Abstract
Background
The purpose of this study was to evaluate the clinical feasibility of an electric nerve stimulator in a lumbar transforaminal epidural block.
Methods
Using an electric nerve stimulator, transforaminal epidural blocks were performed in 105 segments of 49 patients who presented with lower back pain with radiating pain to lower extremities. The contrast medium was injected to delineate the nerve root after positioning an insulated needle at the intervertebral foramen under fluoroscopic guidance. Then, the nerve root was electrically stimulated with the insulated needle to confirm whether or not the same radiating pain was evoked.
Results
Of the 105 foraminal segments, the same radiating pain was evoked at 0.5 mAh in 47 segments (44.8%), at 1.0 mAh in 22 (21.0%), at 1.5 mAh in 3 (2.9%), at 2.0 mAh in 15 (14.3%), at 2.5 mAh in 4 (3.8%), and at 3.0 mAh in 5 (4.8%). No response was observed in 9 segments (8.6%). The fluoroscopy revealed successful positioning of the needle in the patients with an evoked radiating pain over 2.0 mAh. The visual analogue scale (VAS) obtained for pain improved from a mean of 7.5 to 2.7 after the block (p = 0.001). In the 9 cases without response to electrical stimulation, the patients showed an improvement on VAS from 7.8 to 3.4 (p= 0.008) also.
In the treatment of lower back pain accompanied by radiating pain to the leg, the transforaminal epidural block (TFEB) has been widely used as a therapeutic modality as well as a diagnostic tool.1) However, definitive targets for effective TFEB have obtained good results. Two conditions should be considered in terms of definitive targeting. One condition is the proper level. Imaging studies including magnetic resonance image (MRI) or computed tomography (CT) might have been obtained in almost all patients before the nerve root block. However, MRI or CT findings are not always consistent with clinical symptoms. The other condition is an appropriate positioning of the needle. For the visual verification of needle positioning, the fluoroscopy is the most reliable method, which can delineate running of nerve roots by contrast media. However, the fluoroscopy cannot confirm the exact relation with clinical symptoms.
The nerve stimulation of nerve roots can recreate the symptoms in the middle of procedure and can therefore identify the level involved with radicular pain. It is generally accepted that seeking a motor response at low amplitudes increases the chances of success of a nerve block.2) However, how much amplitude is enough has not been adequately determined yet.
Previously, Kim et al.3) reported that the transverse processes under longitudinal view as a ultrasound landmark and the needles of medial branch block to the facet joint could be a promising guidance for the selective nerve root block in the lumbar spine. At that time, physicians were interested in the application of electric nerve stimulator in an ultrasound-guided block to improve a successful needle position. We have tried to use an electric nerve stimulator to improve the success of positioning of the needles in ultrasound-guided TFEB as previous authors have tried as well.4) We designed this study as a preliminary study to set up proper amplitudes for successful TFEB because the seeking amplitude was not well known. The purpose of this study is to evaluate the clinical feasibility of an electric nerve stimulator in a lumbar TFEB.
The patients in this study had visited our hospital for chronic lower back pain with radiating pain to the leg between September 2011 and February 2012. They were diagnosed with lumbar spinal stenosis, based on their medical history, physical examination, radiography, MRI, or CT. Forty-nine patients showed no satisfactory improvement of symptoms following medication, physical therapy and rehabilitation programs for more than 6 weeks (Table 1). All of these 49 patients were provided with an explanation of the purpose for this study. They were also advised of the associated risks and given the choice as to whether or not they wanted to participate. Then an informed consent was obtained. Twenty-five males and 24 females with a mean age of 64.7 years (range, 27 to 89 years) were included in the study. TFEBs using an insulated needle for electric nerve stimulation (Fig. 1) were performed at 105 foraminal segments based on clinical symptoms and radiological pathology, including foraminal stenosis on MRI or CT.
