Abstract
Background
Currently, an algorithmic approach for deciding treatment options according to the Vancouver classification is widely used for treatment of periprosthetic femoral fractures after hip arthroplasty. However, this treatment algorithm based on the Vancouver classification lacks consideration of patient physiology and surgeon's experience (judgment), which are also important for deciding treatment options. The purpose of this study was to assess the treatment results and discuss the treatment options using a case series.
Methods
Eighteen consecutive cases with periprosthetic femoral fractures after total hip arthroplasty and hemiarthroplasty were retrospectively reviewed. A locking compression plate system was used for osteosynthesis during the study period. The fracture type was determined by the Vancouver classification. The treatment algorithm based on the Vancouver classification was generally applied, but was modified in some cases according to the surgeon's judgment. The reasons for modification of the treatment algorithm were investigated. Mobility status, ambulatory status, and social status were assessed before the fracture and at the latest follow-up. Radiological results including bony union and stem stability were also evaluated.
Results
Thirteen cases were treated by osteosynthesis, two by revision arthroplasty and three by conservative treatment. Four cases of type B2 fractures with a loose stem, in which revision arthroplasty is recommended according to the Vancouver classification, were treated by other options. Of these, three were treated by osteosynthesis and one was treated conservatively. The reasons why the three cases were treated by osteosynthesis were technical difficulty associated with performance of revision arthroplasty owing to severe central migration of an Austin-Moore implant in one case and subsequent severe hip contracture and low activity in two cases. The reasons for the conservative treatment in the remaining case were low activity, low-grade pain, previous wiring around the fracture and light weight. All patients obtained primary bony union and almost fully regained their prior activities.
Conclusions
We suggest reaching a decision regarding treatment methods of periprosthetic femoral fractures by following the algorithmic approach of the Vancouver classification in addition to the assessment of each patient's hip joint pathology, physical status and activity, especially for type B2 fractures. The customized treatments demonstrated favorable overall results.
The prevalence of postoperative periprosthetic femoral fractures is reported to range from 1% after primary hip arthroplasties to 4% after revision hip arthroplasties.1) As a result of the increasing number of hip replacements and increasing expectations regarding mobility in the elderly, it can be expected that the incidence of periprosthetic femoral fractures will continue to increase.
Treatment of these fractures can be challenging in a patient population that typically presents with many comorbidities. However, surgical treatment is often preferred over nonoperative treatment. Osteosynthesis2,3,4) and revision arthroplasty5,6,7) are the options for surgical treatment. Osteosynthesis is challenging owing to the limited space available for screw insertion, because the stem and cement mantle exist in the femoral bone. Previously, fixation of periprosthetic femoral fractures was performed using various compression plates, wires and allografts or a combination thereof 2,3,4) and was then succeeded by the introduction of locking plates. Recently, clinical applications and results of locking plate fixation have been reported.8,9,10,11,12,13,14,15,16)
Periprosthetic femoral fracture treatment decisions depend on five important factors: fracture location, stability of implant and fracture, quality of host bone stock, patient physiology, and surgeon experience.17) Among these five important factors, the first three can be judged by radiographs and are well classified by the Vancouver classification.18) An algorithmic approach for deciding treatment options based on the Vancouver classification is recommended.19) Briefly, type A fractures located at the trochanteric region are mainly treated by conservative means, and surgery is indicated for limited cases only. Type B1 fractures with a well-fixed stem are indications for osteosynthesis among type B fractures located around the stem, while type B2 and B3 fractures with a loose stem are indications for revision arthroplasty. Type C fractures located distal to the stem are treated by ignoring the stem and managing the fracture.
However, the final two important factors, i.e., patient physiology and surgeon experience (surgeon's judgment), are not reflected by the Vancouver classification, but should also be considered when deciding the treatment method. In this study, we retrospectively reviewed a consecutive case series of periprosthetic femoral fractures. We describe the clinical and radiological results and discuss the decision-making process for the treatment options.
Eighteen consecutive cases were retrospectively analyzed, involving seventeen patients with periprosthetic fractures of the femur after total hip arthroplasty (THA) and hemiarthroplasty who were treated in our hospital from July 2005 to May 2012. The study was approved by the Ethics Committee of our institute.
The patient characteristics, treatment methods and clinical results were investigated by reviewing the medical charts. The treatment methods included conservative and surgical treatments. The surgical treatments comprised osteosynthesis and revision hip arthroplasty. Mobility status, ambulatory status, and social status were assessed for all patients before the fracture and at the latest follow-up. Mobility status was assessed using the Parker mobility score.20) Ambulatory status was assessed by five categories: non-ambulatory, with walker, with crutch, with cane, and no aids.15) Social status was assessed by patient autonomy and place of residence and assessed by four categories: at home without support (independent), at home with caregiver support, at hospital, and at nursing home. Operation time, intraoperative bleeding and blood transfusion were assessed for the surgically treated patients. Complications and mortality were assessed for all patients.
