism (OR, 12.4; p = 0.006), and polyethylene liner exchange (OR, 0.07; p = 0.021) were significant parameters.
Infection after total knee arthroplasty (TKA) is a devastating complication that is fortunately rare, occurring in 1% to 2% of primary surgeries.1) Infection types have been classified based on the clinical scenario. Type I infection is defined as a positive intraoperative culture. Type II infection is defined as an early postoperative infection that occurs within the first 4 weeks after primary TKA, which is subdivided into superficial (IIA) and deep (IIB) infections. Type III infection is an acute hematogenous infection, which presents with sudden onset of pain or stiffness in a previously well-functioning arthroplasty. Type IV infection is a late chronic infection with a delayed onset longer than 4 weeks after primary TKA.2) Treatment options for infected TKA include chronic antibiotic suppression,3) irrigation and debridement with component retention (IDCR),4,5) one-stage exchange arthroplasty,6) two-stage exchange arthroplasty,7) and salvage procedures such as resection arthroplasty, arthrodesis, or amputation.8) Of these treatment options, two-stage exchange arthroplasty using an antibiotic-laden cement spacer is considered the gold standard protocol with a high rate of infection control, ranging from 72% to 100%.7,9) However, two-stage exchange arthroplasty has disadvantages such as pain, difficulties in mobility between stages, financial implications, and the potential need for a constrained prosthesis.10) In comparison, IDCR is associated with lower cost and morbidity, retains the primary well-fixed implant, and is a technically less demanding treatment for infected TKA.4,10) However, IDCR has shown lower infection control rates, ranging from 20% to 40% (average, 32%), than component removal treatment.1,8,11,12,13) Many authors have suggested that this procedure is appropriate for treating acute infections developing within 2 days-4 weeks of symptom duration (type II or type III).5,6,9,14,15,16,17,18) However, many of these previous studies did not determine the duration of symptoms within 4 weeks after performing IDCR except for a few studies.5,17,18,19) In addition, there have been few studies that evaluated the parameters affecting the success of IDCR including clinical and laboratory tests.17,20) The aims of our study were to evaluate the success rate of IDCR for acutely infected TKA developing within 4 weeks of symptom duration and to analyze the factors affecting prognosis of IDCR.
We retrospectively reviewed the records of 28 knees (26 patients) surgically treated for infected TKA from 2003 to 2012. Primary TKA was performed in 26 knees at Korea University Medical Center and in 2 knees at other hospitals. The inclusion criteria were as follows: (1) treatment with IDCR (with or without polyethylene liner change); (2) type II or type III infections developing within 4 weeks of symptom duration; (3) absence of established draining sinus tracts and radiographic loosening of the prostheses; (4) more than 2 years of follow-up period; (5) presence of laboratory tests preoperative erythrocyte sedimentation rate (ESR), preoperative C-reactive protein (CRP), preoperative white blood cell (WBC) count and culture result. The diagnosis of acute periprosthetic joint infection was made at the discretion of the operating surgeon based on the following: clinical presentation (painful swelling, skin redness, discharging wound, fever or limited range of motion, discharging sinus), serologic testing (ESR > 30 mm/hr; CRP > 10 mg/L), knee aspiration analysis (polymorphonuclear cell > 20,000 cells/µL), and culture result of the fluid obtained by joint aspiration intraoperatively. Also, all 28 cases in our study satisfied the criteria in "A new definition for periprosthetic joint infection" by Parvizi et al.21)
The treatment was considered to be a failure if the infection was not controlled (persistent symptoms, sustained ESR and CRP elevation), or if repeated irrigation and debridement was performed, or if the implant was replaced with an antibiotic-loaded cement spacer after the IDCR.5) Primary diagnoses for performing primary TKAs were osteoarthritis in 26 knees, rheumatoid arthritis in 1 knee, and Charcot joint in 1 knee. Twenty-three knees were females and 5 knees were males; 28 knees (26 patients), with a mean age at the time of initial treatment for infection of 65.8 ± 8.5 years (range, 42 to 81 years). We have described patient comorbidities in Table 1, which were assessed with the Charlson comorbidity index.11) Additionally, intraoperative tissue cultures were analyzed for acute inflammation and presence of purulence around the implant.4,12) The mean time from primary TKA to the diagnosis of infection was 10.6 ± 19.1 months (range, 0.25 to 79 months). The mean time from symptoms to IDCR was 0.4 ± 0.2 months (range, 0.2 to 1.0 months). The mean follow-up period after IDCR was 40.3 ± 43.1 months (range, 24 to 142 months).
