Abstract
Background
The purpose of this study was to report outcomes of congenital hallux varus deformity after surgical treatment.
Methods
We evaluated ten feet of eight patients with a congenital hallux varus deformity, including four feet combined with a longitudinal epiphyseal bracket (LEB). There were seven male patients and one female patient with a mean age of 33 months (range, 7 to 103 months) at the time of surgery. Two patients were bilaterally involved. The mean duration of follow-up was 5.9 years (range, 2.3 to 13.8 years). Clinical outcomes were assessed according to the criteria of Phelps and Grogan. Surgical procedures included the Farmer procedure, the McElvenny procedure or an osteotomy at the first metatarsal or proximal phalanx.
Congenital hallux varus is a rare condition in which the great toe is angled medially at the metatarsophalangeal joint. The varus deformity of the toe can vary in severity from only a few degrees to as much as 90°. The cleft between the great and second toe is usually larger than normal.1) Potential causes of the congenital hallux varus are multifactorial, including: thickened medial cords, medial slopes to the first metatarsocuneiform joints, first metatarsal longitudinal epiphyseal bracket (LEB; delta phalanx), shortened block first metatarsals, space occupying extra metatarsals with the first web spaces and ineffective abductor halluces and adductor hallucis insertions.1,2,3,4,5,6,7)
Surgical correction is generally recommended for congenital hallux varus and various surgical techniques have been described.1,2,4,5,8,9,10) McElvenny11) described the removal of accessory bones, medial sesamoidectomy and capsulotomy, release of the medial fibrous band, reinforcement of the lateral capsule, transfixing of the metatarsophalangeal joint with a Kirschner wire and a partial syndactylization of the first and second toes.10) Farmer1) addressed soft tissue contractures and described a rotational skin flap and syndactylization of the first and second toes. Resection of the entire abductor hallucis muscle and tendon, tenotomy of the abductor hallucis tendon, metatarsal osteotomy and also arthrodesis have been reported.2,5,10) However, most previous studies of outcomes after surgical treatment of congenital hallux varus have been based on a small number of case series or have included several mixed disease cases.1,4,5,8,10,12) Few studies have reported surgical outcomes of several cases with long-term follow-up.5,12) These factors, in addition to the rarity of disease, limit our understanding of this complex deformity.
On the other hand, congenital hallux varus may coexist with other malformations of the foot, such as a LEB of the first metatarsal.2) A LEB is a rare ossification anomaly of tubular bones in which an arcuate secondary ossification center brackets the diaphysis and metaphysis of a phalanx, metacarpal, or metatarsal.3,6,13,14,15,16,17) LEB results in a short, trapezoid-shaped metatarsal, metatarsal angulation and hallux varus if the first metatarsal is involved. Soft tissue correction alone of a congenital hallux varus combined with a LEB of the first metatarsal leads to persistent abnormal growth of the aberrant epiphysis of the first metatarsal, which can be a definite cause of recurrent varus deformity. This concept has been articulated by several authors and various surgical correction techniques for hallux varus associated with a LEB of the first metatarsal have been described.6,13,15,16) In this study, we report outcomes for patients with a congenital hallux varus deformity after surgical treatment.
Totally ten feet of eight patients with a congenital hallux varus deformity were surgically treated at our institute between 1993 and 2008 by the senior author. Indications for surgery were to improve appearance and to enable the wearing of normal shoes.5) There were seven male and one female with a mean age at the time of surgery of 33 months (range, 7 to 103 months). Two patients showed bilateral involvement. Mean duration of the follow-up was 5.9 years after index operation (range, 2.3 to 13.8 years). Six of the patients had hallux varus as an isolated congenital anomaly, while two patients had other anomalies; one had a congenital anterolateral bowing of the tibia on the ipsilateral side, and the other patient had a congenital anterolateral bowing of the tibia and hypoplasia of the second finger on the ipsilateral side.