The periprosthetic fractures were by reviewing radiographs classified by the Vancouver classification18) and the Johansson classification.21) Diagnosis of loosening was necessary for the Vancouver classification, but difficult for the Austin-Moore hemiarthroplasty stem. Fractures disrupting the three-point fixation of the stem were diagnosed as leading to a loose stem.22) Bony union, loss of reduction, malunion, and implant-related complications were assessed.
One man and sixteen women were included with a mean age (± SD) of 77.9 ± 9.1 years. The previous hip arthroplasty procedures were two cases of cemented THA, four of cementless THA, one of cementless revision THA, six of cementless bipolar hemiarthroplasty, and five of cementless monopolar (Austin-Moore) hemiarthroplasty. The mean duration from hip arthroplasty to periprosthetic femoral fracture was 11.5 ± 12.3 years. The mean follow-up period was 18.4 ± 14.2 months.
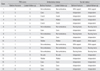
The fractures were classified as one type AG, six type B1, six type B2, and five type C by the Vancouver classification and as ten type I, three type II, and five type III by the Johansson classification. Thirteen fractures were treated by osteosynthesis, two patients by revision arthroplasty, and three patients by conservative treatment. All six type B1, three of six type B2, and four of five type C fractures classified by the Vancouver classification were treated by osteosynthesis. Two cases of type B2 fractures were treated by revision arthroplasty. One case each of type AG, B2, and C fractures were treated by conservative treatment (Table 1).
During the study period, a locking compression plate (LCP) system (Synthes, Tokyo, Japan) was used for all osteosynthesis cases. The LCP cable system was applied to four patients. The used implants were: three narrow LCP, one LCP-distal femur (LCP-DF), three LCP-DF + cable, five reversed LCP-DF, and one reversed LCP-DF + cable (Table 1). All osteosynthesis cases obtained primary bony union. The mean time from surgery to bony union was 4.8 ± 1.8 months. There were no cases with loss of reduction and malunion. There were no severe implant-related complications, such as implant breakage. There was one case of partial screw pull-out in a patient without use of cable fixation in a proximal fragment, although bony union was obtained and the postoperative course was uneventful. Three cases of type B2 fractures were treated by osteosynthesis because of its technical difficulty associated with the performance of revision arthroplasty owing to a severe central migration of an Austin-Moore implant and a subsequent severe hip contracture in one case (case 3) (Fig. 1) and low activity (bedridden or wheelchair-bound with total aid) in two cases (cases 11 and 12) (Table 2).
Two cases with type B2 fractures were treated by revision arthroplasty. One case was an active patient who could walk without aid before the fracture (case 14). The patient was treated by wiring of the fracture site and revision with a cementless longer stem (Fig. 2). The other case demonstrated gross instability of the stem owing to a fracture of a large proximal fragment (case 15). The patient was treated by wiring of the fracture site and revision with a cemented stem. The fracture locations were classified as type I by Johansson classification in both cases. The postoperative courses were uneventful in the revision arthroplasty cases.
The mean operation time was 125.2 ± 54.5 minutes for the osteosynthesis cases and totals of 138 and 150 minutes for the revision arthroplasty cases. The mean intraoperative bleeding was 190.2 ± 177.1 g for the osteosynthesis cases and totals of 535 and 2,470 g for the revision arthroplasty cases. Blood transfusion was performed in four of 13 osteosynthesis cases and one of two revision arthroplasty cases. Autologous blood transfusion was performed in one revision arthroplasty case (Table 1).
One case each of type AG, B2, and C fractures was treated by conservative means. The type C fracture was an incomplete fracture and not accompanied by any displacement (case 16). The type B2 fracture was accompanied by stem sinking, but a conservative treatment was selected because of low activity, low-grade pain, previous wiring around the fracture, and light weight (case 17) (Fig. 3, Table 2). The type AG fracture was not accompanied by displacement and the patient rapidly recovered its activity (case 18).
There were no incidences of infection and intraoperative mortality. There were two cases of early postoperative mortality at 3 and 5 months postoperatively (cases 10 and 13, respectively). Mobility status, ambulatory status and social status were almost the same between before the fracture onset and at the latest follow-up for all patients (Table 3).
The Vancouver classification system is reported to be reliable and valid.23) Currently, an algorithmic approach for deciding treatment options according to the Vancouver classification is widely recommended.19) However, this treatment algorithm based on the Vancouver classification lacks consideration of patient physiology and surgeon experience, which are also important factors for deciding treatment options.17) Park et al.24) suggested custom-tailored treatment according to the general medical condition of the patient in addition to stem stability and fracture configuration. They stated that physicians should not blindly follow the routine management algorithm.