During the procedure, patients were placed in a prone position and the lumbar lordotic curve was countervailed. The procedure was utilized by a single operator for all cases. The fluoroscope was positioned so that an appropriate posteroanterior view was obtained. Local anesthetic infiltration was carried out with a 25-gauge needle infiltrating 1% lidocaine, not to exceed approximately 1 mL per level at the lateral edge and slightly inferior to the transverse process. A 22-gauge insulated needle with a stylet was guided towards the neural foramen. Under intermittent fluoroscopy, the needle was advanced into the 'safe triangle',5) inferior to the pedicle and superolateral to the exiting spinal nerve. After positioning the insulated needle at the target foramen and checking detection of blood or cerebral space fluid, 1 mL of contrast medium was injected to assure contrast distribution along the nerve root. Biplanar visualization was carried out in all cases (Fig. 2).
After the positioning of the needle at each level, electrical current was applied through the insulated needle in the same position to evoke the same radicular pain for which the patient wished to undergo TFEB (Fig. 3). As this study was designed to evaluate the relationship between successful lumbar TFEB and the response to electric nerve stimulator, we did not apply the nerve stimulation during inserting the needles to the desired target. After confirming successful TFEB under fluoroscopy, we applied the nerve stimulation with gradually increasing amplitude and checked the amplitude at which a response was observed. Finally, we used a mixture of 1 mL of 2% lidocaine and 1 mL of triamcinolone acetate (40 mg/mL) for the TFEB. All patients took a rest in the recovery room for one hour before leaving the hospital. The clinical assessment for radiating pain was performed by visual analogue scale (VAS) one to three days after the procedure at the outpatient clinic visit. The Wilcoxon signed rank test was used to compare the pre- and post-block VAS. Statistical analysis was carried out using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The statistical significance was set at p < 0.05.
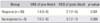
Of the 105 foraminal segments, the same radiating pain was evoked at 0.5 mAh in 47 segments (44.8%), at 1.0 mAh in 22 (21.0%), at 1.5 mAh in 3 (2.9%), at 2.0 mAh in 15 (14.3%), at 2.5 mAh in 4 (3.8%), and at 3.0 mAh in 5 (4.8%). No response was observed in 9 segments (8.6%) (Table 2). The patients evoked the radiating pain over 2.0 mAh and a fluoroscopy revealed the successful positioning of the needle. This result suggests that amplitudes over 2.0 mAh could be used in electrical stimulation for successful TFEB as a safety zone. The VAS for radicular pain improved from a mean of 7.5 to 2.7 after the block (p = 0.001) in patients who had responded to the stimulator (Table 3) and also the 9 cases without response to electrical stimulation showed an improvement on VAS from 7.8 to 3.4 (p = 0.008). No patient experienced any complication such as an aggravation of the pain, numbness, headache, dizziness, or an allergic reaction.
The majority of TFEBs have been distributed at the ventral epidural area. It is possible to provide a high concentration of medicine at a nociceptive target such as the dorsal aspect of the disc herniation. This potentially explains the reasons for significantly better outcomes with lumbosacral transforaminal epidural injections.6)
Electric nerve stimulators are now widely applied as useful aids for nerve blocks.2) There were many studies to establish the relationship between evoked responses and the needle tip-nerve distance.2,7,8) The amplitude of the current needed to produce an evoked response is inversely proportional to the square of the needle tip-nerve distance.2,7) However, "how much amplitude is enough" remains to be determined and this might as well be different for different blocks.9,10) In a selective nerve root block, initiating the amplitude at 0.5 mA seems to be very popular amplitude like the peripheral nerve block. Physicians try to determine the exact amplitude at which an evoked response initiates.11)
In this study, we tried to investigate the proper amplitude to initiate an evoked response of the electric nerve stimulator by examining the relationship between successful TFEB and amplitude of current. The closer the needle positioned to nerve roots, the less amplitude is required and the response of the nerve root block would be more prominent. However, in contrast to a selective nerve root block, the needle has to bypass the nerve root for a successful TFEB. At low amplitudes, there is more chance to sting the nerve which could be produce uncomfortable feeling as the response is evoked when the needle is close to the nerve. In other words, it is not necessary for the end of the insulated needle to be very close to the nerve root in order to conduct a successful TFEB. Pfirrmann et al.12) reported in their cadaveric study that 7 of 30 needles (23.3%) for therapeutic selective nerve root block were located intraepineural, inside the nerve root sleeve. Sato et al.4) found that there was no intraneural pattern in patients who responded to an electrical stimulator. According to our results, even though patients evoked the radiating pain at over 2.0 mAh, radiographs revealed successful positioning of the needle which was confirmed by fluoroscopy. This result suggests a high amplitude over 2.0 mAh could be used as a safety zone in the guidance for a successful TFEB.