An algorithm for the treatment of infected TKA was not standardized as a result of the retrospective nature of this study. All operations were performed by a single senior surgeon. Thorough open or arthroscopic irrigation and debridement were performed with or without a polyethylene liner change based on the method of debridement (open or arthroscopy). When we performed open debridement, a polyethylene liner change was initiated with total synovectomy, circumferential exposure, and debridement of prosthetic-bone interfaces. When we performed arthroscopic debridement, we did not remove the polyethylene liner. During arthroscopic surgery, anterolateral, anteromedial, posterolateral, and posteromedial portals were used for debridement of all compartments of the knee joint including the posterior compartment. The choice of debridement method was dependent on the patient's general condition and the severity of symptoms. Empiric antibiotics were commenced after joint aspiration or surgical sampling. In general, patients were started on first generation cephalosporins (cefazolin) or vancomycin. Then, they are converted to organism-specific IV antibiotics such as first or third generation cephalosporins (cefazolin, ceftriaxone), ciprofloxacin, vancomycin, and meropenem after the culture results and sensitivity testing were obtained for a minimum of 4 weeks up to 6 weeks. In addition, oral therapy for a longer period of about 8 to 12 weeks was administered with levofloxacin 500 mg and rifampicin 600 mg once per day according to the recommendations of the infectious disease consultant until the ESR and CRP were normalized and the signs of clinical infection disappeared based on previous studies.13,22)
We evaluated the success rate of IDCR. All variables were compared between the success group and the failure group. The time from symptoms of infection to IDCR, the time from primary TKA to the diagnosis of infection, and the time from primary TKA to IDCR, were compared between the success and failure groups using the Wilcoxon rank sum test. Age, preoperative joint fluid WBC count, preoperative ESR, and preoperative CRP were compared using the Student t-test. The categorical variables such as sex (male vs. female), microorganism (methicillin-resistant Staphylococcus aureus/methicillin-resistant S. epidermidis [MRSA/MRSE] vs. other microorganisms), Charlson comorbidity index (0 or 1 vs. 2 to 5), and polyethylene liner change (yes vs. no) were analyzed using the Fisher's exact test. Multivariable logistic regression analysis was used to examine the relative contribution of these parameters to the success of IDCR. All statistical analysis was performed using SAS ver. 9.2 (SAS Institute Inc., Cary, NC, USA). A p-value < 0.05 was considered to be statistically significant.
Seventeen knees (60.7%) were successfully treated without the need for component removal or antibiotic-loaded cement spacer insertion. All of the failure cases (11 cases, 39.3%) required component removal, antibiotic-loaded cement spacer insertion, and then revision TKA after infection control. In 8 cases (28.5%), the causative infecting organism was not detected. The most commonly detected organisms were sensitive S. aureus (MSSA, 2 cases; MRSA, 6 cases) and sensitive S. epidermidis (MSSE, 1 case; MRSE, 5 cases) (Table 2). Between the success and failure groups, there were significant differences in the time from primary TKA to IDCR, the preoperative ESR, the microorganism, and the polyethylene liner change. The mean time from primary TKA to IDCR in the success group (8.1 ± 14.0 months) was shorter than that in the failure group (28.2 ± 50.8 months; p = 0.021). The mean preoperative ESR in the success group (69.1 ± 35.5 mm/hr) was lower than that in the failure group (103.5 ± 43.7 mm/hr; p = 0.021). There was a significantly more number of MRSA/MRSE in the failure group than in the success group (p = 0.006). In addition, there were significantly more instances of polyethylene liner change in the success group than in the failure group (p = 0.017) (Table 3). Multivariable logistic regression analysis of parameters affecting the success of IDCR demonstrated that preoperative ESR (odds ratio [OR], 1.02; p = 0.041), microorganism (OR, 12.4; p = 0.006), and polyethylene liner change (OR, 0.07; p = 0.021) were significant parameters (Table 4). Multicollinearity in continuous variables was defined as variance inflation factor > 10, and there was no significant multicollinearity among these variables (data not shown). For the categorical variables, κ-statistics was utilized to confirm that there is no collinearity. We assumed that a high κ-value near 1 indicates great agreement, collinearity, between the two categorical variables. Among the categorical variables, all κ-values were < 0.1, which indicates the least agreement between two categorical variables.