A preoperative, simple radiograph was used to evaluate the angular deformity, the presence of supernumerary bones or toes and abnormal appearances of the first metatarsal or phalanges, including a LEB. Based on a preoperative radiograph and operative findings, pathological structures in patients reported to be associated with congenital hallux varus deformity by McElvenny11) were described as follows: (1) short, thick metatarsal, (2) accessory bones or toes, (3) varus deformity of one or more of the four metatarsals, and (4) a firm fibrous band extending from the medial side of the great toe to the base of the first metatarsal. Residual varus deformity or recurrence was evaluated by postoperative, simple radiographs and clinical photographs in all patients at follow-up.
Clinical outcomes were assessed according to the criteria of Phelps and Grogan.7) Pain, calluses, residual deformities and scar cosmesis were examined in all patients and the final results were graded as excellent, good or poor. The final result was rated as the most unsatisfactory grade out of the four categories. Furthermore, the patients were asked if they experienced any difficulty in wearing shoes and if they felt that the cosmetic results were satisfactory. The study was approved by our institutional review board.
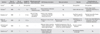
All of the deformities in our patients were associated with one or more of the four components described by McElvenny11) (Table 1). Preaxial polydactyly was present in all patients. Five feet of three patients had been operated to remove polydactyly approximately 12 months after birth at another institute (patients 5, 7, and 8). All remaining five patients had preaxial polydactyly of incompletely duplicated phalanges (type 4 according to Venn-Watson classification7)), although most of the phalanges were poorly formed with little bony contact and arose from the medial border of the foot at the level of the metatarsophalangeal joint.5) These were removed at surgery. A firm fibrous band that extended from the medial side of the great toe to the base of the first metatarsal was also common, present in nine of the ten feet.
A combined LEB was identified in four feet and involved the first metatarsal in three feet (right foot of patient 5 and both feet of patient 7) and the proximal phalanx of the great toe in one foot (patient 8). Interestingly, varus deformities were still present even though all of them had a previous history of surgical removal of polydactyly.
Surgical procedures varied according to the severity of the deformity and the anatomic configuration of the first metatarsal or proximal phalanx (Table 1). Decisions regarding surgical options were individualized, mainly depending on the pathology and severity of the deformity as well as on the age of the patient. A soft tissue procedure, as described by Farmer1) or McElvenny,11) was in isolation performed for three feet (patients 1, 3, and 4) and in conjunction with osteotomy of the first metatarsal or proximal phalanx in four feet. Specifically, a medial open-wedge osteotomy of the first metatarsal was performed for the three feet with a combined LEB of the first metatarsal (right foot of patient 5 and both feet of patient 7), followed by an interposition of an appropriately sized allogenous strut graft (Fig. 1). An osteotomy was performed at the proximal phalanx for the foot with hallux varus combined with a LEB of the proximal phalanx. The Farmer technique was initially performed for patient 6 with a severe deformity, but the varus alignment was not sufficiently corrected. A lateral closing-wedge osteotomy of the first metatarsal was performed for further correction because the first metatarsal was not shortened. After the Farmer technique was performed, the varus deformity was still present in patient 2 with an interphalangeal joint and a severe varus preoperative angulation of 60°. Further correction with a medial open-wedge osteotomy at the proximal phalanx was necessary to achieve a neutral alignment (Fig. 2).
The clinical results were excellent in two feet, good in six and poor in two feet (Table 1). There were no or minimal problems with footwear in all patients. Gross appearances were satisfactory compared with preoperative appearances, although none of the feet could be described as cosmetically normal.5) An unsatisfactory rating was generally related to scar cosmesis. One patient with poor results (patient 5) who had been bilaterally treated was not satisfied due to scar cosmesis of both feet, even though he did not experience pain or footwear problems. The varus deformity was significantly corrected by surgery in all patients. The mean varus angulation of 29.1° at the metatarsophalangeal joint was improved to a mean angle of 4.0° of valgus at follow-up (p < 0.05) (Table 1). Overcorrection was seen in one patient, who had 30° of valgus angulation at follow-up, although he did not complain of pain or difficulties wearing footwear.
A revision surgery was necessary in two patients. One patient (patient 1) with a previous surgery using the Farmer technique complained of a painful bump on the medial aspect of the great toe and persistent widening of the first web space at weight-bearing at year 6 postoperative. Soft tissue procedures were performed to resect the medial skin bump and to narrow the first web space. The patients' outcome was rated as good at the final follow-up. The other patient (patient 3) experienced footwear problems due to shortening of the first ray with mild, residual varus after the Farmer procedure. This patient required a medial open-wedge osteotomy of the first metatarsal and insertion of a strut allograft for further correction 7.5 years postoperative. This patient's outcome was eventually rated as good.