Recently, a locking plate has been applied to the treatment of periprosthetic fractures of the femur after hip arthroplasty and the clinical results have been reported to be satisfactory. Although fixation by a locking plate alone was reported to have limitations, and addition of a cable or wire was recommended in some recent reports,15,16,25) type B1 and C fractures are currently becoming widely treated by locking plate systems. We treated all of our type B1 and C fractures by osteosynthesis using a locking plate system, except of one case with a non-displaced type C fracture and the clinical results were satisfactory. The minimally invasive plate osteosynthesis technique can be applied using a locking plate for applicable cases and allows less surgical stress. Less surgical stress is beneficial, especially in the treatment of elderly patients. There was one case of partial screw pull-out in a patient without use of cable fixation in a proximal fragment, although bony union was obtained and the postoperative course was uneventful. We used reversed LCP-DF in this case, and the short locking screws inserted to the greater trochanter demonstrated a partial screw pull-out. Lag screw fixation maintained the stability although the partial screw pull-out of a neutralization plate was observed. We suggest adding a cable or wire fixation if only short screws can be inserted to the proximal fragment especially for greater trochanter and in cases with very poor bone quality.
Type B2 fractures with a loose stem are recommended for the treatment by revision arthroplasty according to the treatment algorithm based on the Vancouver classification. Although we performed revision arthroplasty for two cases, we selected locking plate fixation for three cases of type B2 fractures. Of these cases, two patients were bedridden with low activity. We suggest that locking plate fixation can restore the mobility and activity of such patients to similar levels to those before the fracture. The performance of revision arthroplasty was accompanied by technical difficulties owing to severe central migration of an Austin-Moore implant and a subsequent severe hip contracture in one patient. Locking plate fixation can be a salvage surgery for such patients and provides satisfactory results. In addition, one patient was treated by conservative means because of low activity, low-grade pain, previous wiring around the fracture, and light weight. Conservative treatment can be applied for patients with such limitations.
A revision arthroplasty was performed in two patients and our experiences with this technique are limited. Intraoperative bleeding occurred in relatively large amounts which could be caused by our limited experiences. Both involved patients were relatively active patients with walking ability. We suggest that active patients with a loose stem present good indications for revision arthroplasty. We further suggest that decisions for a treatment method of Vancouver type B2 periprosthetic femoral fractures should be based not only on the algorithmic approach of the Vancouver classification but also on the assessment of each patient's physical status and activity.
Surgeon experience is also an important factor for deciding treatment options.17) Trauma surgeons are familiar with the management of fractures, but have less experience in managing hip arthroplasty compared with hip joint surgeons. Misinterpretation of the stem stability leading to an inappropriate selection of surgical methods26) can occur with trauma surgeons. In our case series, the preoperative assessment was carried out by both, a trauma surgeon and a hip joint surgeon, and the treatment method was selected after consultation. Osteosynthesis was performed by the trauma surgeon and revision arthroplasty was carried out by the hip joint surgeon. Cooperation of a trauma surgeon and a hip joint surgeon is desirable in the treatment of periprosthetic femoral fractures, if possible.
Patient age is another important factor for the management of a fracture.17) Very advanced age with severe medical comorbidity can be a contraindication for surgery. However, a displaced fracture causes severe pain and makes the patient bedridden. We think that pain relief and avoidance of becoming bedridden are important and that these goals can be achieved through surgical stabilization of a fracture. The authors perform a surgery for patients with surgical indications if it was allowed by an anesthesiologist. Therefore, we do not set a limitation on surgery according to the patient's age. We have experiences of surgery (open reduction and internal fixation) in a 96-year-old woman as our oldest patient.
In summary, we suggest that decisions regarding the treatment method for periprosthetic femoral fractures should be based on the algorithmic approach of the Vancouver classification, in addition to the assessment of each patient's hip joint pathology, physical status and activity, especially for type B2 fractures with a loose stem. Cooperation of a trauma surgeon and a hip joint surgeon is desirable, if possible.
Figures and Tables
Fig. 1
Case 3: An 80-year-old woman. (A) Substantial sinking of an Austin-Moore stem was observed and the fracture was judged to be Vancouver type B2. (B) This patient was treated by an osteosynthesis using a locking plate instead of revision arthroplasty because of technical difficulty of performing revision arthroplasty owing to severe central migration of an Austin-Moore implant and subsequent severe hip contracture. (C) Sixteen months after the osteosynthesis. Bony union was obtained and her previous walking ability was recovered.