The principal findings of our study were that 60.7% (17/28) of the knees were successfully treated without the need for component removal or antibiotic-loaded cement spacer insertion, and the preoperative ESR, microorganism, and polyethylene liner change were the factors that affected the success of IDCR for acutely infected TKA developing within 4 weeks of symptom duration. Many studies reported that the success rate of IDCR for infected TKA ranged from 20% to 40%.5,6,9,14,15,16,17,18,19,20,23) Our results showed a relatively higher success rate compared to previous studies. Most of these studies on IDCR were performed without limitations on the duration of symptoms of infection. However, some studies evaluated the results in acute infections developing within 4 weeks.5,17,18,19) In addition, there have been few studies that evaluated the parameters affecting the success of IDCR including clinical and laboratory tests.17,20) Of the many factors that should be considered in the treatment of acutely infected TKA, symptom duration has been suggested to be the most important factor.14,15,23,24) The reported success rates for treating deep infection of TKA by IDCR are 26% to 84% for acute infections and 0% to 19% for late chronic infections.12,15,16,23) Therefore, it would be meaningful to evaluate the results of IDCR in acute infections of TKA according to the recommended indications of IDCR. However, even in studies performed in acutely infected TKA, the success rate was variable (16% to 73%).5,17,18,19) These variations in the success rate of IDCR can also be explained by other factors such as definition of infection, complex antibiotic regimen, and differing criteria for failure of treatment.25)
In many studies, the control of infection with IDCR was traditionally linked to various factors including age, gender, symptom duration, host comorbidity, thoroughness of debridement, virulence of the organism, timing of the infection in relation to the original surgery, presence of the sinus tract, polyethylene liner exchange, and well-fixed components with no radiologic evidence of loosening.4,9,14,15,16,18,23,24) Of these factors, symptom duration has been suggested to be the most important factor,15,23) and symptom duration of less than 4 weeks is associated with success of IDCR.6,9,15) Some studies on IDCR performed within 4 weeks of symptom duration reported a success rate of 16% to 73%.7,23,25,26) In the present study, we treated acute cases developing within 4 weeks of symptom duration; however, the mean time from symptoms of infection to IDCR was less than 2 weeks (0.4 months). This could be one of the reasons for our relatively high success rate (60.7%). However, the effect of symptom duration of less than 4 weeks, which defines the effect of acute infection on the outcome of IDCR, is controversial, and the available evidence is limited.9,15,23,24) In addition, the definition of 'acute' is nebulous and it is also difficult to accurately define the onset of symptoms based on the patient history.19) This could be one of the reasons for variable results after IDCR in acutely infected TKA.
In the present study, the mean time from primary TKA to IDCR in the success group was significantly shorter than that in the failure group. Teeny et al.9) suggested that the recurrence rate after IDCR was high in infections identified at more than 2 weeks after primary TKA, and in late infections, it was difficult to know whether the infection is of an acute hematogenous origin or a flare of a long-term low-grade infection. Silva et al.6) in their literature review also suggested that early postoperative infection was one of the factors associated with successful IDCR. Therefore, to increase the success rate of IDCR, it would be better to consider IDCR in cases of early postoperative infection. In the present study, the mean time from primary TKA to IDCR in the success group was 8.1 ± 14.0 months, which was longer compared to that in previous studies. The reason for this result was that we not only included cases of early postoperative infection (< 4 weeks) but we also included cases of acute hematogenous infection in previously well-functioning TKA (< 4 weeks of symptom duration).
In our study, the preoperative ESR was one of the factors affecting the success of IDCR. Similar to our study, Kuiper et al.20) demonstrated that ESR at presentation above 60 mm/L was one of the factors associated with the result of IDCR. Although CRP and ESR are the markers to diagnose TKA infection, the predictive abilities of these serologic markers for the success of treatment of TKA infection have not been deeply evaluated. Because the levels of these markers undergo characteristic elevations following an inflammatory insult in a kinetic fashion, it is possible that they may be used as proxies for the duration of infection.26) However, Stryker et al.17) reported that no role exists for them in predicting outcomes of IDCR for the treatment of acute hematogenous TKA infection. They also stated that no reliable correlation seems to exist between duration or severity of infection and their levels, despite the kinetic fashion in which CRP and ESR act.17) Therefore, it seems that there is no consensus on the predictive value of these serologic markers. More studies including more number of cases are needed.