In the current study, congenital hallux varus deformities were treated with various surgical techniques on a case-to-case basis depending on the severity and anatomic characteristics of the deformity. Overall, these techniques yielded favorable results in terms of pain, ability to wear footwear and recurrence of the deformity. Several studies have reported surgical outcomes for congenital hallux varus (Table 2).1,4,5,8,10,12) These studies evaluated patients with mixed diseases or were based on only a few case reports. No uniform method was used to assess clinical outcome and also various surgical procedures were used. This heterogeneity in previous studies, as well as in ours, is most likely not only due to the rarity of congenital hallux varus, but also to the lack of an established, clear definition of the deformity, its underlying pathomechanisms and the surgical treatment of choice for correction.
General guidelines recommend that the issues to be considered for surgery are the correction of a polydactyly if present; correction of the soft tissue tether on the medial side of the foot and the enlarged web space between the great and second toe; correction of a metatarsal-phalangeal incongruity and the correction of a metatarsal or bracket epiphyseal deformity.18) Soft tissue procedure by McElvenny11) or Farmer1) is recommended if the first metatarsal is normal. Also a combined bony deformity, such as a LEB, should be corrected. We followed this guideline in our series and decisions regarding surgical options were based on the pathology and severity of deformity and were individualized for each patient. Mills and Menelaus5) reported surgical outcomes of 20 feet of 12 patients followed-up for an average of 12.7 years. Surgical procedures varied, including McElvenny technique for nine feet, Farmer technique for four, metatarsal osteotomy for two and arthrodesis of the first metatarsophalangeal osteotomy for one foot. The results of soft tissue procedures, such as McElvenny or Farmer technique, and those of arthrodesis were satisfactory, but the metatarsal osteotomy produced unsatisfactory results. They reported that metatarsal osteotomy could cause footwear problems due to varus deformity of the second and third toes or shortening of the first ray. Even amputations of digits were needed to improve the symptoms in their series.5)
In the current study, an osteotomy of the first metatarsal or proximal phalanx was more frequently performed than in that of Mills and Menelaus5) and good to excellent results were yielded in five of seven feet. Specifically, a soft tissue procedure alone was performed in three feet, an osteotomy alone in three and a combined soft tissue procedure and osteotomy in four feet (Table 1). As result, two of three feet with soft tissue procedure alone had revision surgeries (patients 1 and 3) and two of three feet with osteotomy alone had poor clinical outcomes because of unsatisfactory cosmesis (bilateral in patient 5). On the other hand, all of four feet with combined procedures had excellent or good results without any complication or subsequent surgery.
Our study results demonstrated that an osteotomy in conjunction with adequate soft tissue procedure would be a reliable option for the correction of congenital hallux varus. In this series, a soft tissue procedure alone did not provide satisfactory correction and further correction was deemed necessary in case of a combined bony deformity of the metatarsal. We preferably used an opening wedge osteotomy with an interposition of the allograft. This procedure was always combined with physeal bridge resection for a LEB. Our technique, consisting of Farmer technique and opening wedge osteotomy, provided satisfactory correction and good clinical results. We also postulated that an osteotomy plays some role in congenital hallux varus surgery, like described as follows: first, an osteotomy can be used to further correct any residual deformity after the soft tissue procedure. It is possible that varus angulation could remain at the first metatarsophalangeal joint or interphalangeal joint due to the severity and complexity of the deformity, and widening of the first web space could still be present after a soft tissue procedure alone. Widening of the forefoot should be corrected because it can result in difficulties wearing footwear or painful calluses. A lateral closing osteotomy or medial open wedge osteotomy of the first metatarsal can reduce the first and second intermetatarsal angles and cause relief of symptoms. An osteotomy can not only reduce varus angulation, but can also narrow the gap between the first and second toes. Second, a short first metatarsal can be corrected by interposition of a bone graft after osteotomy. Uncorrected shortening of the first metatarsal can cause footwear problems and residual deformities.5) Graft positioning following a medial open-wedge osteotomy may be used for lengthening as well as to reduce varus angulation.8)