This study has some limitations. We applied an electrical nerve stimulator on a fluoroscopy confirmed TFEB. Therefore, the present study findings cannot readily be applied when nerve stimulators are used as supplemental aids in needle positioning of ultrasound-guided TFEB. Although an exact conclusion cannot be drawn from this study, a nerve stimulator can help as a supplemental aid in the successful needle positioning for an ultrasound-guided TFEB at the outpatient department. Further clinical relevant studies are necessary such as application of nerve stimulator in ultrasound-guided TFEB without fluoroscopy in outpatient settings to provide more support for the nerve stimulator.
In conclusion, these results suggest a nerve stimulator can help to predict the success of needle positioning as a supplemental aid for a successful lumbar TFEB. It is enough to initiate proper stimulation amplitude of the nerve at 2 mAh.
Figures and Tables
Fig. 1
An insulated needle for the electric nerve stimulation with two lines: one line is a tube to instill contrast media and medicine, and the other is an insulated electrical line connected to the nerve stimulator device.

Fig. 2
Anteroposterior (A) and lateral (B) radiographs show a successful transforaminal epidural block.

Fig. 3
The nerve stimulator was turned on and the amplitude was increased from 0.5 mAh up to 3 mAh until a response was observed.

References
1. Riew KD, Park JB, Cho YS, et al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five-year follow-up. J Bone Joint Surg Am. 2006; 88(8):1722–1725.
2. De Andres J, Sala-Blanch X. Peripheral nerve stimulation in the practice of brachial plexus anesthesia: a review. Reg Anesth Pain Med. 2001; 26(5):478–483.
3. Kim D, Choi D, Kim C, Kim J, Choi Y. Transverse process marks for ultrasound-guided selective nerve root block. Clin Orthop Surg. 2013; 5(1):44–48.
4. Sato M, Simizu S, Kadota R, Takahasi H. Ultrasound and nerve stimulation-guided L5 nerve root block. Spine (Phila Pa 1976). 2009; 34(24):2669–2673.
5. Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 4th ed. New York: Churchill Livingstone;2005. p. 123–140.
6. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7(2):217–223.
7. Hadzic A, Vloka J, Hadzic N, Thys DM, Santos AC. Nerve stimulators used for peripheral nerve blocks vary in their electrical characteristics. Anesthesiology. 2003; 98(4):969–974.
8. Tulchinsky A, Weller RS, Rosenblum M, Gross JB. Nerve stimulator polarity and brachial plexus block. Anesth Analg. 1993; 77(1):100–103.
9. Choyce A, Chan VW, Middleton WJ, Knight PR, Peng P, McCartney CJ. What is the relationship between paresthesia and nerve stimulation for axillary brachial plexus block. Reg Anesth Pain Med. 2001; 26(2):100–104.
10. Neal JM. How close is close enough? Defining the "paresthesia chad". Reg Anesth Pain Med. 2001; 26(2):97–99.
11. Eeckelaert JP, Filliers E, Alleman JJ, Hanegreefs G. Supraclavicular brachial plexus block with the aid of a nerve stimulator. Acta Anaesthesiol Belg. 1984; 35(1):5–17.
12. Pfirrmann CW, Oberholzer PA, Zanetti M, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness--a study with patients and cadavers. Radiology. 2001; 221(3):704–711.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download