In the present study, we reported that the mean age of patients in the success group tended to be greater than that of patients in the failure group. Theoretically, younger patients should have more robust immune systems to defend against infections. In a previous study, Schoifet and Morrey14) suggested that IDCR was significantly less successful in controlling infections in older patients. On the contrary, Stryker et al.17) reported that patients who failed were younger, on average than those who were successfully treated, which is similar to our result. They described that their finding was somewhat counter-intuitive and might reflect a blunt immune response which predisposed young patients to treatment failure.17) However, in many other studies, authors have reported that age did not influence the risk of failure.9,12,18,24) The reason for this variation could be that other more powerful factors affecting the success of IDCR differed between studies, and age was not a dependent variable.
In the present study, there was a significant difference in the number of resistant microorganisms (MRSA/MRSE) between the success and failure groups. Many previous studies have reported that virulence of the microorganism was one of the risk factors for the failure of IDCR.5,6,14,15,16,18) Bradbury et al.19) reviewed 19 cases of acute periprosthetic MRSA infection managed by IDCR and suggested that the total success rate of IDCR in acute periprosthetic infection (< 4 weeks) was only 18%. In their systematic review, Silva et al.6) reported that antibiotic-sensitive Gram-positive organisms were one of the factors associated with the success of open debridement. Therefore, if the cultured microorganism in infected TKA is a resistant microorganism such as MRSA or MRSE, it would be better to cautiously consider a two-stage revision rather than IDCR. Some authors reported an 86% success rate in eradicating MRSA/MRSE periprosthetic infection with 2-stage exchange arthroplasty.27)
We also reported in this study that polyethylene liner exchange was one of the factors affecting the success of IDCR. In the present study, we performed polyethylene liner exchange in cases of open debridement and did not perform polyethylene liner exchange in cases of arthroscopic debridement. This was because the polyethylene liner change seemed to prevent the recurrence of infections by removing microorganisms present between the metal tibial tray and the polyethylene liner. Although arthroscopy has been recommended as a debridement method for infected TKA, the ability to perform satisfactory debridement of proliferative synovitis and the modular implant between the metal tibial tray and the polyethylene liner is limited, carrying with it the risk of scarring from deep periprosthetic infection.28) Waldman et al.29) suggested that only 38% of infected knees were successfully treated using arthroscopic debridement and recommended the use of open debridement for infected TKA.
This study has some limitations. First, this study was retrospective in nature with a relatively small number of cases. In addition, our cases included arthroscopic debridement without polyethylene liner change and open debridement with polyethylene liner change. This was not a comparative study. Second, the timing, choice, and administration of antibiotics were co-managed with the infectious disease consultant without a standardized protocol. Therefore, we could not analyze antibiotic use due to individualization of treatment regimen according to culture results and patient co-morbidities. Third, selection bias exists since we performed IDCR in only acute cases (< 4 weeks). However, this can also be an advantage as the recommended indication for IDCR is acute infection developing within 4 weeks.14,15,23,24) Fourth, we were not able to report the clinical or functional results and we only reported the success rate of the IDCR procedure.
In conclusion, 60.7% of the cases (17/28) were successfully treated with IDCR for acute TKA infection developing within 4 weeks. The preoperative ESR, microorganism, and polyethylene liner change were the factors that affected the success of IDCR for acute TKA infection. After considering these factors, IDCR with polyethylene liner change would be an effective treatment for TKAs that develop acute infections within 4 weeks.
Figures and Tables
Table 1
Patient Comorbidity and Charlson Comorbidity Index*