LEB involving the first metatarsal is a common cause of hallux varus.2,6,13,15,16) In the current study, it was clear that congenital hallux varus in four feet resulted from a LEB of the first metatarsal or proximal phalanx. All of these feet had a residual hallux varus even after previous removal of polydactyly approximately 12 months after birth.13,14,15,19) Therefore a LEB could not have been considered at the initial surgery until two years of age as it is the time point where the ossification of the proximal and distal ossification centers occurs and it cannot be detected on radiographs before.13,14,15,19) A longitudinal growth of the digit is impossible because the longitudinal bony bracket cannot elongate sufficiently if a LEB is not treatedand the growth occurs in a C-shape along the shortened side of the bone. Bracketing along the medial shaft of the bone probably led to varus deviation with growth in these patients. Sobel et al.13) emphasized that a LEB should not be overlooked when treating pediatric deformities, including congenital hallux varus. We agree that a bracket epiphysis should be suspected if a bone appears short or wide on radiographs in conjunction with one of the known associated anomalies or syndrome.13,19) Diagnostic modalities, including magnetic resonance imaging or ultrasonography, have been shown to be effective in children less than two years of age before the occurrence of ossification of the bracket.14,19)
Numerous surgical procedures to treat a metatarsal LEB have been described; these include bracket chondro-osteotomy accompanied by fat interposition, resection of the LEB with silicone polymer or polymethylmethacrylate interposition, simple bracket excision before ossification, distraction osteogenesis and metatarsal osteotomy after complete closure of the LEB.6,15,16,17,20) The overall goal of any of these procedure is to eliminate the tethering effect of the growth plate by removing the bar and therefore to promote growth in a lengthwise fashion.6,19) We performed a medial open-wedge osteotomy at the diaphysis of the first metatarsal with interposition of an allogenous strut graft to resect the abnormal longitudinal section of the epiphysis, to correct varus angulation and to lengthen the short first metatarsal. Three of four feet with a LEB were sufficiently corrected and showed favorable clinical outcomes using this method. However, in patient 5 (poor results), the varus angulation of the first metatarsal shaft still remained and the longitudinal growth of the first metatarsal was not sufficient at the final follow-up, although the hallux varus did not have a gross physical appearance. The radiographic results of this patient were inferior to those reported by Mubarak et al.21); these authors demonstrated successful longitudinal growth and a normally-shaped metatarsal after central physiolysis for metatarsal LEB.
We reported outcomes after treatment of congenital hallux varus using various surgical techniques. Although the small size of our series precludes a definitive conclusion on the optimal treatment strategy, based on our findings we only regard an osteotomy in conjunction with soft tissue reconstruction as being of importance. Furthermore, patient's age is another factor that must be assessed when considering surgery. As shown in our series, a LEB is one of the causes of the deformity and should be taken into consideration at the initial evaluation. Resection of a bracket epiphysis should be performed as with other procedures to prevent recurrent deformity. We also recommend further evaluation with magnetic resonance imaging or ultrasonography before surgery if the presence of a LEB is in doubt, especially for patients aged two years or less.
Figures and Tables
Fig. 1
Patient 7. (A) Preoperative photograph showing bilateral hallux varus with widening of the first web space. Preoperative scars due to removal of accessory toes are also noted. (B) Preoperative radiograph of the right foot at 58 months of age showing a short thickened first metatarsal, which might result from closure of the physis between the bracket and diaphysis. Radiographs at the immediate postoperative follow-up (C) and at the final follow-up (D).

Fig. 2
Patient 2. (A) Preoperative photograph showing marked medial deviation of the broad great toe and widening of the first web space. (B) Preoperative radiograph showing varus angulation of the first metatarsophalangeal joint and accessory bone of the great toe. (C) Follow-up photograph. (D) Sufficient correction with cosmetically satisfactory appearance of the foot was observed at four years after the Farmer technique and medial open wedge osteotomy at the proximal phalanx. The final result was graded as excellent at 10 years after surgery.