Fig. 2
Case 14: A 73-year-old woman. (A) The patient had undergone a cementless total hip arthroplasty on her left hip for treatment of osteoarthritis. (B) A fracture occurred after a fall. Sinking of the stem was observed and the fracture was judged to be Vancouver type B2. (C) Three years after the revision arthroplasty. Wiring and stem revision was performed, and her previous walking ability was recovered.

Fig. 3
Case 17: A 91-year-old woman. (A) Cementless bipolar hemiarthroplasty was performed for treatment of a femoral neck fracture. Wiring was performed at the surgery. (B) A fracture occurred after a fall. Sinking of the stem was observed and the fracture was judged to be Vancouver type B2. (C) Four months after the fracture. Conservative treatment was carried out owing to low activity, low-grade pain, previous wiring around the fracture, and light weight. The previous walking ability was recovered at 1 month after the fracture. Bony union was obtained and the stem sinking never progressed.

References
1. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999; 30(2):183–190.
2. Haddad FS, Duncan CP, Berry DJ, Lewallen DG, Gross AE, Chandler HP. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002; 84(6):945–950.
3. Ricci WM, Bolhofner BR, Loftus T, Cox C, Mitchell S, Borrelli J Jr. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am. 2005; 87(10):2240–2245.
4. Tsiridis E, Narvani AA, Timperley JA, Gie GA. Dynamic compression plates for Vancouver type B periprosthetic femoral fractures: a 3-year follow-up of 18 cases. Acta Orthop. 2005; 76(4):531–537.
5. Macdonald SJ, Paprosky WG, Jablonsky WS, Magnus RG. Periprosthetic femoral fractures treated with a long-stem cementless component. J Arthroplasty. 2001; 16(3):379–383.
6. Park MS, Lee YK, Yang KH, Shin SJ. Management of periprosthetic femoral fractures. J Arthroplasty. 2003; 18(7):903–906.
7. Lee SR, Bostrom MP. Periprosthetic fractures of the femur after total hip arthroplasty. Instr Course Lect. 2004; 53:111–118.
8. Kaab MJ, Stockle U, Schutz M, Stefansky J, Perka C, Haas NP. Stabilisation of periprosthetic fractures with angular stable internal fixation: a report of 13 cases. Arch Orthop Trauma Surg. 2006; 126(2):105–110.
9. O'Toole RV, Gobezie R, Hwang R, et al. Low complication rate of LISS for femur fractures adjacent to stable hip or knee arthroplasty. Clin Orthop Relat Res. 2006; 450:203–210.
10. Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver Type B1 and Type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007; 38(6):725–733.
11. Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant. Arch Orthop Trauma Surg. 2008; 128(4):409–416.
12. Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury. 2008; 39(4):472–479.
13. Ebraheim NA, Gomez C, Ramineni SK, Liu J. Fixation of periprosthetic femoral shaft fractures adjacent to a well-fixed femoral stem with reversed distal femoral locking plate. J Trauma. 2009; 66(4):1152–1157.
14. Bryant GK, Morshed S, Agel J, et al. Isolated locked compression plating for Vancouver Type B1 periprosthetic femoral fractures. Injury. 2009; 40(11):1180–1186.
15. Wood GC, Naudie DR, McAuley J, McCalden RW. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty. 2011; 26(6):886–892.
16. Xue H, Tu Y, Cai M, Yang A. Locking compression plate and cerclage band for type B1 periprosthetic femoral fractures preliminary results at average 30-month follow-up. J Arthroplasty. 2011; 26(3):467–471.
17. Beals RK, Tower SS. Periprosthetic fractures of the femur: an analysis of 93 fractures. Clin Orthop Relat Res. 1996; (327):238–246.
18. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004; (420):80–95.
19. Parvizi J, Vegari DN. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma. 2011; 25:Suppl 2. S77–S81.
20. Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993; 75(5):797–798.
21. Johansson JE, McBroom R, Barrington TW, Hunter GA. Fracture of the ipsilateral femur in patients wih total hip replacement. J Bone Joint Surg Am. 1981; 63(9):1435–1442.
22. Phillips JR, Moran CG, Manktelow AR. Periprosthetic fractures around hip hemiarthroplasty performed for hip fracture. Injury. 2013; 44(6):757–762.
23. Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000; 15(1):59–62.
24. Park SK, Kim YG, Kim SY. Treatment of periprosthetic femoral fractures in hip arthroplasty. Clin Orthop Surg. 2011; 3(2):101–106.
25. Laurer HL, Wutzler S, Possner S, et al. Outcome after operative treatment of Vancouver type B1 and C periprosthetic femoral fractures: open reduction and internal fixation versus revision arthroplasty. Arch Orthop Trauma Surg. 2011; 131(7):983–989.
26. Lindahl H, Garellick G, Regner H, Herberts P, Malchau H. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006; 88(6):1215–1222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download