Table 2
Microbiologic Evaluation
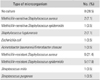
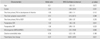
Table 3
Comparison of Variables between the Success and Failure Groups after IDCR

Values are presented as mean ± standard deviation (range) or number (%).
IDCR: irrigation and debridement with component retention, TKA: total knee arthroplasty, WBC: white blood cell, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, MRSA: methicillin-resistant Staphylococcus aureus, MRSE: methicillin-resistant S. epidermidis.
Table 4
Multivariable Logistic Regression Analysis for Evaluating the Relative Contribution of the Variables to the Success of IDCR
References
1. Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010; 468(1):52–56.

2. Tsukayama DT, Goldberg VM, Kyle R. Diagnosis and management of infection after total knee arthroplasty. J Bone Joint Surg Am. 2003; 85:Suppl 1. S75–S80.

3. Trebse R, Pisot V, Trampuz A. Treatment of infected retained implants. J Bone Joint Surg Br. 2005; 87(2):249–256.

4. Sherrell JC, Fehring TK, Odum S, et al. The Chitranjan Ranawat Award: fate of two-stage reimplantation after failed irrigation and debridement for periprosthetic knee infection. Clin Orthop Relat Res. 2011; 469(1):18–25.

5. Choi HR, von Knoch F, Zurakowski D, Nelson SB, Malchau H. Can implant retention be recommended for treatment of infected TKA? Clin Orthop Relat Res. 2011; 469(4):961–969.

6. Silva M, Tharani R, Schmalzried TP. Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res. 2002; (404):125–131.

7. Lee JK, Choi CH. Two-stage reimplantation in infected total knee arthroplasty using a re-sterilized tibial polyethylene insert and femoral component. J Arthroplasty. 2012; 27(9):1701–1706.

8. Ellingsen DE, Rand JA. Intramedullary arthrodesis of the knee after failed total knee arthroplasty. J Bone Joint Surg Am. 1994; 76(6):870–877.

9. Teeny SM, Dorr L, Murata G, Conaty P. Treatment of infected total knee arthroplasty: irrigation and debridement versus two-stage reimplantation. J Arthroplasty. 1990; 5(1):35–39.
10. Leone JM, Hanssen AD. Management of infection at the site of a total knee arthroplasty. J Bone Joint Surg Am. 2005; 87(10):2335–2348.

11. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383.

12. Chiu FY, Chen CM. Surgical debridement and parenteral antibiotics in infected revision total knee arthroplasty. Clin Orthop Relat Res. 2007; 461:130–135.

13. Berbari EF, Marculescu C, Sia I, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007; 45(9):1113–1119.

14. Schoifet SD, Morrey BF. Treatment of infection after total knee arthroplasty by debridement with retention of the components. J Bone Joint Surg Am. 1990; 72(9):1383–1390.

15. Burger RR, Basch T, Hopson CN. Implant salvage in infected total knee arthroplasty. Clin Orthop Relat Res. 1991; (273):105–112.

16. Deirmengian C, Greenbaum J, Lotke PA, Booth RE Jr, Lonner JH. Limited success with open debridement and retention of components in the treatment of acute Staphylococcus aureus infections after total knee arthroplasty. J Arthroplasty. 2003; 18:7 Suppl 1. 22–26.

17. Stryker LS, Abdel MP, Hanssen AD. Predictive value of inflammatory markers for irrigation and debridement of acute TKA infection. Orthopedics. 2013; 36(6):765–770.

18. Gardner J, Gioe TJ, Tatman P. Can this prosthesis be saved?: implant salvage attempts in infected primary TKA. Clin Orthop Relat Res. 2011; 469(4):970–976.

19. Bradbury T, Fehring TK, Taunton M, et al. The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J Arthroplasty. 2009; 24:6 Suppl. 101–104.

20. Kuiper JW, Vos SJ, Saouti R, et al. Prosthetic joint-associated infections treated with DAIR (debridement, antibiotics, irrigation, and retention): analysis of risk factors and local antibiotic carriers in 91 patients. Acta Orthop. 2013; 84(4):380–386.

21. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011; 469(11):2992–2994.

22. Bernard L, Legout L, Zurcher-Pfund L, et al. Six weeks of antibiotic treatment is sufficient following surgery for septic arthroplasty. J Infect. 2010; 61(2):125–132.

23. Brandt CM, Sistrunk WW, Duffy MC, et al. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis. 1997; 24(5):914–919.

24. Hartman MB, Fehring TK, Jordan L, Norton HJ. Periprosthetic knee sepsis: the role of irrigation and debridement. Clin Orthop Relat Res. 1991; (273):113–118.
25. Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997; 12(4):426–433.

26. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999; 340(6):448–454.

27. Mittal Y, Fehring TK, Hanssen A, Marculescu C, Odum SM, Osmon D. Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am. 2007; 89(6):1227–1231.

28. Meneghini RM, Hanssen AD. The infected total knee replacement. In : Scott WN, editor. Surgery of the knee. 4th ed. Philadelphia: Churchill Livingston;2006. p. 1782–1798.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download