Table 1
Patient Data

LEB: longitudinal epiphyseal bracket, MTP: metatarsophalangeal.
*One of four anatomic components of congenital hallux varus as described by McElvenny: 1) a short, thick metatarsal, 2) accessory bones or toes, 3) varus deformity of one or more of the four metatarsals, or 4) a firm fibrous band that extends from the medial side of the great toe to the base of the first metatarsal.11) The number in parentheses indicates previous history of surgical removal of the accessory bone (component 2).
Notes
References
1. Farmer AW. Congenital hallux varus. Am J Surg. 1958; 95(2):274–278.
2. Herring JA. Tachdjian's pediatric orthopaedics. 4th ed. Philadelphia, PA: Saunders;2008. p. 1172–1173.
3. Light TR, Ogden JA. The longitudinal epiphyseal bracket: implications for surgical correction. J Pediatr Orthop. 1981; 1(3):299–305.
4. Masada K, Tsuyuguchi Y, Kawabata H, Ono K. Treatment of preaxial polydactyly of the foot. Plast Reconstr Surg. 1987; 79(2):251–258.
5. Mills JA, Menelaus MB. Hallux varus. J Bone Joint Surg Br. 1989; 71(3):437–440.
6. Mubarak SJ, O'Brien TJ, Davids JR. Metatarsal epiphyseal bracket: treatment by central physiolysis. J Pediatr Orthop. 1993; 13(1):5–8.
7. Phelps DA, Grogan DP. Polydactyly of the foot. J Pediatr Orthop. 1985; 5(4):446–451.
8. Glickman SH, Cornfield RH. Surgical reconstruction of a congenital foot deformity: hallux varus with brachymetatarsia of the first metatarsal. J Foot Surg. 1990; 29(5):499–503.
9. Joseph B, Jacob T, Chacko V. Hallux varus: a study of thirty cases. J Foot Surg. 1984; 23(5):392–397.
10. Stanifer E, Hodor D, Wertheimer S. Congenital hallux varus: case presentation and review of the literature. J Foot Surg. 1991; 30(5):509–512.
11. McElvenny RT. Hallux varus. Q Bull Northwest Univ Med Sch. 1941; 15:277–280.
12. Thomson SA. Hallux varus and metatarsus varus: a five-year study (1954-1958). Clin Orthop. 1960; 16:109–118.
13. Sobel E, Levitz S, Cohen R, Giorgini R, Jules KT. Longitudinal epiphyseal bracket: associated foot deformities with implications for treatment. J Am Podiatr Med Assoc. 1996; 86(4):147–155.
14. Mahboubi S, Davidson R. MR imaging in longitudinal epiphyseal bracket in children. Pediatr Radiol. 1999; 29(4):259–261.
15. Shea KG, Mubarak SJ, Alamin T. Preossified longitudinal epiphyseal bracket of the foot: treatment by partial bracket excision before ossification. J Pediatr Orthop. 2001; 21(3):360–365.
16. Kucukkaya M, Kabukcuoglu Y, Tezer M, Kuzgun U. Correcting and lengthening of metatarsal deformity with circular fixator by distraction osteotomy: a case of longitudinal epiphyseal bracket. Foot Ankle Int. 2002; 23(5):427–432.
17. Marcdargent Fassier A, Gueffier X, Fraisse T, Janelle C, Fassier F. Longitudinal epiphyseal bracket of the first metatarsus (delta bone). Rev Chir Orthop Reparatrice Appar Mot. 2007; 93(5):486–493.
18. Morrissy RT, Weinstein SL. Lovell and Winter's pediatric orthopaedics. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2005. p. 1306.
19. Schreck MA. Pediatric longitudinal epiphyseal bracket: review and case presentation. J Foot Ankle Surg. 2006; 45(5):342–345.
20. Lampropulos M, Puigdevall M, Zapozko D, Malvarez H. Treatment of first metatarsal longitudinal epiphyseal bracket by excision before closure. J Foot Ankle Surg. 2007; 46(4):297–301.
21. Mubarak SJ, O'Brien TJ, Davids JR. Metatarsal epiphyseal bracket: treatment by central physiolysis. J Pediatr Orthop. 1993; 13(1):5–8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download